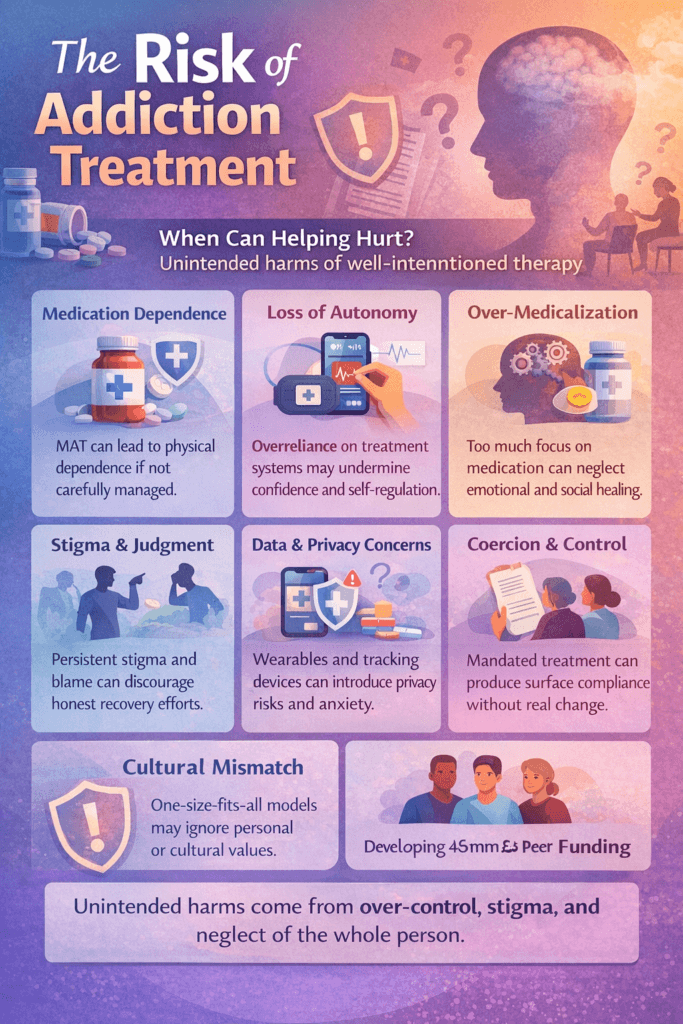
Addiction treatment aims to heal, yet even well-intentioned therapies can cause unintended harm when applied without balance, ethics, or individualized care. Over-medicalization, dependence on treatment systems, stigma, or cultural misalignment can inadvertently hinder recovery instead of supporting it. These risks underscore the need for comprehensive prevention strategies grounded in education, transparency, and compassion. Determining appropriate addiction therapy requires a multi-layered approach—where individuals engage in self-management by clarifying goals and tracking progress, families provide emotional and ethical guidance, and communities ensure equitable access and accountability. When all three levels—personal, familial, and communal—work together, treatment becomes safer, more effective, and truly person-centered.
Could Addiction Treatment Be Worse Than the Disease?
Addiction treatment has advanced dramatically, offering new hope through medication-assisted therapies (MAT), behavioral interventions, and digital innovations. These tools save lives, reduce relapse, and support long-term recovery. Yet an important ethical question remains: Could the cure ever become worse than the disease? This question challenges clinicians, communities, and individuals to examine whether modern treatments truly restore autonomy and wellness—or unintentionally replace one form of dependency, control, or harm with another. Patient-centered care, ethical reflection, and long-term evaluation are essential to ensure recovery methods heal rather than hinder.
When Treatment Becomes a New Dependency
Medications such as methadone or buprenorphine are proven to reduce overdose risk and stabilize individuals with opioid use disorder. However, they can also create long-term physical dependence. Some critics argue that extended reliance on medication may feel like trading one addiction for another. The ethical dilemma lies in deciding whether managed dependence that prevents harm is preferable to complete abstinence that carries a higher relapse risk. For many, medication is a bridge to stability—but it must be paired with opportunities for eventual independence when possible.
