Cravings are a natural and expected part of addiction recovery, yet they are often met with fear, shame, or self-criticism. Responding to cravings with compassion shifts the focus from punishment to understanding, recognizing urges as temporary brain responses rather than personal failures. When cravings are approached with kindness, curiosity, and patience, individuals are better able to regulate emotions, reduce stress, and make intentional choices that support recovery.
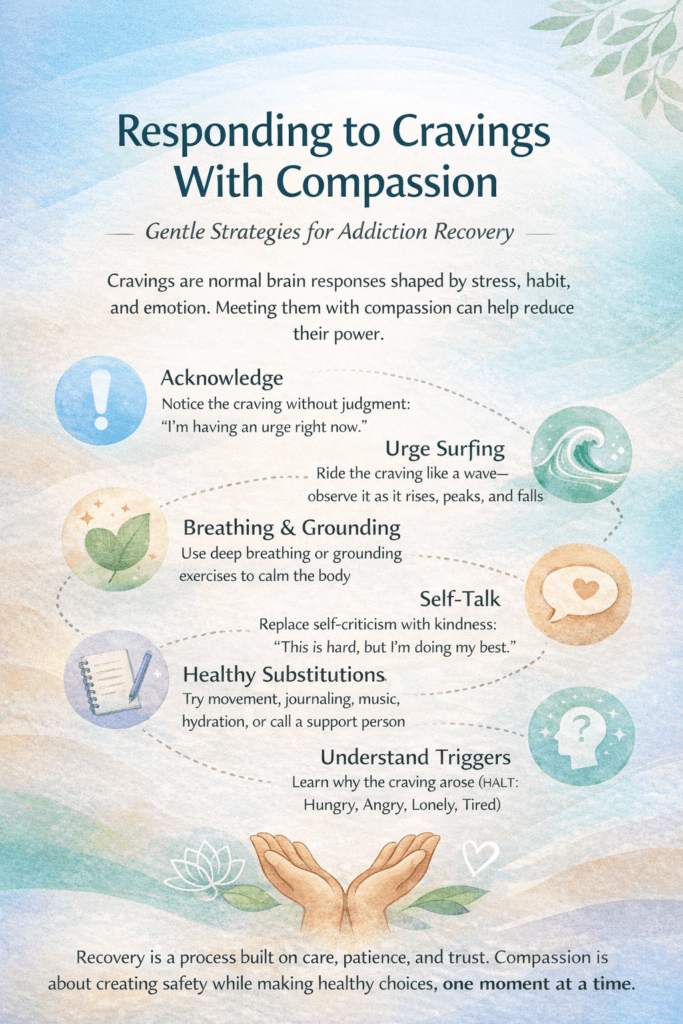
Responding to Cravings With Compassion
Cravings are one of the most misunderstood parts of addiction and recovery. They’re often treated as enemies to fight, weaknesses to suppress, or signs of failure. But cravings are not moral flaws—they are learned brain responses shaped by stress, trauma, habit, and neurobiology. Responding to cravings with compassion can transform them from overwhelming threats into manageable signals.
When a craving appears, the instinctive reaction is often shame or panic: Why am I thinking this? What’s wrong with me? These reactions activate the stress response, which ironically intensifies the craving. Compassion interrupts that cycle. Instead of judgment, it offers understanding: This urge is uncomfortable, but it makes sense given what my brain has learned.
Compassionate responding begins with noticing rather than resisting. A craving can be observed like a wave—it rises, peaks, and eventually falls. You don’t have to obey it, but you don’t have to attack it either. Naming the experience (“I’m having an urge right now”) creates distance between the craving and your identity. You are not the craving; you are the person experiencing it.
Self-compassion also involves curiosity. What triggered this urge? Fatigue, loneliness, stress, celebration, or old routines often play a role. Understanding the trigger turns cravings into information instead of commands. This awareness allows for intentional coping—deep breathing, grounding exercises, movement, hydration, connection, or distraction—rather than reactive behavior.
Importantly, compassion does not mean permissiveness. It does not excuse harmful actions or minimize consequences. It means treating yourself with the same care you would offer someone else who is struggling. Recovery is not strengthened by harshness; it is strengthened by safety, patience, and trust.
Over time, compassionate responses help retrain the brain. Each time a craving is met with calm acknowledgment and healthy coping, new neural pathways are reinforced. The urge loses power, not because it is fought, but because it is understood.
Responding to cravings with compassion is a skill that develops with practice. It reminds us that recovery is not about perfection—it’s about resilience, learning, and choosing care over criticism, one moment at a time.
