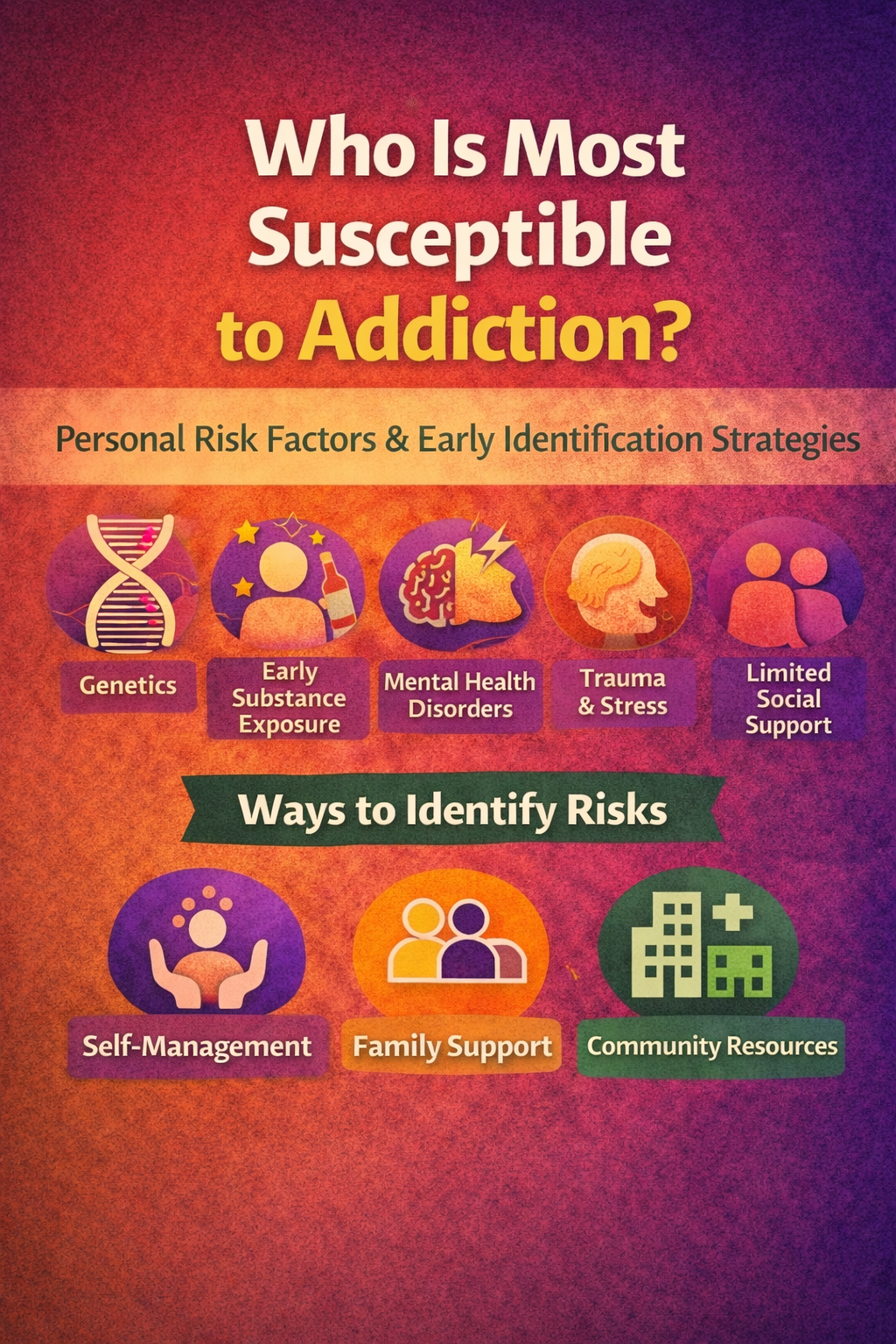
Addiction does not develop in isolation, nor does it affect all individuals equally. Research shows that people with genetic vulnerability, early exposure to substances, untreated mental health conditions, trauma histories, chronic stress, and limited social support are most susceptible to developing addiction. Identifying these risk factors early is critical for prevention and long-term health. Effective identification requires a multi-level approach that includes self-management strategies such as self-awareness and coping skills, family support through education and open communication, and community resources that provide screening, education, and mental health services. When these systems work together, risk factors can be recognized before addiction takes hold, shifting the focus from crisis response to proactive prevention and early intervention.
