Recovery success rates vary across different types of addiction, shaped by biological dependence, brain changes, social conditions, and access to treatment. Opioid use disorder is often identified as having one of the lowest long-term recovery success rates due to intense physical dependence, high relapse risk, and structural barriers such as stigma and limited access to sustained care. However, low success rates do not reflect a lack of effort or motivation. Instead, they highlight the need for comprehensive, long-term recovery strategies that extend beyond detoxification. Improving addiction success rates requires coordinated approaches that empower individuals through self-management skills, strengthen family involvement, and expand community-based resources that support recovery as an ongoing process.
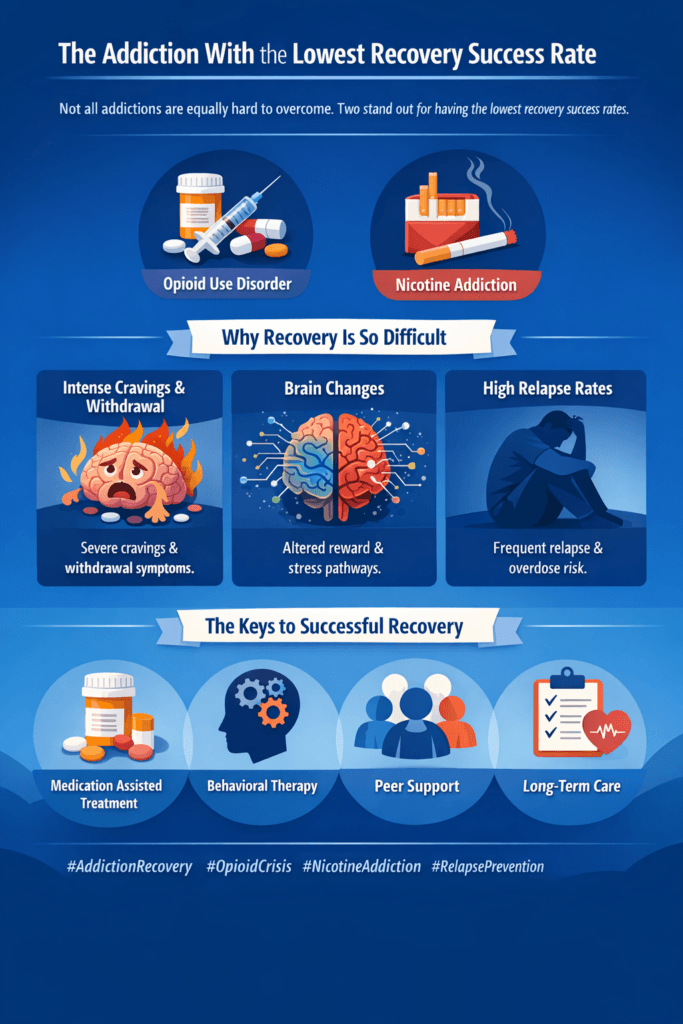
The Addiction With the Lowest Recovery Success Rate: Why It’s So Challenging
Recovery success rates vary widely across different types of addiction, influenced by biological, psychological, social, and environmental factors. While many substances and behaviors are associated with relapse risk, research consistently shows that opioid use disorder (OUD) has one of the lowest long-term recovery success rates when compared to other addictions. This does not mean that recovery is impossible; rather, it highlights the condition’s complexity and the need for sustained, evidence-based care.
Opioid addiction powerfully alters brain chemistry, particularly the systems responsible for pain regulation, reward, and stress response. Over time, opioids reduce the brain’s natural ability to produce and regulate pleasure and comfort, making cravings intense and withdrawal symptoms severe. Physical dependence develops quickly, and withdrawal can involve extreme pain, gastrointestinal distress, anxiety, insomnia, and strong drug-seeking behavior. These factors alone make early recovery difficult to sustain without medical support.
Another major challenge is high relapse risk. Even after detoxification, the brain may take months or years to stabilize. Stress, trauma, exposure to triggers, or reduced tolerance after abstinence significantly increase the risk of relapse and overdose. This is especially dangerous with opioids, as lowered tolerance can make previously “normal” doses fatal.
Social and structural barriers further reduce recovery success rates. Stigma surrounding opioid addiction discourages many individuals from seeking help or staying in treatment. Limited access to medication-assisted treatment, inconsistent insurance coverage, legal consequences, unstable housing, and lack of long-term follow-up care all undermine recovery efforts.
