Coordinated, whole-person care in addiction integrates medical, mental health, and social support to address all aspects of recovery. Its advantages include better outcomes and reduced relapse, but challenges such as high costs, complex implementation, and provider burnout exist. Ethical dilemmas can arise around autonomy, confidentiality, and equitable access. Success relies on self-management strategies like medication adherence and coping skills, family support through education and encouragement, and community resources such as peer groups, social services, and crisis programs. Together, these elements create a comprehensive, patient-centered approach to addiction recovery.
Coordinated Whole-Person Addiction Care
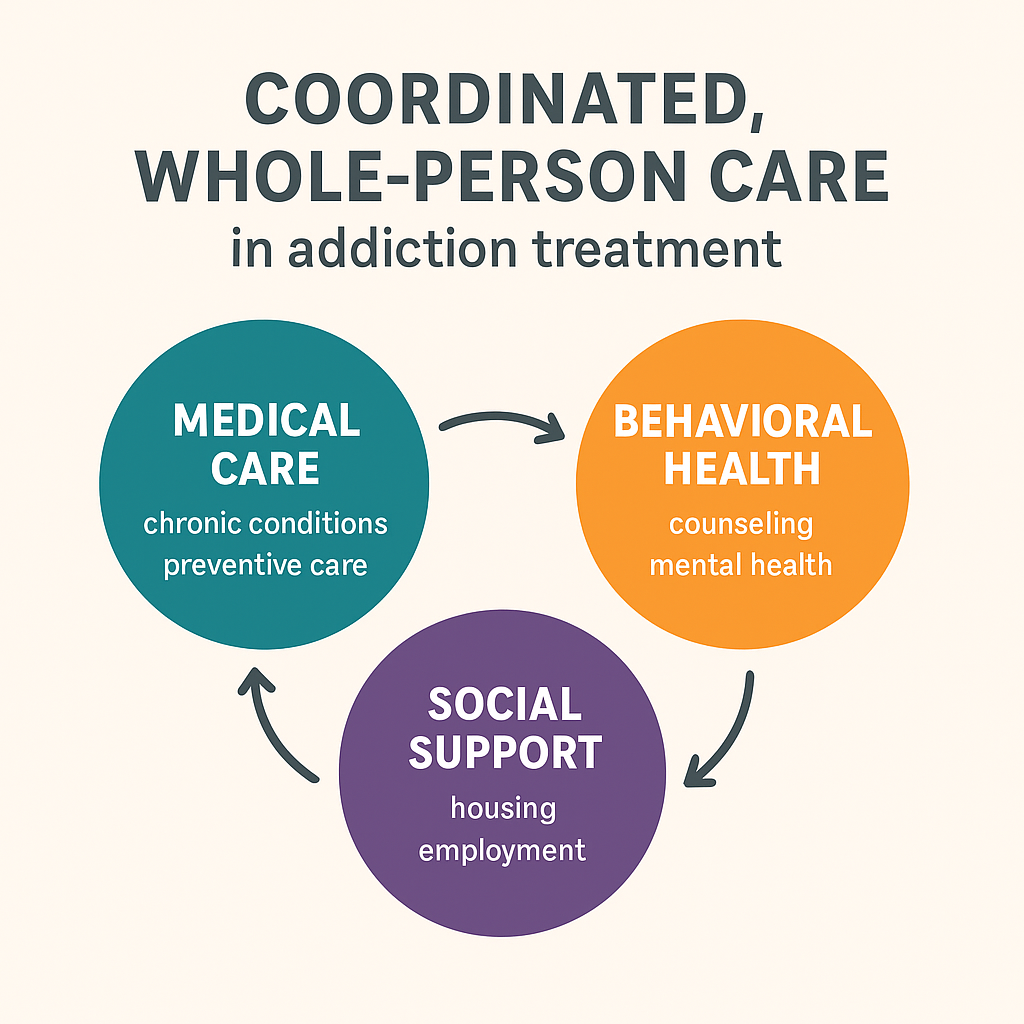
Coordinated, whole-person care in addiction treatment treats the individual as a complete, interconnected system rather than focusing only on substance use. It recognizes that addiction is shaped by physical, mental, social, and environmental factors, and effective care must address all of them together.