Who Is Most Susceptible to Addiction? Understanding Risk Factors and Vulnerability
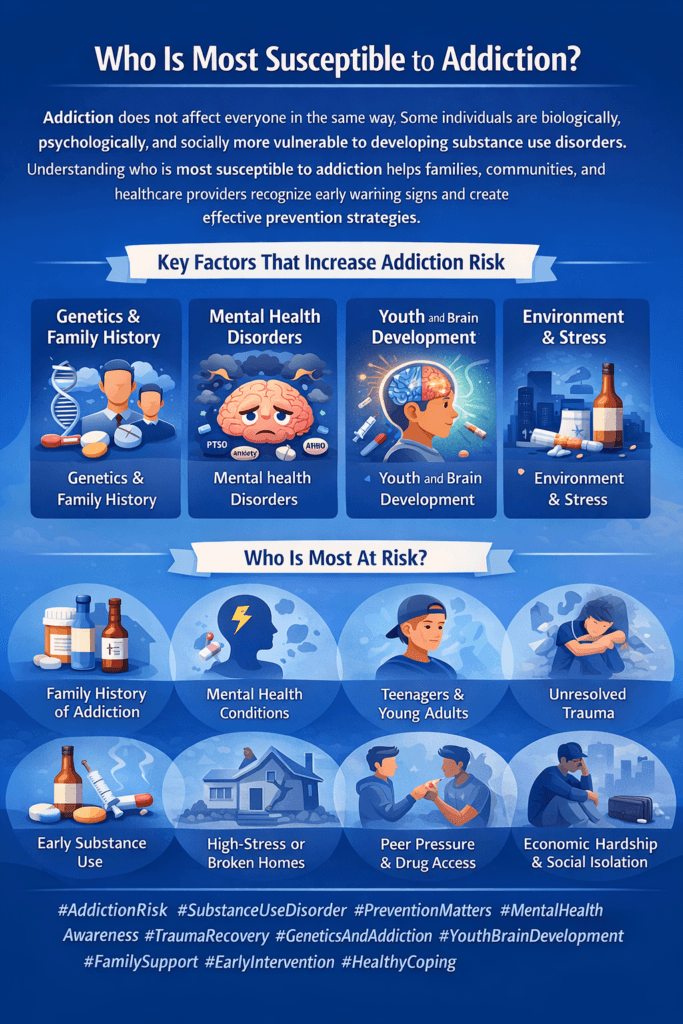
Addiction does not affect everyone in the same way. While anyone can develop a substance use disorder under certain conditions, research shows that some individuals are more susceptible to addiction due to a combination of biological, psychological, and social factors. Understanding who is most vulnerable helps shift the narrative away from blame and toward prevention, early intervention, and compassionate care.
One of the strongest risk factors for addiction is genetics. Family history plays a significant role, as genetic traits can influence how the brain responds to substances, how quickly tolerance develops, and how intensely cravings are experienced. Individuals with close relatives who struggle with addiction are at higher risk, especially when substance use begins early.
Early exposure to substances, particularly during adolescence, greatly increases susceptibility. The adolescent brain continues to develop, particularly in regions responsible for impulse control, decision-making, and emotion regulation. Substance use during this critical period can permanently alter brain development and increase the likelihood of lifelong addiction.
Mental health conditions also increase vulnerability. Individuals with anxiety disorders, depression, bipolar disorder, ADHD, PTSD, or trauma histories may use substances to cope with emotional pain or distress. This pattern of self-medication can quickly evolve into dependence, especially when mental health needs go untreated.
Chronic stress and trauma are major contributors as well. People exposed to abuse, neglect, domestic violence, poverty, or unstable environments are more likely to turn to substances for relief or escape. Trauma changes how the brain processes fear, reward, and stress, increasing addiction risk.
Social and environmental factors further influence susceptibility. Peer pressure, easy access to substances, cultural normalization of substance use, lack of social support, and limited access to healthcare all raise the likelihood of developing addiction. Isolation and stigma can worsen vulnerability by discouraging help-seeking.
