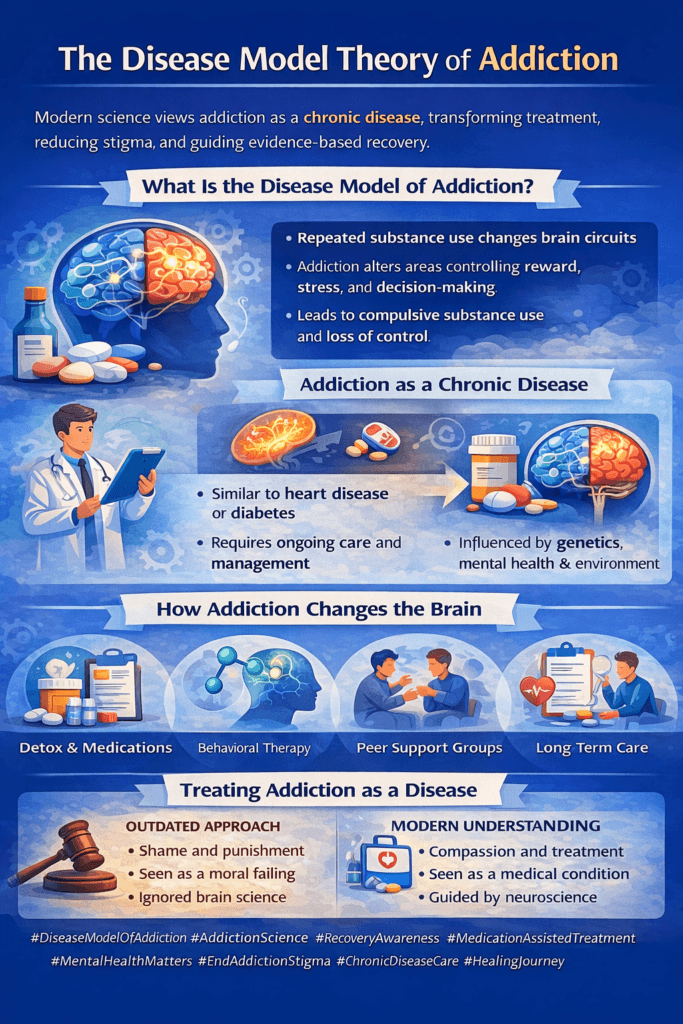
The Disease Model Theory of Addiction explains addiction as a chronic, relapsing medical condition that involves changes in brain structure, function, and behavior. Rather than viewing addiction as a failure of character or willpower, this model recognizes the role of genetics, brain chemistry, mental health, and environmental factors in driving substance use. Understanding addiction through the disease model helps individuals, families, and communities recognize addiction as a health condition that requires treatment, ongoing care, and support—much like other chronic illnesses.
The Disease Model Theory of Addiction: A Medical Perspective on Substance Use
The Disease Model Theory of Addiction views addiction as a chronic, relapsing medical condition rather than a moral failing or lack of willpower. This theory proposes that addiction results from changes in brain structure and function caused by repeated substance use, combined with genetic vulnerability and environmental influences. By framing addiction as a disease, this model emphasizes treatment, long-term management, and compassion over blame and punishment.
According to the disease model, substances alter the brain’s reward, motivation, and stress systems. Over time, these changes reduce self-control and increase cravings, making it extremely difficult for individuals to stop using substances through willpower alone. Just as with other chronic illnesses such as diabetes or hypertension, symptoms can improve with treatment but may return without ongoing care.
One of the key strengths of the disease model is its potential to reduce stigma. When addiction is recognized as a health condition, individuals are more likely to seek help without shame. Families and communities are also more likely to respond with empathy and support rather than judgment. Within this framework, relapse is viewed as a setback or flare-up of the disease rather than a personal failure.
The disease model has strongly influenced modern addiction treatment. Evidence-based approaches such as medication-assisted treatment, behavioral therapies, counseling, and long-term recovery support align with this perspective. Treatment plans focus on managing symptoms, preventing relapse, and improving quality of life rather than expecting immediate or permanent abstinence after short-term intervention.