Over-Medicalization and Loss of Holistic Care
As addiction treatment becomes increasingly clinical, there is a risk of overlooking the emotional, social, and spiritual dimensions of recovery. Healing from addiction involves rebuilding identity, relationships, and purpose—not just correcting brain chemistry. When treatment focuses primarily on prescriptions and protocols, recovery can feel mechanical rather than human-centered. Effective care must balance medical science with psychotherapy, peer connection, and meaning-making.
Stigma, Coercion, and Control
Some individuals enter treatment through court mandates, institutional requirements, or family pressure. If treatment feels forced rather than chosen, it can mirror the loss of control experienced during addiction. Additionally, stigma persists for those using medications like Suboxone or naltrexone, even within recovery communities. Ethical care requires that treatment empower choice, dignity, and respect—not replace one form of powerlessness with another.
Emerging Technologies: Innovation or Intrusion?
Wearable monitors, virtual reality therapy, and neurostimulation tools are expanding the frontiers of relapse prevention. While promising, they also raise concerns about privacy, data security, and psychological intrusion. Continuous monitoring may feel invasive, and misuse of personal data could threaten confidentiality. Technology should enhance self-awareness and support recovery—not create surveillance or dependency.
Harm Reduction vs. Complete Recovery
Modern recovery systems increasingly embrace harm reduction, prioritizing safety and reduced risk over immediate abstinence. Critics argue this may unintentionally normalize ongoing substance use or weaken motivation for full recovery. Supporters counter that harm reduction saves lives and builds trust. The debate reflects a deeper question: Should treatment prioritize immediate safety, long-term transformation, or both? The answer likely lies in flexible, individualized care.
Conclusion
Addiction treatment is not inherently worse than the disease—but without ethical safeguards and personalized care, even well-meaning interventions can create unintended harm. The true purpose of recovery support is empowerment, not replacement. Treatment becomes problematic only when it sacrifices autonomy for control, or heals symptoms while neglecting the whole person. The future of addiction care depends on balance—uniting science, compassion, and respect for human agency so that the cure genuinely heals rather than binds.
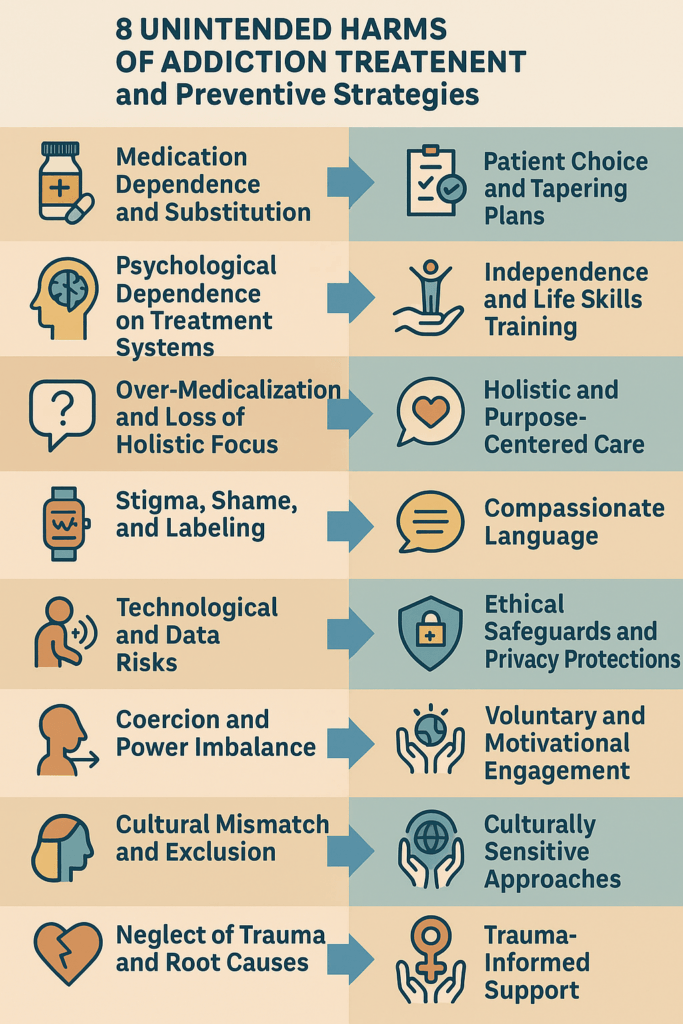
Unintended Harms in Addiction Treatment: When Help Can Miss the Mark
Addiction treatment is designed to heal, restore stability, and save lives. Yet even well-intentioned, evidence-based interventions can cause unintended harms. These harms often emerge from over-medicalization, social stigma, rigid systems, or gaps in holistic care that unintentionally distort recovery goals. Recognizing these risks does not undermine treatment—it strengthens ethical, person-centered healing.