Finally, coping skills and resilience play a protective role. Individuals who lack healthy coping strategies or support systems may be more susceptible when faced with stress or adversity.
Addiction vulnerability is not a personal weakness—it is the result of intersecting risk factors. By identifying those most susceptible, communities and healthcare systems can focus on prevention, early support, and targeted interventions to reduce harm and improve long-term outcomes.
Self-Management Strategies to Identify Personal Risk Factors for Addiction
Addiction often develops gradually, influenced by a combination of biological, psychological, and environmental factors. While some risks cannot be changed, many can be recognized and managed early through effective self-awareness and self-management strategies. Identifying personal risk factors enables individuals to take proactive steps to reduce the risk of addiction and support long-term health.
One of the most important self-management strategies is self-reflection. Regularly examining thoughts, emotions, and behaviors helps individuals recognize patterns that may signal increased vulnerability. Noticing when substance use is used to cope with stress, sadness, boredom, or anxiety provides early insight into potential risk.
Tracking behaviors and triggers is another effective approach. Keeping a journal or using digital tracking tools to monitor substance use, cravings, moods, and situations helps identify high-risk environments or emotional states. Over time, patterns such as increased use during stressful periods or social gatherings become clear, allowing for early intervention.
Understanding family history and genetics is also essential. Being aware of relatives with substance use disorders can increase motivation to monitor personal use more carefully and seek preventive support. This knowledge helps individuals make informed choices about substance exposure and limits.
Self-management also includes recognizing mental health warning signs. Symptoms of anxiety, depression, trauma-related stress, or impulsivity can increase addiction risk when left untreated. Seeking mental health support early prevents self-medication patterns from forming.
Another key strategy is assessing coping skills. Individuals who rely on substances to manage emotions may lack healthy coping tools. Learning stress-management techniques such as mindfulness, physical activity, relaxation exercises, and problem-solving skills reduces reliance on substances during difficult moments.
Finally, self-compassion and honesty are critical. Identifying risk factors requires acknowledging vulnerability without self-judgment. Compassionate self-awareness encourages individuals to seek support, set boundaries, and adjust behaviors before addiction develops.
By actively identifying personal risk factors through self-management strategies, individuals gain control over their health and decision-making. Awareness becomes a powerful form of prevention, transforming potential risk into informed, proactive care.
Family Support Strategies to Identify Risk Factors for Addiction
Families play a vital role in recognizing early risk factors for addiction. Because family members often observe changes in behavior, mood, and routines before problems escalate, supportive family involvement can lead to earlier identification and prevention of substance use disorders. When families approach these concerns with understanding rather than judgment, they become powerful partners in prevention and early intervention.
One of the most effective family strategies is open and ongoing communication. Creating a safe environment where conversations about stress, emotions, and substance use can occur without fear of punishment encourages honesty. When individuals feel heard rather than criticized, they are more likely to disclose struggles or risky behaviors early.
Education about addiction risk factors strengthens a family’s ability to identify warning signs. Understanding the role of genetics, mental health conditions, trauma, peer influence, and early substance exposure allows families to recognize vulnerability before addiction develops. Awareness helps families respond with support instead of denial or blame.
Families are often the first to notice behavioral and emotional changes. Shifts in sleep patterns, mood swings, withdrawal from relationships, declining performance at work or school, secrecy, or increased irritability may indicate rising risk. Observing these changes over time provides valuable insight into potential substance-related concerns.
Another important strategy is discussing family history openly. Honest conversations about substance use disorders within the family help normalize caution and reduce stigma. When individuals understand their genetic or environmental risk, they may be more mindful of their choices.
Supporting healthy coping skills also reduces addiction risk. Families can encourage stress management through exercise, hobbies, routines, and emotional expression. Modeling healthy coping strategies for stress teaches protective behaviors.
Finally, families must practice compassionate boundaries. Expressing concern, setting expectations, and offering help without confrontation builds trust. Early support and guidance are far more effective than reacting after addiction has already taken hold.
Through education, communication, observation, and compassion, families can identify addiction risk factors early and help prevent long-term consequences.