However, the disease model is not without limitations. Critics argue that it may underemphasize personal responsibility or social factors if applied too narrowly. For this reason, many modern approaches integrate the disease model with psychological, social, and behavioral frameworks to provide comprehensive care.
Overall, the Disease Model Theory of Addiction represents a major shift toward science-based, compassionate treatment. By understanding addiction as a medical condition that requires ongoing care and support, individuals, families, and communities can foster more effective recovery pathways and reduce the stigma that often surrounds substance use disorders.
Self-Management Strategies for Understanding the Disease Model Theory of Addiction
The Disease Model Theory of Addiction explains addiction as a chronic, relapsing medical condition that affects brain function, behavior, and decision-making. While this perspective has transformed modern treatment, many individuals still struggle to fully accept addiction as a disease rather than a personal failure. Self-management strategies play an important role in helping individuals understand this model and apply it to their own recovery or prevention efforts.
A foundational self-management strategy is education and self-learning. Reading evidence-based resources, attending psychoeducation groups, and learning how substances affect brain chemistry help individuals understand why cravings, withdrawal, and relapse occur. This knowledge reduces self-blame and replaces confusion with clarity.
Self-observation and symptom tracking also support understanding the disease model. Monitoring cravings, mood changes, stress levels, and triggers helps individuals recognize addiction symptoms as medical and behavioral responses rather than character flaws. Tracking patterns reinforces the idea that addiction follows predictable cycles influenced by biology and environment.
Practicing self-compassion is essential. Viewing addiction as a disease encourages individuals to treat themselves with patience and understanding, especially during setbacks. Self-compassion supports accountability without shame and promotes continued engagement in recovery efforts.
Cognitive reframing further strengthens this understanding. Replacing thoughts such as “I lack willpower” with “my brain is responding to stress and triggers” aligns personal experience with the disease model. This shift encourages problem-solving and treatment-seeking instead of self-punishment.
Another important strategy is actively engaging in treatment and support. Medication management, therapy, peer support groups, and recovery programs reinforce the medical nature of addiction. Participation in these services helps individuals experience firsthand how structured care improves symptoms.
By using self-management strategies to understand the Disease Model Theory of Addiction, individuals learn to recognize addiction as a health condition requiring care, consistency, and support. This perspective empowers recovery by replacing shame with knowledge and self-judgment with informed self-care.
Family Support Strategies for Understanding the Disease Model Theory of Addiction
The Disease Model Theory of Addiction defines addiction as a chronic medical condition involving changes in brain chemistry, behavior, and impulse control. While this perspective is widely accepted in healthcare, many families struggle to move away from viewing addiction as a matter of choice or character. Family support strategies focused on understanding the disease model help shift attitudes, reduce stigma, and strengthen recovery outcomes.
A critical family strategy is education about addiction science. Learning how substances affect the brain’s reward and stress systems helps families understand why cravings, withdrawal, and relapse occur. This knowledge reframes addiction-related behaviors as symptoms of a disease rather than intentional wrongdoing, fostering empathy instead of frustration.
Language awareness also plays an important role. Families who adopt person-centered language and avoid blame-based statements reinforce the disease model. Referring to addiction as a health condition rather than a failure encourages open communication and reduces shame.
Another key strategy is reframing relapse. Within the disease model, relapse is understood as a recurrence of symptoms rather than proof that recovery has failed. Families who respond with problem-solving and support rather than punishment help individuals remain engaged in treatment and recovery.
Families can also support disease-model understanding by encouraging consistent adherence to treatment. Attending medical appointments, therapy sessions, or family education programs together reinforces the medical nature of addiction. This shared involvement normalizes ongoing care and reduces isolation.
Equally important is family self-care and support. Addiction affects the entire family system. Participating in family counseling or support groups helps relatives manage stress, process emotions, and maintain healthy boundaries while staying supportive.
By adopting family support strategies grounded in the Disease Model Theory of Addiction, families learn to recognize addiction as a health condition that requires patience, treatment, and long-term care. This shift strengthens trust, reduces conflict, and creates a more supportive environment for lasting recovery.