Responding to Cravings With Compassion: Self-Management Strategies for Recovery
Cravings are a normal part of addiction recovery, not a personal failure. They reflect how the brain learned to cope with stress, emotion, and reward. When cravings are met with shame, fear, or self-criticism, they often intensify. When they are met with compassion, they become manageable experiences rather than overwhelming commands. Self-management strategies rooted in compassion help individuals stay grounded, build resilience, and maintain long-term recovery.
A compassionate approach begins with acknowledgment. Instead of trying to push a craving away, notice it without judgment. Saying, “I’m experiencing a craving right now,” separates the urge from your identity. This simple step reduces emotional reactivity and creates space for choice.
Breathing and grounding techniques are powerful tools. Slow, intentional breathing calms the nervous system and lowers stress hormones that fuel cravings. Grounding exercises—such as noticing five things you can see, four you can feel, and three you can hear—help refocus attention on the present moment, where cravings have less control.
Another key strategy is urge surfing. Cravings behave like waves: they rise, peak, and fall. Instead of fighting the wave, ride it. Set a short timer and observe your body’s sensations with curiosity. Most cravings pass within minutes when they are not fed by panic or resistance.
Self-talk matters deeply. Replace harsh inner dialogue with compassionate language. Statements such as “This is hard, and I’m doing my best” or “I don’t need to act on this feeling to survive it” reinforce a sense of emotional safety. Compassionate self-talk strengthens motivation and reduces the risk of relapse.
Trigger awareness supports proactive self-management. Hunger, anger, loneliness, tiredness, stress, and even celebration can increase vulnerability. Identifying patterns allows you to respond early with nourishment, rest, connection, or coping skills before cravings escalate.
Healthy substitutions are another compassionate strategy. Movement, hydration, music, journaling, prayer, mindfulness, or a brief connection with a trusted person can redirect attention without denial. The goal is not merely to distract, but to address the underlying need driving the craving.
Importantly, compassion does not mean giving in. It means holding yourself accountable without punishment. Recovery thrives in environments of patience, understanding, and consistency—not fear or self-blame.
By responding to cravings with compassion, individuals retrain the brain to associate urges with safety rather than urgency. Over time, cravings lose intensity and frequency. Self-management rooted in compassion turns recovery into a sustainable, humane process—one grounded in strength, awareness, and self-respect.
Responding to Cravings With Compassion: Family Support Strategies in Recovery
Cravings are a normal part of addiction recovery, yet they are often misunderstood by families. Loved ones may interpret cravings as a lack of commitment or a sign of impending relapse. In reality, cravings are learned brain responses to stress, memory, and emotion. When families respond with compassion rather than fear or frustration, they become powerful allies in recovery.
One of the most important family strategies is normalizing cravings. Helping a loved one understand that urges are expected—and not a failure—reduces shame and secrecy. Simple statements like, “I’m glad you told me,” or “Cravings don’t mean you’re doing something wrong,” reinforce trust and openness.
Compassionate communication is essential. Families should focus on listening more than fixing. When a person shares that they are struggling with cravings, responding with curiosity instead of interrogation helps de-escalate distress. Asking, “What do you need right now?” rather than offering immediate advice allows the individual to feel respected and supported.
Avoiding judgmental language is critical. Comments that imply weakness, disappointment, or threat can intensify cravings by increasing stress and emotional isolation. Replacing blame with empathy—“That sounds really hard”—helps calm the nervous system and supports self-regulation.
Families can also support recovery by encouraging healthy coping strategies. This might include suggesting a walk together, sharing a meal, practicing relaxation exercises, or engaging in a meaningful activity. These moments of connection reduce loneliness, a common trigger for cravings.
Boundaries remain important, even when practicing compassion. Supporting someone through cravings does not mean excusing harmful behavior or removing accountability. Clear, consistent boundaries create safety for both the individual in recovery and the family. Compassion and structure work best together.
Education plays a vital role. When families understand the neurobiology of addiction and cravings, fear is replaced with informed support. Learning that cravings are temporary brain events—not conscious choices—helps families respond calmly and effectively.
Finally, families should practice self-compassion. Supporting someone in recovery can be emotionally demanding. Seeking family support groups, counseling, or education helps loved ones manage their own stress while remaining present and supportive.
When families respond to cravings with compassion, they reduce shame, strengthen connection, and promote long-term recovery. Recovery does not happen in isolation—it grows in environments where understanding, patience, and care are consistently present.
Responding to Cravings With Compassion: Community Resource Strategies That Support Recovery
Cravings are a common and expected part of addiction recovery, yet many people struggle with them in silence due to shame or fear of judgment. Communities play a critical role in shaping how cravings are understood and managed. When community resources respond to cravings with compassion rather than punishment or stigma, they create environments where recovery can truly take root.