Community Resource Strategies to Identify Risk Factors for Addiction
Addiction prevention and early intervention extend beyond individual and family efforts. Communities play a critical role in identifying risk factors for addiction by providing education, screening, and support services that reach individuals before substance use becomes a disorder. When community resources are accessible, coordinated, and stigma-free, risk factors can be recognized early and addressed effectively.
One of the most impactful community strategies is public education and awareness programs. Schools, healthcare systems, nonprofits, and workplaces can provide education on addiction risk factors such as genetics, mental health conditions, trauma, early substance exposure, and social influences. Awareness empowers individuals to recognize their own and others’ vulnerability.
Early screening and assessment services are another essential resource. Primary care clinics, school counselors, mental health providers, and community health centers can screen for substance use risk, mental health concerns, and trauma history during routine visits. Early screening allows for timely referrals and preventive interventions.
Communities also support risk identification through mental health and trauma-informed services. Accessible counseling, crisis intervention programs, and youth support services help identify emotional distress that may lead to substance use as a coping mechanism. Addressing mental health needs early reduces the likelihood of self-medication.
Peer support and mentorship programs further strengthen community response. Youth mentors, recovery coaches, and community advocates with lived experience can recognize early warning signs and provide guidance in relatable, non-threatening ways. Peer connection reduces stigma and increases trust.
Another key strategy involves data-driven public health initiatives. Community health departments track trends in substance use, overdose rates, and social stressors to identify high-risk populations and areas. This information helps target prevention efforts where they are needed most.
Finally, safe access to resources, including housing support, employment assistance, and educational programs, helps address underlying risk factors, such as instability and poverty. Reducing these stressors lowers overall addiction vulnerability.
When communities invest in education, screening, mental health services, and social support, they create protective environments that identify addiction risk early. Prevention becomes a shared responsibility, improving long-term health outcomes for individuals and society.
Frequently Asked Questions
Here are some common questions:
Who is most susceptible to addiction?
Individuals with a combination of genetic vulnerability, early substance exposure, mental health conditions, trauma history, chronic stress, or limited social support are at higher risk.
Does genetics really influence addiction risk?
Yes. Family history can affect how the brain responds to substances, how quickly tolerance develops, and how intense cravings become.
Why does early substance use increase addiction risk?
Using substances during adolescence can disrupt brain development related to impulse control and decision-making, increasing long-term vulnerability.
How do mental health conditions affect addiction risk?
Conditions such as anxiety, depression, ADHD, PTSD, and bipolar disorder can increase risk, especially when substances are used to self-medicate symptoms.
Can trauma and chronic stress lead to addiction?
Yes. Trauma and ongoing stress alter stress-response systems in the brain, making substances more appealing as coping tools.
What social factors increase susceptibility to addiction?
Peer pressure, easy access to substances, social isolation, stigma, and lack of healthcare or community support all increase risk.
How can self-management help identify addiction risk factors?
Self-reflection, tracking moods and behaviors, recognizing triggers, assessing coping skills, and understanding family history help identify personal risk early.
What signs can families look for to identify risk?
Changes in mood, behavior, sleep, social withdrawal, secrecy, declining performance, or increased stress may signal rising vulnerability.
How can families talk about addiction risk without causing conflict?
Using open, non-judgmental communication focused on concern and support encourages honesty and early disclosure.
What role do community resources play in identifying risk factors?
Community education, mental health screening, school counseling, healthcare assessments, and peer programs help detect risk before addiction develops.
Why is early identification of risk factors important?
Early identification allows for prevention and support before substance use escalates into addiction, improving long-term outcomes.
Can addiction risk be reduced once identified?
Yes. Strengthening coping skills, addressing mental health needs, improving support systems, and reducing exposure to substances can significantly lower risk.
Conclusion
Understanding who is most susceptible to addiction allows prevention efforts to focus on awareness rather than blame. When individuals actively monitor their emotional health and behaviors, families provide informed and compassionate support, and communities offer accessible education and screening resources, addiction risk factors can be identified early. This coordinated approach strengthens resilience, reduces vulnerability, and promotes timely intervention. By addressing risk factors before substance use becomes entrenched, individuals and support systems can work together to prevent addiction and foster healthier, more sustainable outcomes.
Video: Who Is Most Susceptible to Addiction