Key Principles
- Integration of Services: Combines medical, mental health, substance use, and social support into one coordinated plan.
- Patient-Centered: Tailors treatment to each person’s needs, goals, and circumstances.
- Continuity of Care: Promotes communication among providers to prevent gaps or conflicts.
- Evidence-Based Practices: Uses proven approaches like medication-assisted treatment and behavioral therapy, while managing co-occurring conditions.
Core Components
- Medical Care: Managing chronic conditions, preventive health, and safe medication use.
- Behavioral Health: Counseling, therapy for co-occurring disorders, and relapse prevention.
- Social Support: Help with housing, jobs, education, and reintegration into community life.
- Harm Reduction & Recovery Support: Tools like naloxone, syringe services, peer support, and long-term recovery planning.
Benefits
- Better treatment outcomes and retention.
- Lower relapse rates by addressing root causes.
- Improved health, functioning, and quality of life.
- Stronger collaboration among providers reduces fragmented care.
In short, coordinated whole-person care views addiction within the broader context of a person’s health and life circumstances, creating a more sustainable path to recovery.
Challenges of Coordinated Whole-Person Care in Addiction Treatment
Coordinated, whole-person care in addiction treatment—where physical health, mental health, social services, and addiction care are fully integrated—offers significant benefits. Yet, implementing this approach also brings several disadvantages and challenges that organizations must navigate.
Key Challenges
- Complex Implementation: Coordinating across multiple services requires extensive communication, planning, and collaboration. Smaller clinics often lack the infrastructure to integrate care effectively.
- Higher Costs: While whole-person care can save money in the long term by reducing relapse and hospitalizations, upfront expenses for staff training, integrated electronic health records (EHRs), and multidisciplinary teams are significant.
- Provider Burnout: Clinicians face heavier workloads and higher stress when addressing medical, behavioral, and social needs simultaneously, especially if staffing is limited.
- Fragmented Accountability: With many providers involved, responsibility for patient outcomes can become unclear, leading to gaps or conflicting treatment approaches.
- Patient Privacy Concerns: Sharing information across providers requires careful adherence to privacy laws such as HIPAA. Some patients may also resist sharing sensitive health data.
- Variable Quality Across Services: Uneven quality in mental health care, social services, or recovery supports can weaken the effectiveness of integrated models.
- Cultural and Systemic Barriers: Patients from marginalized communities may face stigma, mistrust, or difficulty navigating complex systems, reducing engagement.
- Delayed Access to Care: Coordinating assessments, approvals, and referrals across multiple providers can slow down the start of treatment.
In summary, while coordinated, whole-person care has the potential to transform addiction treatment by improving outcomes and supporting recovery, it also requires significant resources, strong leadership, and systemic reform. Without these, implementation can be slow, costly, and uneven—particularly in underfunded or fragmented health systems.
Ethical Dilemmas in Coordinated Whole-Person Addiction Care
Coordinated, whole-person care in addiction treatment—while highly beneficial—also introduces complex ethical dilemmas. By integrating physical health, mental health, social services, and addiction care, providers must balance competing values and responsibilities.
Key Ethical Challenges
- Autonomy vs. Beneficence: Integrated care often requires joint decision-making. This can create tension between respecting a patient’s autonomy—their right to make independent choices—and acting in their best interest when providers believe specific interventions are essential.
- Privacy and Confidentiality: With multiple providers involved, protecting sensitive information is more difficult. Breaches of confidentiality, intentional or accidental, raise serious ethical concerns.
- Resource Allocation: Whole-person care demands significant staffing, funding, and technology. Ethical questions emerge when resources are limited: who receives comprehensive care, and who does not?