Community Resource Strategies for Understanding the Disease Model Theory of Addiction
The Disease Model Theory of Addiction recognizes addiction as a chronic, relapsing medical condition shaped by brain changes, genetics, mental health, and environmental factors. While this model is widely supported by scientific research, community understanding often lags behind medical knowledge. Community resource strategies play a vital role in helping the public recognize addiction as a disease and respond with treatment-focused solutions rather than stigma or punishment.
One of the most effective community strategies is public education and awareness. Health departments, schools, nonprofits, and community organizations can provide evidence-based education explaining how substances alter brain chemistry and behavior. These programs help replace myths rooted in moral judgment with accurate medical information, fostering compassion and early help-seeking.
Integrated healthcare services further reinforce the disease model. Community clinics, primary care offices, and mental health centers that screen for substance use disorders normalize addiction as part of overall health. When addiction care is embedded into routine medical services, individuals are less likely to feel labeled or marginalized.
Peer support and recovery-oriented programs also strengthen community understanding. Recovery coaches, peer-led groups, and recovery community centers share lived experiences that humanize addiction and demonstrate how ongoing care supports stability. These resources reinforce the idea that addiction, like other chronic illnesses, requires long-term management rather than short-term fixes.
Communities can also promote disease-model understanding through policy and workforce training. Educating healthcare providers, educators, law enforcement, and employers on trauma-informed and medical approaches to addiction helps reduce discrimination and improve referrals to treatment instead of punishment.
Finally, accessible support services such as housing assistance, employment programs, counseling, and harm-reduction initiatives address social factors that influence addiction severity and recovery. Meeting these needs reinforces the medical perspective by supporting overall health and stability.
By investing in education, integrated care, peer support, and compassionate policies, communities help shift public perception of addiction from a moral issue to a medical condition. This shift increases treatment engagement, reduces stigma, and supports sustainable recovery.
Frequently Asked Questions
Here are some common questions:
What is the Disease Model Theory of Addiction?
The Disease Model Theory views addiction as a chronic, relapsing medical condition that affects brain structure, chemistry, and behavior rather than a moral failure or lack of willpower.
Why is addiction considered a disease under this model?
Repeated substance use causes measurable changes in brain reward, motivation, and stress systems, leading to cravings, loss of control, and continued use despite negative consequences.
Does recognizing addiction as a disease remove personal responsibility?
No. It shifts responsibility for managing a health condition toward treatment, coping strategies, and ongoing care rather than toward blame and punishment.
How does the disease model explain relapse?
Relapse is defined as the recurrence of symptoms, similar to flare-ups in other chronic illnesses, and signals a need for treatment adjustment rather than failure.
What are common signs that addiction is a disease?
Loss of control over use, intense cravings, tolerance, withdrawal symptoms, and continued use despite harm indicate disease-related brain changes.
How does the disease model reduce stigma?
By framing addiction as a medical condition, it replaces judgment with compassion and encourages people to seek help without shame.
What types of treatment align with the disease model?
Medication-assisted treatment, counseling, behavioral therapies, peer support, and long-term recovery planning.
Can addiction be managed like other chronic diseases?
Yes. With consistent care, symptom management, and lifestyle support, many individuals achieve long-term stability.
How can families recognize addiction as a disease?
By understanding brain changes, using supportive language, and responding to relapse with problem-solving instead of punishment.
What role do communities play in reinforcing the disease model?
Communities promote understanding through education, integrated healthcare services, and stigma-free recovery resources.
Why is early recognition important?
Early identification allows for timely treatment, reducing the severity and long-term impact of addiction.
Is recovery possible under the disease model?
Yes. Recognizing addiction as a disease increases access to care, improves engagement in treatment, and supports long-term recovery success.
Conclusion
Recognizing addiction as a disease shifts the focus from blame and punishment to compassion and evidence-based care. When addiction is understood as a medical condition, relapse is viewed as a signal for treatment adjustment rather than failure, and recovery becomes a process of long-term management. Embracing the Disease Model Theory of Addiction encourages early intervention, reduces stigma, and promotes supportive responses that improve recovery outcomes. By treating addiction as a disease, individuals are more likely to seek help, remain engaged in care, and achieve lasting recovery.
Video: Why Addiction Feels Impossible to Stop (Science Explains) #brainhealth #substanceuse