One of the most effective community strategies is peer support. Peer recovery groups, recovery community organizations, and mutual-aid meetings provide spaces where individuals can openly discuss cravings without fear of rejection. Hearing others normalize these experiences reduces isolation and reinforces the message that cravings do not define failure—they signal a need for support.
Accessible crisis and support services are another cornerstone. Hotlines, walk-in centers, mobile crisis units, and peer warm lines enable individuals to reach out during intense cravings. Compassionate responses during these moments—listening, reassurance, and practical coping guidance—can prevent escalation and reduce the risk of relapse.
Community-based education and stigma reduction are equally important. Public workshops, schools, faith-based organizations, and healthcare systems that teach the neurobiology of addiction help reframe cravings as health-related experiences rather than moral shortcomings. This understanding encourages earlier help-seeking and more supportive responses from the public.
Recovery-friendly spaces also make a difference. Libraries, community centers, gyms, and cafés that host sober events or recovery-focused programming offer safe alternatives to substance-centered environments. These spaces promote connection, belonging, and routine—protective factors against cravings.
Integrated health and social services strengthen compassionate responses. When primary care, mental health providers, housing services, employment programs, and addiction treatment collaborate, individuals are less likely to face unmet needs that trigger cravings. Coordinated care reduces stress and supports stability, both essential for recovery.
Community organizations can further support compassionate responses by offering skills-based workshops, including mindfulness training, stress management, emotion regulation, and relapse prevention. These programs empower individuals with practical tools while reinforcing self-compassion and resilience.
Finally, communities must also care for those providing support. Training for volunteers, clinicians, first responders, and peer workers in trauma-informed and compassion-centered approaches ensures that helpers respond effectively without burnout or judgment.
When communities respond to cravings with compassion, they transform recovery from an individual struggle into a shared responsibility. Supportive resources, informed responses, and inclusive spaces reduce harm, strengthen connection, and remind individuals in recovery that they are not alone—especially when they need compassion most.
Frequently Asked Questions
Here are some common questions:
What does it mean to respond to cravings with compassion?
Responding with compassion means acknowledging cravings without judgment or shame. Instead of viewing urges as failures, they are recognized as temporary brain responses shaped by stress, habit, and past learning. Compassion creates emotional safety, which helps reduce the intensity of cravings.
Does compassion mean giving in to cravings?
No. Compassion is not permissiveness. It allows individuals to hold boundaries and make healthy choices without self-punishment. You can acknowledge an urge without acting on it.
Why do cravings get stronger when I judge myself?
Self-criticism activates the stress response, increasing anxiety and emotional discomfort. This stress can intensify cravings because the brain seeks relief. Compassion calms the nervous system, making urges easier to manage.
How long do cravings usually last?
Most cravings peak and pass within minutes when they are not reinforced. Viewing cravings as waves—rising, peaking, and falling—helps individuals tolerate discomfort without reacting impulsively.
What is urge surfing?
Urge surfing is a mindfulness technique where cravings are observed without resistance. Instead of fighting the urge, individuals notice physical sensations and emotions until the craving naturally subsides.
Can compassionate self-talk really help?
Yes. Supportive self-talk, such as “This is uncomfortable, but I can handle it,” reduces emotional distress and strengthens self-regulation. Over time, compassionate language helps retrain the brain’s response to cravings.
What triggers cravings most often?
Common triggers include stress, fatigue, hunger, loneliness, emotional pain, celebration, and environmental cues. Understanding personal triggers allows for early intervention and self-care.
How can family or friends respond compassionately to cravings?
Supportive responses include listening without judgment, validating the experience, avoiding blame, and offering connection or practical support. Compassionate support reduces shame and promotes openness.
Is responding with compassion evidence-based?
Yes. Research in addiction science, trauma-informed care, and mindfulness shows that compassionate responses improve emotional regulation, reduce relapse risk, and support long-term recovery.
Will cravings ever go away completely?
For many people, cravings decrease in frequency and intensity over time. While occasional urges may occur, compassionate coping skills make them far less disruptive and easier to manage.
What if I slip after a craving?
A slip does not mean failure. Responding with compassion encourages learning rather than shame. Reflecting on triggers and supports helps strengthen future coping rather than abandoning recovery.
Why is compassion important for long-term recovery?
Recovery is sustained through safety, trust, and consistency—not fear or self-punishment. Compassion builds resilience, strengthens self-efficacy, and supports lasting behavioral change.
Conclusion
Responding to cravings with compassion is not about giving in—it is about creating safety, awareness, and resilience in the recovery process. By replacing judgment with understanding and criticism with care, cravings lose their power to control behavior. Over time, compassionate responses help retrain the brain, strengthen coping skills, and support lasting recovery. Compassion reminds us that healing is built through consistency and care, one moment and one choice at a time.
Video: The wave technique that changed recovery #RelapsePrevention #CravingManagement