- Informed Consent: When multiple treatments and services occur simultaneously, patients may struggle to grasp the scope of care fully. Ensuring explicit, meaningful consent across disciplines is a persistent challenge.
- Potential for Coercion: Patients may feel pressured to accept services tied to housing, employment, or legal compliance, blurring the line between voluntary and coerced participation.
- Cultural Sensitivity and Equity: Standardized care models may overlook cultural, social, or personal values, raising concerns about fairness, inclusivity, and respect for diversity.
- Professional Boundaries: Multidisciplinary teams can blur roles, creating conflicts between providers with differing ethical obligations—for example, between medical and behavioral health priorities.
In summary, while coordinated whole-person care holds promise for improving addiction outcomes, it requires careful navigation of ethical tensions. Providers must safeguard patient rights, maintain confidentiality, respect diversity, and uphold professional integrity—ensuring that holistic treatment does not come at the cost of ethical responsibility.
Self-Management Strategies in Whole-Person Addiction Care
In coordinated, whole-person addiction care, patients are not passive recipients of treatment—they are active participants in their recovery. While medical, mental health, and social service providers work together to deliver integrated support, self-management strategies empower individuals to take ownership of their health, build resilience, and sustain long-term recovery.
Key Self-Management Strategies
- Medication Adherence: Consistently take prescribed medications for addiction (e.g., buprenorphine, naltrexone) and co-occurring conditions. Tools such as reminders, pill organizers, and mobile apps can help maintain adherence.
- Routine Health Monitoring: Track health indicators such as blood pressure, weight, sleep, and mood. Report any changes promptly to providers for early intervention.
- Behavioral and Cognitive Skills: Apply coping strategies learned in therapy—such as CBT techniques, mindfulness, or stress-reduction exercises. Recognize triggers and develop action plans to prevent relapse.
- Goal Setting and Progress Tracking: Establish realistic, measurable recovery goals, such as attending meetings or reducing risky behaviors. Journals and apps can help monitor progress and setbacks.
- Engaging in Support Networks: Join peer recovery groups, family support programs, or community activities. Strong social connections play a crucial role in maintaining sobriety.
- Lifestyle and Wellness Management: Maintain consistent routines for exercise, nutrition, and sleep. Avoid high-risk environments that could trigger relapse.
- Communication and Advocacy: Share concerns, needs, or changes in symptoms openly with care teams. Advocate for personalized adjustments when treatments don’t align with goals.
- Education and Self-Awareness: Learn about addiction and co-occurring conditions. Build awareness of personal triggers and early warning signs to intervene before relapse escalates.
In summary, self-management strategies complement coordinated care by creating a feedback loop between patients and providers. By developing healthy routines, building awareness, and staying engaged, individuals strengthen their role as partners in recovery—empowered, supported, and prepared to sustain progress over the long term.
Family Support in Whole-Person Addiction Care
Family support is a vital element of coordinated, whole-person addiction care. By reinforcing recovery, providing emotional encouragement, and fostering a healthy environment, families play an active role in sustaining long-term progress. When integrated with professional treatment, family involvement strengthens recovery outcomes and reduces relapse risks.
Key Family Support Strategies
- Education and Awareness: Teach family members that addiction is a chronic medical condition, not a moral failing. Provide information about treatment options, relapse triggers, and recovery expectations to reduce stigma and build understanding.
- Open Communication: Foster honest, nonjudgmental conversations about struggles, progress, and emotions. Use active listening and empathy to support the individual in recovery.
- Structured Involvement in Care: Participate in family therapy or support groups. With patient consent, join coordinated care planning to align home support with treatment goals.
- Creating a Supportive Home Environment: Minimize exposure to triggers such as alcohol, drugs, or negative influences. Encourage routines that promote wellness, including healthy meals, exercise, and consistent sleep.