Medication Dependence and Substitution
Medication-Assisted Treatment (MAT) with drugs like methadone or buprenorphine has dramatically reduced overdose deaths and improved stability. However, some individuals develop long-term dependence on treatment medications themselves. This can create emotional conflict about “real sobriety,” reinforce stigma, or make tapering difficult. Harm arises when treatment becomes maintenance without empowerment—controlling symptoms without building long-term self-efficacy.
Psychological Dependence on Treatment Systems
Structured programs, therapy schedules, sponsors, and monitoring tools provide essential support. But in some cases, individuals become over-reliant on external systems for regulation and approval. When independence is delayed or discouraged, individuals may struggle to transition from treatment settings to everyday life. The risk is shifting from dependence on substances to dependence on structure.
Over-Medicalization and Loss of Holistic Focus
When treatment prioritizes biology and medication over emotional healing, relationships, identity, and purpose, recovery can feel clinical rather than human. Clients may achieve physical sobriety but lack meaning, connection, or self-trust. True recovery requires both medical care and personal transformation.
Stigma, Shame, and Labeling
Stigma can persist even inside recovery spaces. Individuals using MAT may be told they are “not really sober,” and those who relapse may feel judged rather than supported. Shame discourages honesty, increases the risk of dropout, and erodes trust between clients and providers. Healing cannot thrive where judgment replaces compassion.
Technological and Data Risks
Wearables, tracking apps, and biofeedback tools introduce new ethical concerns. Constant monitoring can feel intrusive, data breaches can threaten privacy, and performance metrics may create anxiety instead of empowerment. Technology should support self-awareness—not create surveillance or fear.
Coercion and Power Imbalance
Court-mandated or forced treatment can produce surface compliance without internal motivation. When participation is driven by fear of punishment rather than desire for growth, recovery becomes performative rather than transformative. In extreme cases, control-based programs can replicate trauma dynamics rather than resolve them.
Cultural Mismatch and Exclusion
Many treatment models reflect specific cultural or spiritual assumptions that may not fit every individual. When identity, family values, or belief systems are ignored, people feel misunderstood and disengaged. Recovery must be culturally responsive to be effective.
Neglect of Trauma and Root Causes
Substance use often develops alongside trauma, mental illness, or socioeconomic hardship. When treatment focuses only on stopping substance use without addressing root drivers, relapse risk remains high. Clients may blame themselves for “failing treatment” when deeper needs were never treated.
Summary
Unintended harms in addiction treatment rarely come from bad intentions—they come from imbalance. Too much control, too little compassion. Too much symptom management, too little human understanding. Ethical and effective recovery care must restore dignity, autonomy, and connection. Treatment succeeds when it empowers individuals to reclaim their lives—rather than trading one form of dependence for another.
Self-Management Strategies for Choosing the Right Addiction Therapy
Addiction treatment offers more options than ever before — from medication-assisted therapies and behavioral counseling to holistic and technology-based approaches. While this is a major advancement, it can also feel overwhelming. The most effective recovery plans are developed when individuals actively evaluate treatment options rather than passively accept recommendations. Self-management strategies rooted in reflection, education, and collaboration help ensure that therapy aligns with personal goals, values, and readiness.
Clarify Your Personal Recovery Goals
Before beginning any therapy, define what success means to you. Some individuals prioritize complete abstinence, while others focus on reducing cravings, improving relationships, or stabilizing mental health. Writing down your top recovery goals and asking whether a proposed therapy supports long-term growth rather than short-term relief creates clarity. It is also important to distinguish goals driven by personal motivation from those influenced by external pressure. Recovery is most sustainable when it reflects your own purpose.