Despite these challenges, outcomes improve dramatically with long-term, comprehensive treatment, particularly when medication-assisted treatment is combined with counseling, peer support, and community-based services. Recovery from opioid addiction often requires ongoing care rather than a short-term intervention.
Understanding why opioid addiction has lower recovery success rates helps shift the conversation away from blame and toward compassion, science, and sustained support. Recovery is not a single event—it is a process that becomes more achievable when individuals receive evidence-based care, patience, and long-term resources.
Self-Management Strategies That Improve Addiction Recovery Success Rates
Addiction recovery success is influenced not only by professional treatment, but also by the daily choices and self-management skills individuals develop over time. While addiction is a complex medical and psychological condition, self-management strategies play a critical role in improving long-term recovery outcomes. These strategies empower individuals to actively participate in their healing, reduce the risk of relapse, and build sustainable, healthy lifestyles.
One of the most effective self-management tools is self-awareness. Recognizing personal triggers such as stress, emotional distress, social pressure, or environmental cues allows individuals to anticipate cravings and respond proactively. Tracking moods, cravings, and behaviors through journaling or recovery apps helps identify patterns and reinforces accountability without self-judgment.
Routine and structure are also essential. Consistent sleep schedules, regular meals, exercise, and planned daily activities stabilize brain chemistry and reduce impulsive decision-making. Structure helps replace chaotic patterns associated with substance use and creates predictability that supports emotional regulation.
Coping skills development significantly improves recovery success rates. Learning techniques such as mindfulness, deep breathing, urge surfing, and cognitive reframing helps individuals tolerate discomfort without returning to substance use. These skills are especially important during early recovery, when cravings and emotional sensitivity are strongest.
Self-management also includes goal setting and progress tracking. Setting realistic, short-term goals builds confidence and motivation, while celebrating small successes reinforces positive behavior change. Recovery is strengthened when progress is measured by growth rather than perfection.
Another critical strategy is self-compassion. Harsh self-criticism increases stress and relapse risk, while compassionate self-talk supports resilience after setbacks. Viewing lapses as learning opportunities rather than failures keeps individuals engaged in recovery rather than abandoning it.
Finally, effective self-management involves knowing when to seek support. Reaching out to counselors, peer support groups, healthcare providers, or trusted individuals is a sign of strength, not weakness. Combining self-management with external support creates a balanced approach to recovery.
When individuals actively manage their recovery through awareness, structure, coping skills, and self-compassion, addiction success rates improve. Recovery becomes a long-term process of growth, self-care, and empowerment rather than a short-term struggle driven by willpower alone.
Family Support Strategies That Improve Addiction Recovery Success Rates
Family involvement is one of the most influential factors in long-term addiction recovery success. While professional treatment provides essential clinical care, family support shapes the environment in which recovery either strengthens or struggles. When families are informed, compassionate, and consistent, recovery success rates improve significantly.
One of the most effective family strategies is open and non-judgmental communication. When individuals feel safe discussing cravings, setbacks, or emotional challenges, they are more likely to seek help early rather than hide their struggles. Listening without blame reduces shame, which is a major driver of relapse.
Education about addiction also plays a critical role. Understanding addiction as a medical and behavioral condition—rather than a moral failing—helps families respond with empathy and realism. Knowledge about withdrawal, relapse risk, and treatment options allows families to recognize warning signs and encourage timely intervention.
Families improve recovery outcomes by establishing healthy boundaries. Boundaries provide structure and accountability without punishment. Clear expectations around substance-free environments, responsibilities, and safety protect both the individual and the family while reinforcing recovery goals.
Another important strategy is encouraging treatment engagement. Family members can support attendance at medical appointments, counseling sessions, and peer recovery meetings. Positive reinforcement for treatment participation increases motivation and adherence.
Families also strengthen recovery by supporting healthy routines. Shared meals, regular sleep schedules, physical activity, and stress-reducing activities promote stability and connection. These routines reduce isolation and help replace substance-centered behaviors with healthy alternatives.
Equally important is family self-care. When families attend support groups or counseling, they reduce burnout, improve communication skills, and model healthy coping behaviors. A stable and supported family system is better equipped to sustain recovery over time.
When families combine education, compassion, boundaries, and active involvement, addiction recovery success rates improve. Recovery is not an individual journey—it is strengthened by informed, consistent, and supportive family relationships.
Community Resource Strategies That Improve Addiction Recovery Success Rates
Addiction recovery does not happen in isolation. While individual effort and clinical treatment are essential, community resources play a critical role in improving long-term addiction success rates. Communities that provide accessible, coordinated, and compassionate services create environments where recovery is supported, relapse risk is reduced, and individuals are more likely to remain engaged in care.