- Emotional Support and Encouragement: Provide positive reinforcement for recovery milestones and offer judgment-free support during setbacks.
- Boundary Setting: Establish clear, healthy boundaries to prevent enabling behaviors while maintaining care and connection.
- Peer and Community Resources: Encourage participation in groups such as Al-Anon or Nar-Anon, and connect with community programs that offer guidance and respite for families.
- Crisis Preparedness: Know how to respond to relapse, overdose, or mental health emergencies. Keep naloxone and emergency contacts readily available if needed.
In summary, in coordinated, whole-person care, family support works hand in hand with professional treatment to create a stable, recovery-focused environment. By combining education, open communication, healthy boundaries, and crisis preparedness, families can become powerful allies in their loved one’s journey to recovery.
Community Resource Strategies in Whole-Person Addiction Care
In coordinated, whole-person addiction care, recovery extends beyond clinical settings. Community resource strategies help individuals build resilience, reduce isolation, and address social determinants of health such as housing, employment, and access to supportive networks. These resources complement medical, mental health, and family-based interventions, creating a comprehensive system of support.
Key Community Resource Strategies
- Peer Support and Recovery Groups
- Participation in programs such as Alcoholics Anonymous (AA), Narcotics Anonymous (NA), or SMART Recovery.
- Access to peer mentors who provide accountability, encouragement, and shared lived experience.
- Social Services and Case Management
- Assistance with housing, transportation, employment, and financial resources.
- Case managers who coordinate across providers and community programs to ensure continuity of care.
- Educational and Vocational Programs
- Enrollment in skills training, adult education, or job placement programs.
- Building self-sufficiency and purpose—protective factors against relapse.
- Mental Health and Counseling Services
- Access to community-based therapy, trauma-informed care, and crisis hotlines.
- Integration with addiction treatment to address co-occurring mental health needs.
- Health and Wellness Programs
- Community fitness, nutrition, and wellness initiatives that promote overall health.
- Stress reduction, mindfulness, and support for a healthy lifestyle.
- Legal and Advocacy Resources
- Guidance for navigating legal issues, probation requirements, or disability services.
- Advocacy organizations that promote equity and reduce stigma in addiction care.
- Cultural and Faith-Based Supports
- Engagement with cultural programs, religious organizations, or faith-based communities.
- Supports that respect cultural values and provide meaning, belonging, and resilience.
- Crisis and Harm Reduction Services
- Access to overdose prevention programs, syringe exchanges, and naloxone distribution.
- Immediate support for high-risk situations, integrated with long-term recovery planning.
In summary, by leveraging community resources, coordinated care programs strengthen recovery networks and address the broader social and emotional needs of individuals. When combined with clinical treatment, family involvement, and self-management strategies, community supports create a holistic foundation for sustainable recovery.
Frequently Asked Questions
Here are some common questions:
Question: Why is whole-person coordinated care critical for individuals with addiction?
Answer: Whole-person coordinated care is essential for individuals with addiction because it treats recovery as more than just stopping substance use. Addiction often affects—and is influenced by—physical health, mental health, relationships, housing, employment, and social environments. Traditional, fragmented care that focuses only on substance use misses these interconnected factors, which can increase relapse risk and limit recovery.
Key reasons it matters:
- Addresses Root Causes: Many people with addiction also live with chronic medical conditions, trauma, or mental health disorders. Coordinated care manages these together rather than in isolation.
- Reduces Fragmentation: It ensures providers communicate, preventing gaps, duplicated efforts, or conflicting treatment plans.
- Improves Engagement and Retention: When care is person-centered and tailored, individuals are more likely to stay in treatment.
- Supports Long-Term Recovery: By including housing, employment, family support, and community resources, it builds a foundation for stability beyond medical treatment.
- Enhances Quality of Life: The focus shifts from just “not using substances” to helping individuals thrive physically, emotionally, and socially.