Educate Yourself About Treatment Options
Informed decision-making begins with knowledge. Exploring different approaches—such as medication-assisted treatment, cognitive behavioral therapy, trauma-informed care, peer recovery programs, and emerging technologies—provides perspective. Reviewing credible sources and discussing options with professionals helps you understand how each therapy addresses both physical dependence and emotional healing. Education protects against misinformation and unrealistic expectations.
Assess Risks, Benefits, and Values Alignment
Every therapy has advantages and trade-offs. Asking providers to explain potential benefits, side effects, time commitments, and ethical considerations allows you to weigh whether a treatment supports autonomy or creates unwanted dependence. Reflecting on personal values — such as independence, spirituality, privacy, or holistic wellness — helps align treatment with identity.
Seek Multiple Professional Perspectives
Addiction is complex, and no single professional holds all the answers. Consulting various specialists, such as physicians, therapists, and peer recovery coaches, provides diverse insights. Asking about treatment duration, success rates, and follow-up care provides transparency. Collective expertise leads to stronger, more confident decision-making.
Evaluate Emotional Readiness and Lifestyle Fit
A therapy can be effective only if it fits realistically into your life. Consider emotional readiness, work and family responsibilities, financial cost, and transportation. If trauma or anxiety is present, ensure the treatment includes emotional safety tools. Matching therapy demands to current capacity prevents burnout and disengagement.
Track Personal Progress and Reflection
Keeping a recovery journal to record cravings, stress levels, mood changes, and coping successes creates valuable self-data. Reviewing these reflections after several weeks helps determine whether a therapy is improving physical, emotional, and social well-being. This information empowers you to request adjustments or explore alternatives when needed.
Build a Support and Accountability Network
Sharing your decision-making process with trusted friends, family, or peer groups offers encouragement and perspective. Support systems reinforce motivation and provide honest feedback on progress. Recovery thrives in connection, not isolation.
Reassess and Stay Flexible
Recovery is a dynamic journey. What works early may need refinement later. Scheduling regular check-ins to evaluate progress and remaining open to combining or changing treatments maintains forward momentum. Adjusting direction is not failure — it is strategic self-care.
Summary
Self-management in addiction treatment means becoming an informed, empowered participant in your recovery journey. By clarifying goals, educating yourself, weighing risks, tracking progress, and seeking support, you can determine whether a therapy truly serves your healing. The right treatment is not the most popular or high-tech — it is the one that strengthens self-awareness, autonomy, and lasting growth.
Family Support Strategies for Choosing the Right Addiction Therapy
Choosing an addiction therapy is one of the most important decisions in a loved one’s recovery journey. With numerous treatment options—medical, behavioral, holistic, and technology-based—families may feel uncertain about which offers the best chance for healing. Strong family support helps ensure treatment decisions are informed, ethical, and compassionate. The goal is not to control the process but to serve as a knowledgeable ally who strengthens autonomy, trust, and long-term recovery outcomes.
Educate the Family About Treatment Options
Families make better decisions when they understand how different therapies work. Attending treatment center orientations, family education sessions, or informational workshops builds shared knowledge. Reviewing credible sources together helps distinguish evidence-based care from marketing claims. Discussing how each treatment option aligns with the loved one’s personality, mental health needs, and recovery goals ensures decisions are grounded in facts rather than fear.
Goal: Build a shared understanding before committing to therapy.
Encourage Open, Nonjudgmental Communication
A supportive home environment allows honest discussion about concerns and expectations. Asking open-ended questions, listening without interrupting, and validating emotions help loved ones feel heard rather than managed. Avoiding pressure or comparison with others’ recovery paths preserves dignity and trust.
Goal: Empower the individual to participate confidently in their treatment choice.
Assess Emotional Readiness and Life Fit
Families often notice emotional patterns and stress tolerance that may influence treatment success. Discussing whether a therapy’s intensity aligns with current emotional stability and daily responsibilities helps prevent overload. Short trial sessions or pilot programs can provide insight before committing.
Goal: Choose a therapy that aligns with both psychological readiness and real-life conditions.
Evaluate Ethical and Practical Considerations
Families play an essential role in asking critical questions about informed consent, privacy protections, data security, and follow-up care. Discussing costs, insurance coverage, and long-term affordability helps prevent financial strain. Ensuring treatment is voluntary and transparent protects autonomy and ethical integrity.
