Neuromodulation is getting a lot of attention as a treatment option for people dealing with substance use disorders (SUDs). It’s a fresh approach in addiction medicine, offering hope to those who haven’t had much luck with standard therapies. In recent years, research and clinical studies have started to shine a light on ways neuromodulation might help people manage cravings and lower relapse rates. This article is a closer look at what neuromodulation is, how it works for SUDs, and what to keep in mind if you’re curious about the future of addiction treatment.
Understanding Neuromodulation for Substance Use Disorders
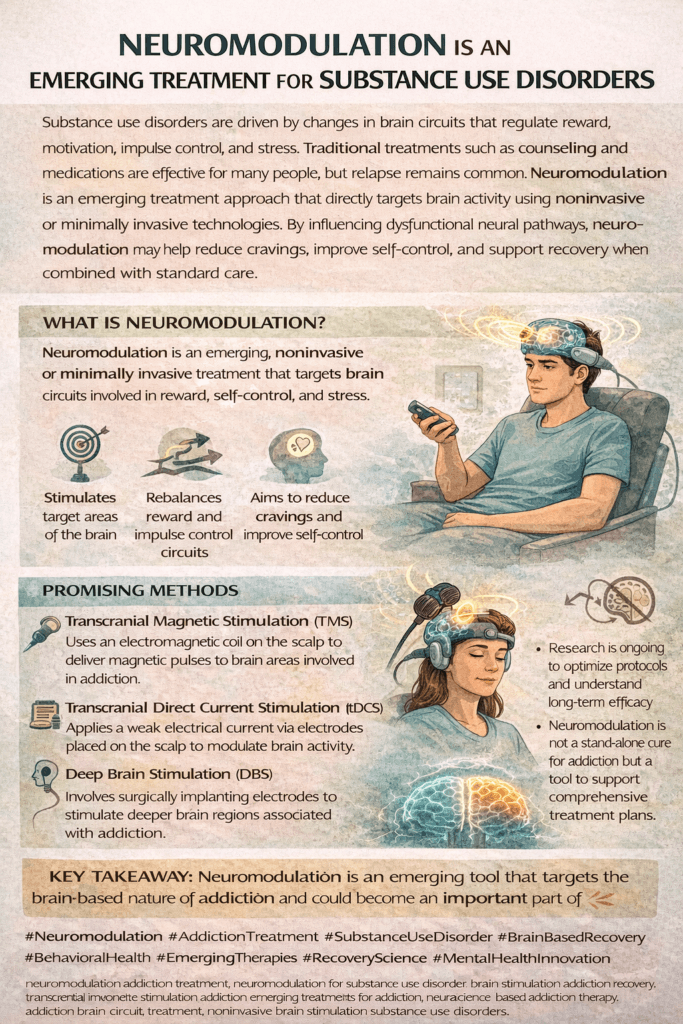
Neuromodulation is a broad term, but at its core, it means using technology to change how the brain communicates with itself. In medical practice, this usually involves stimulating specific parts of the nervous system to get therapeutic effects. For substance use disorders, the goal is to tweak brain circuits linked to cravings, impulse control, and reward, which play a big role in addiction and relapse.
The field of neuromodulation started in areas like chronic pain and Parkinson’s disease, but now researchers are checking out its impact in psychiatry and addiction medicine. The numbers show just how big the need is—over 20 million people in the United States live with a substance use disorder, and many of them don’t respond well to traditional treatments.
The growing interest in neuromodulation comes from advances in technology and a better understanding of how the brain works in addiction. Instead of focusing solely on talk therapy and medication, neuromodulation targets the brain’s electrical signals, offering people new options when other approaches haven’t worked. The research community and clinicians are excited about what this means for the future.
Basics of Neuromodulation Techniques Used in Addiction
The main neuromodulation methods used for SUDs are noninvasive and don’t require surgery. These include transcranial magnetic stimulation (TMS), transcranial direct current stimulation (tDCS), and, less commonly right now, deep brain stimulation (DBS). Each offers a different approach to influencing brain activity.
- Transcranial Magnetic Stimulation (TMS): Sends magnetic pulses to certain areas on the scalp to change brain activity below the surface. It’s painless and usually done in short outpatient sessions.
- Transcranial Direct Current Stimulation (tDCS): Sends a gentle electrical current between two electrodes placed on the head. It can change the likelihood of cravings or impulsive decisions by adjusting brain activity up or down.
- Deep Brain Stimulation (DBS): Needs a surgical procedure to implant electrodes deep in the brain. Although it’s not widely used for addiction yet, research is ongoing for severe, tough-to-treat cases.
Every method has its own strengths and challenges. Most studies so far have focused on TMS and tDCS because they’re noninvasive, widely available, and don’t require anesthesia or recovery time. If you want to check out more, trusted resources from the National Institute on Drug Abuse and clinical guidelines from large health organizations are a great starting point.