One of the most effective community strategies is the provision of accessible treatment and healthcare services. Community health centers, primary care clinics, and outpatient treatment programs that integrate addiction screening and follow-up care help identify substance use disorders early and maintain continuity of treatment. When services are affordable and easy to access, individuals are more likely to seek help before addiction becomes severe.
Peer support and recovery networks significantly improve recovery outcomes. Mutual support groups, recovery coaches, and community recovery centers offer connection, accountability, and shared experience. These resources reduce isolation and stigma while reinforcing hope and motivation. Peer-based support has been shown to increase treatment retention and long-term abstinence.
Communities also improve success rates through education and prevention programs. Public awareness campaigns, school-based education, and workplace wellness initiatives help reduce stigma and promote understanding of addiction as a health condition. Education encourages early intervention and normalizes help-seeking behavior.
Housing, employment, and social services are equally vital. Stable housing, job training, and financial assistance address social stressors that often contribute to relapse. Recovery is more sustainable when individuals have safe living conditions, meaningful work, and supportive social networks.
Another key strategy is harm reduction and crisis support. Naloxone distribution, crisis hotlines, and referral systems prioritize safety while guiding individuals toward treatment readiness. These programs save lives and maintain engagement with healthcare systems.
When communities invest in coordinated care, peer support, education, and social stability, addiction recovery success rates improve. Recovery becomes a shared public health effort rather than an individual burden, thereby strengthening individuals, families, and communities.
Frequently Asked Questions
Here are some common questions:
Which addiction has the lowest recovery success rate?
Opioid Use Disorder is often identified as having one of the lowest long-term recovery success rates due to intense physical dependence, severe withdrawal symptoms, high relapse risk, and reduced tolerance after abstinence.
Why is opioid addiction harder to recover from than other addictions?
Opioids significantly alter brain reward, pain, and stress systems. These changes create powerful cravings, long-lasting withdrawal effects, and heightened overdose risk, making sustained recovery more difficult without long-term treatment.
Does a low success rate mean recovery is unlikely?
No. A low success rate reflects the complexity of the condition, not a lack of effort or ability. With proper, ongoing support, many individuals achieve stable, long-term recovery.
Why does relapse occur so frequently with opioid addiction?
Relapse is influenced by lingering brain changes, stress, trauma, exposure to triggers, and limited access to continuous care. Reduced tolerance after abstinence also increases overdose risk.
How can self-management improve addiction success rates?
Self-management strategies such as identifying triggers, building daily routines, developing coping skills, practicing mindfulness, and using self-compassion reduce cravings and improve emotional regulation.
Why is self-compassion important in recovery?
Harsh self-judgment increases stress and relapse risk. Self-compassion helps individuals recover from setbacks, stay engaged in treatment, and view recovery as a process rather than a failure.
How does family support improve recovery success rates?
Families provide stability, accountability, and encouragement. Open communication, education about addiction, and healthy boundaries reduce shame and increase treatment engagement.
Can family involvement reduce relapse risk?
Yes. Supportive family environments reduce stress, increase motivation, and encourage individuals to seek help early when challenges arise.
What role do community resources play in improving recovery outcomes?
Community resources provide access to healthcare, medication-assisted treatment, peer support, housing, employment services, and harm-reduction programs that support long-term stability.
Why is long-term treatment important for opioid addiction?
Opioid recovery often requires ongoing care rather than short-term detox. Long-term treatment helps stabilize brain chemistry and reduce relapse risk.
How do peer support programs improve success rates?
Peer support reduces isolation, builds accountability, and reinforces hope through shared lived experience, increasing retention in recovery programs.
Can addiction success rates improve overall?
Yes. When self-management skills, family support, and community resources work together, even the most challenging addictions become more manageable, and long-term recovery becomes more achievable.
Conclusion
Although some addictions present greater recovery challenges, success rates improve significantly when recovery is supported at multiple levels. Self-management strategies such as trigger awareness, structured routines, coping skills, and self-compassion help individuals maintain daily stability. Family support through education, healthy boundaries, and consistent encouragement reduces the risk of relapse and promotes treatment engagement. Community resources—including accessible healthcare, peer support, housing, employment services, and harm-reduction programs—provide the stability and continuity necessary for long-term recovery. When individual effort is reinforced by family and community systems, even the most difficult addictions can become manageable, transforming recovery from a fragile outcome into a sustainable journey.
Video: Opioids vs Nicotine: Which Addiction is Harder to Beat #addiction #recovery #comparison