Goal: Support ethical, sustainable decision-making.
Provide Balanced Emotional Support
Recovery choices are emotional decisions. Families can offer encouragement, reinforce hope, and remind loved ones that adapting treatment plans is part of growth—not failure. Celebrating effort and progress rather than perfection builds resilience.
Goal: Strengthen motivation through compassion rather than control.
Collaborate with Professionals and Peer Networks
Joining family therapy groups, consulting multiple providers, and connecting with peer-support families provides perspective and guidance. Professional and lived-experience insight helps families understand what to expect and avoid unrealistic assumptions.
Goal: Base decisions on both clinical expertise and real-world experience.
Advocate for Community and Cultural Support
Families can help ensure treatment extends beyond clinic walls by connecting loved ones to community recovery programs, faith-based support, cultural organizations, or peer groups. When digital or technology-based therapies are proposed, families can advocate for accessibility, cultural sensitivity, and evidence-based practice.
Goal: Promote continuity of care and meaningful community integration.
Summary
Family support in evaluating addiction therapy blends education, empathy, communication, and advocacy. By staying informed, respecting autonomy, collaborating with professionals, and offering steady encouragement, families help loved ones choose treatment that aligns with emotional readiness, ethical standards, and personal values. When families act as compassionate partners rather than controllers, treatment becomes a shared path toward lasting recovery.
Community-Level Strategies for Choosing the Right Addiction Therapy
When individuals or families explore addiction treatment, the decision is rarely made in isolation. Communities play a powerful role in shaping which therapies are trusted, accessible, and recommended. Community-level strategies help ensure that treatment options are evaluated through collaboration, education, equity, and accountability, so that decisions about recovery care are informed, ethical, and sustainable rather than driven by marketing or urgency.
Collaborate with Local Health and Behavioral Agencies
Community health organizations, behavioral health boards, and recovery centers serve as trusted gatekeepers of treatment information. By connecting individuals with licensed addiction specialists for assessments or second opinions, communities help ensure that therapies align with clinical needs and recovery stages. Maintaining up-to-date directories of local detoxification programs, counseling services, medication-assisted treatment, and peer support resources helps prevent confusion and misinformation.
Goal: Base treatment decisions on verified, evidence-based guidance rather than convenience or promotion.
Provide Public Education and Awareness Campaigns
Health literacy is essential for informed recovery choices. Community seminars, webinars, town halls, and information sessions featuring clinicians, peer mentors, and families help residents understand different therapy models and what realistic outcomes look like. Distributing educational materials through schools, libraries, and faith-based centers also helps individuals recognize unethical or unregulated treatment programs.
Goal: Equip the public with knowledge to make confident, stigma-free decisions.
Engage Peer Recovery Networks
Peer recovery organizations bring lived experience into treatment evaluation. When individuals can speak directly with others who have tried different therapies, they gain realistic expectations and practical insight. Including peer specialists on advisory boards or review panels ensures that community recommendations reflect real recovery experiences rather than just clinical theory.
Goal: Center treatment guidance on lived experience and trust.
Address Equity, Access, and Funding Barriers
Even the most effective therapy fails if people cannot access it. Communities can partner with public health departments, nonprofits, and Medicaid programs to fund evidence-based care. Supporting telehealth, mobile clinics, and transportation services expands reach to rural and underserved populations. Advocacy for insurance parity laws ensures addiction treatment receives equal coverage as other medical conditions.
Goal: Guarantee fair access to quality care for all community members.
Create Interdisciplinary Evaluation Panels
Before adopting new or emerging therapies, communities benefit from interdisciplinary oversight. Panels that include physicians, addiction counselors, psychologists, ethicists, researchers, and peer advocates can evaluate safety, cultural fit, ethical standards, and outcome data. Transparent criteria for approving treatment programs protect residents from untested or exploitative services.
Goal: Maintain scientific and ethical integrity in local treatment offerings.
Incorporate Cultural and Ethical Sensitivity
Recovery support must feel relevant and respectful to diverse populations. Partnering with cultural organizations, faith leaders, and language-access services helps ensure that therapies align with community values and communication needs. Training providers in trauma-informed and culturally competent care strengthens engagement and trust.