Key Steps in Getting Started with Neuromodulation
Thinking about neuromodulation for substance use? There are some basics to get familiar with as you look into this option. Here’s a practical rundown on starting these treatments:
- Talk with an Addiction Specialist: Not everyone is the right match for neuromodulation, so getting a detailed assessment from an expert helps set you on the right path.
- Review Your Treatment History: Neuromodulation is typically considered when other treatments, such as cognitive-behavioral therapy and medications, haven’t been successful. Your provider will look at your whole journey to figure out what might help next.
- Medical and Safety Screening: Some types of neuromodulation aren’t allowed for people with certain implants, medical conditions, or for those who are pregnant.
- Choose a Treatment Setting: Most neuromodulation takes place in an outpatient setting, meaning you visit a clinic a few times a week and then head home.
- Ongoing Monitoring and Support: Neuromodulation is most effective when combined with counseling, peer support, or medication-assisted treatment as part of an all-in-one plan.
For anyone just starting out, working with a supportive care team makes a big difference. Don’t hesitate to ask questions about goals, risks, or what to expect.
Real-Life Challenges and How to Steer Through Them
Trying neuromodulation comes with its own learning curve. Many people run into a few common stumbling blocks:
- Expectations: This isn’t an overnight fix. While some see quick changes in cravings or mood, the effects often build up slowly over several weeks.
- Access and Cost: Treatments aren’t always close to home, and insurance coverage can be hit-or-miss. It helps to check out local providers and ask about payment plans up front.
- Evidence and Results: Neuromodulation holds promise, but the research is still in its early stages. It’s important to remember that everyone’s experience is unique, and we’re still learning from new clinical trials.
- Side Effects: Most side effects are mild, such as headaches or scalp tingling, but you should always discuss any risks before starting.
Managing Expectations
It’s key to be patient. Neuromodulation usually doesn’t erase cravings overnight. Some feel better after several sessions, others need a bit more time. Knowing what to expect can ease frustration.
Insurance and Cost
The cost can be a hurdle if you don’t have coverage. It pays to call insurance companies to check on what’s included and to speak with clinics about payment plans or financial aid options.
Personalization and Adjustments
Not every approach works on the first try. Doctors might change the target area in the brain or adjust the treatment schedule, sometimes combining neuromodulation with other therapies. Staying in good communication with your care team is crucial.
Can Neuromodulation Help Me? Practical Benefits and Next-Level Cool Features
More studies show that neuromodulation can help people with substance use issues, especially with cravings, mood swings, and impulse control. While it’s not a cure, it can give a boost to your odds of making progress if other options have fallen short.
- Less Craving: Repeated sessions often turn down the urge to use substances, a key benefit during the challenging early phase of recovery.
- Improved Self-Control: Many people report better decision-making and fewer slip-ups.
- Mood Lifting: A modest boost in depression and anxiety symptoms can keep motivation and hope alive during recovery.
- Works Alongside Other Treatments: Neuromodulation can be paired with talk therapy or medications for a stronger recovery plan.
It’s important to keep in mind that everyone responds differently. Researchers are still trying to figure out why some benefit more and which subtypes of substance use are most responsive.
Commonly Asked Questions About Neuromodulation for SUDs
People often ask how neuromodulation fits into everyday life during recovery. Here are some common questions and what I’ve picked up from patients and providers:
Question: Who is a good candidate for neuromodulation?
Answer: People who have tried other treatments without success, and who don’t have conditions that would keep them from using brain stimulation, are often considered. Being open about your treatment history helps doctors decide if it’s a good fit.
Question: Are the treatments painful or tough to handle?
Answer: Most people find TMS and tDCS pretty comfortable. There might be mild tingling or pressure, but it’s easy to work through with a short break or tweak to the settings.
Question: How long does it take to see changes?
Answer: Many programs run daily or several times a week over a span of weeks. Most people notice minor shifts early, but big improvements typically show up near the end of a full round of sessions.
Question: Can I use neuromodulation with therapy or meds?
Answer: Absolutely, and experts recommend it. Combining strategies usually increases your chances of success.
Next Steps and Where to Track Down More Info
Neuromodulation remains in the next stage of addiction treatment, but early results are promising, especially for those dealing with hard-to-treat substance use disorders. If you’re interested or think it could help with your recovery, have an open talk with an addiction specialist. Community support, regular monitoring, and an adventurous spirit for trying new things all help set you up for success with these modern options.
Keep up with research and news by following organizations like the National Institute on Drug Abuse. Staying informed means you can track new advances and possible clinical trials. As the field grows, options for people in recovery will likely continue to expand, offering more hope for moving forward.
Video: NEUROMODULATION IS AN EMERGING TREATMENT FOR SUBSTANCE USE DISORDERS