In short, whole-person coordinated care views addiction as part of a broader life context. It empowers individuals, integrates support, and increases the likelihood of lasting recovery.
Question: Why is whole-person coordinated care critical for families with addiction?
Answer: Whole-person coordinated care is just as critical for families as it is for individuals with addiction, because addiction rarely affects only one person—it impacts the entire household. Families often carry the emotional, financial, and social burden of addiction, and coordinated care brings them into the healing process instead of leaving them isolated.
Why it matters for families:
- Shared Understanding: Education about addiction as a chronic condition reduces stigma and blame, helping families support recovery with compassion instead of frustration.
- Improved Communication: Family therapy and support groups create safe spaces for open dialogue, strengthening relationships and trust.
- Aligned Support: By involving families in care planning (with patient consent), providers help families reinforce treatment goals at home.
- Reduced Stress and Burnout: Coordinated care connects families to resources—such as counseling, respite programs, or peer support—that ease the burden of caregiving.
- Healthier Home Environment: Families learn how to set boundaries, minimize triggers, and build routines that foster stability and wellness.
- Crisis Preparedness: Families receive training on how to respond to relapse, overdose, or mental health emergencies, increasing safety and confidence.
In short, whole-person coordinated care empowers families with knowledge, support, and tools to be active partners in recovery. It transforms them from overwhelmed caregivers into informed allies, creating a stronger foundation for lasting recovery and healthier family dynamics.
Question: How can whole-person coordinated care be implemented in a clinic setting?
Answer: Implementing whole-person coordinated care in a clinic setting requires integration, collaboration, and patient-centered systems. It’s not about creating new services from scratch, but about weaving together medical, behavioral, and social supports in a structured, accessible way. Here’s how it can be done:
1. Integrated Care Teams
- Build multidisciplinary teams including medical providers, behavioral health specialists, case managers, and peer support workers.
- Hold regular case conferences to review patient progress and align treatment goals.
2. Centralized Care Coordination
- Assign a care coordinator or case manager as the primary point of contact for patients and families.
- Ensure smooth referrals between in-house services (e.g., primary care, therapy, MAT programs) and outside resources (housing, legal aid, job programs).
3. Shared Information Systems
- Use integrated electronic health records (EHRs) that allow different providers to share updates securely.
- Develop workflows that balance privacy protections with the need for communication.
4. Patient-Centered Care Planning
- Involve patients (and families, with consent) in setting recovery goals.
- Tailor care plans to include medical needs, mental health treatment, social supports, and harm reduction strategies.
5. Access to Wraparound Services
- Partner with community organizations for housing, transportation, employment, and educational support.
- Provide onsite or linked access to harm reduction tools, crisis intervention, and peer recovery coaches.
6. Training and Staff Support
- Train staff in trauma-informed care, cultural humility, and motivational interviewing.
- Offer supports to reduce provider burnout, such as team-based care models and supervision.
7. Continuous Evaluation and Quality Improvement
- Collect data on outcomes such as retention, relapse rates, and patient satisfaction.
- Use feedback to adjust programs and close care gaps.
In summary, clinics can implement whole-person coordinated care by creating integrated teams, centralizing coordination, leveraging community partnerships, and ensuring patients are active participants in their recovery. Over time, this approach reduces fragmentation, improves outcomes, and supports both patients and families more effectively.
Conclusion
Coordinated, whole-person care in addiction offers a holistic approach that can improve recovery outcomes by addressing physical, mental, and social needs simultaneously. While it provides clear advantages—such as comprehensive support and reduced relapse—it also faces challenges, including high costs, complex coordination, and potential ethical dilemmas related to autonomy, confidentiality, and resource allocation. Effective recovery depends on active self-management, strong family involvement, and the use of community resources, all of which reinforce treatment and promote long-term well-being. Despite its complexities, this integrated model remains a promising strategy for supporting individuals in sustained addiction recovery.
Video: 5 Crucial Elements of Whole Person Addiction Care You Need to Know