Goal: Build an inclusive recovery ecosystem where everyone feels understood.
Collect Feedback and Monitor Outcomes
Communities thrive when they learn from experience. Anonymous surveys, public review meetings, and transparent reporting of treatment outcomes help identify what works and what needs improvement. Continuous feedback ensures programs remain accountable and responsive to community needs.
Goal: Use real-world data to refine and strengthen recovery services over time.
Summary
Community-level strategies transform addiction treatment from an individual challenge into a shared responsibility. Through collaboration, education, peer involvement, equitable access, ethical oversight, cultural inclusion, and outcome monitoring, communities can guide residents toward therapies that are not only scientifically sound but trusted, supported, and sustainable. The best recovery care is not chosen alone — it is strengthened by an informed and compassionate community.
Frequently Asked Questions
Here are some common questions:
1. What does “The Risk of Addiction Treatment” mean?
It refers to the unintended harms that can occur during addiction treatment — such as medication dependence, stigma, emotional distress, privacy risks, or loss of autonomy — even when therapies are well-intentioned and evidence-based.
2. Can addiction treatment create new dependencies?
Yes. Some treatments, especially medication-assisted therapies like methadone or buprenorphine, can cause physical dependence. While these medications save lives and reduce relapse risk, some individuals feel they are “trading one dependence for another.” Proper medical supervision and long-term recovery planning help manage this risk.
3. Is medication-assisted treatment (MAT) harmful?
MAT is widely proven to reduce overdose deaths and stabilize recovery. The risk arises only when medication is used without psychological, social, or behavioral support. Balanced treatment prevents harm and supports long-term healing.
4. Can therapy programs cause psychological harm?
In some cases, yes. Overly rigid, punitive, or trauma-insensitive programs can increase shame, anxiety, or emotional distress. Ethical, trauma-informed, and person-centered care reduces this risk.
5. Why does stigma remain a risk in treatment?
Some individuals face judgment for using medication, relapsing, or attending treatment. Stigma can discourage honesty and reduce engagement. Supportive, non-judgmental environments are essential for effective recovery.
6. Are technology-based treatments risky?
Emerging tools such as biofeedback patches, recovery apps, and virtual reality therapy can raise concerns about privacy, data security, and emotional monitoring. These tools should always include informed consent and data protection safeguards.
7. Can treatment feel controlling or coercive?
Yes. Court-mandated or pressured treatment may lead to compliance without personal motivation. Ethical care prioritizes autonomy, informed choice, and collaboration over coercion.
8. Does harm reduction encourage continued drug use?
Harm reduction focuses on safety and on reducing mortality and disease. Critics worry it may reduce motivation for abstinence, but research shows it often increases long-term engagement in recovery when combined with supportive care.
9. How can someone avoid harmful treatment experiences?
By asking questions, seeking second opinions, understanding risks and benefits, checking provider credentials, and choosing programs that respect autonomy, privacy, and holistic healing.
10. Does the risk mean treatment should be avoided?
No. Untreated addiction carries far greater risks. The goal is not to reject treatment — but to choose ethical, evidence-based, and person-centered care that minimizes unintended harm.
11. What should families watch for?
Families should watch for emotional distress, lack of consent, financial exploitation, or treatment approaches that ignore the individual’s voice. Supportive advocacy protects loved ones from harmful practices.
12. What is the safest approach to addiction treatment?
Integrated care — combining medical treatment, therapy, peer support, family involvement, and respect for personal autonomy — offers the best balance between effectiveness and safety.
Conclusion
Preventing harm in addiction treatment begins with recognizing that recovery is not a one-size-fits-all journey. Every approach—whether medical, behavioral, or technological—must align with the individual’s values, emotional readiness, and cultural context. Self-management empowers individuals to make informed choices, families strengthen trust and advocacy, and community resources safeguard ethical standards and accessibility. When these supports function in harmony, they transform potential risks into resilience. The best addiction therapy, therefore, is not merely about symptom control—it’s about restoring autonomy, dignity, and hope through informed, collaborative, and compassionate care.
Video: Treatment Starts Easy, Then This Happens #Sobriety #RealStory