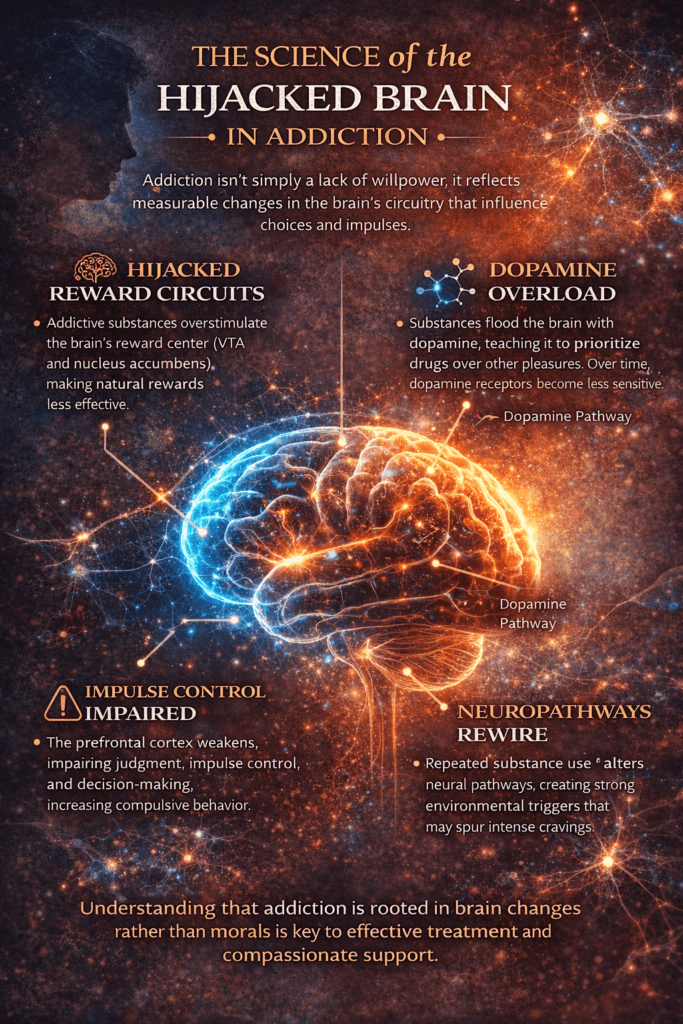
The science of the hijacked brain in addiction reveals that substance use disorders are not simply matters of willpower or poor decision-making, but conditions rooted in measurable changes within brain circuitry. Repeated exposure to addictive substances alters systems responsible for reward, motivation, stress response, and impulse control. Dopamine signaling becomes dysregulated, natural pleasures lose their impact, and environmental cues can trigger powerful cravings. These neurological shifts explain why individuals may continue using substances despite negative consequences. Understanding this science reframes addiction from a moral judgment to a medical and psychological condition, allowing individuals, families, and professionals to approach it with greater accuracy, compassion, and effectiveness.
The Science of the Hijacked Brain in Addiction: How Neurobiology Rewires Choice
Addiction is often described as a loss of control, but neuroscience reveals something more precise: a reorganization of the brain’s reward, motivation, and decision-making systems. Rather than simply choosing substances or compulsive behaviors, individuals with addiction experience measurable biological changes that influence how they perceive pleasure, stress, and consequences. Understanding the science of the “hijacked brain” reframes addiction from a moral failing to a neurobehavioral condition rooted in altered circuitry.
At the center of addiction lies the brain’s reward system, particularly dopamine signaling within pathways connecting the ventral tegmental area, nucleus accumbens, and prefrontal cortex. Under normal conditions, dopamine reinforces survival behaviors such as eating, bonding, and achieving goals. Addictive substances artificially flood this system with dopamine far beyond natural levels. Over time, the brain adapts by reducing receptor sensitivity and natural dopamine production. This process—called neuroadaptation—makes ordinary pleasures feel dull while increasing dependence on the substance for relief or motivation.
As addiction progresses, the prefrontal cortex—responsible for judgment, impulse control, and long-term planning—becomes less effective. This impairment weakens the brain’s ability to weigh consequences, resist urges, and regulate behavior. Meanwhile, the amygdala and stress circuits become more reactive, increasing anxiety, irritability, and emotional distress when the substance is absent. The result is a powerful neurological push-pull: reduced self-control combined with intensified craving.
Another key component is learning and memory. The hippocampus and related systems store strong associations between substances and environmental cues. Locations, people, emotions, or even certain times of day can trigger intense cravings because the brain has linked them with reward. These conditioned responses can persist long after substance use stops, which explains why relapse risk can remain elevated even after long periods of abstinence.
Importantly, the hijacked brain is not permanently broken. Neuroplasticity—the brain’s ability to change—allows recovery to occur. With sustained abstinence, therapy, medication when appropriate, and supportive environments, neural pathways gradually reorganize. Dopamine systems begin to stabilize, stress responses become less reactive, and cognitive control strengthens. Healing may be gradual, but it is biologically real.
Understanding addiction through neuroscience promotes compassion and evidence-based care. When we recognize that addiction alters brain function, treatment shifts from blame to intervention. The science is clear: addiction is not simply about willpower—it is about brain circuitry. Because the brain can change, recovery is not only possible but also scientifically supported.
Self-Management Strategies to Understand the Science of the Hijacked Brain in Addiction
Understanding the neuroscience of addiction can be a powerful recovery tool. When individuals learn how substances alter brain circuitry—affecting dopamine signaling, impulse control, stress responses, and decision-making—they often experience a shift in perspective. Instead of viewing addiction as a personal failure, they begin to see it as a biological condition that can be managed and healed. Self-management strategies that incorporate this scientific understanding help individuals respond to cravings, emotions, and setbacks with knowledge rather than shame.
One essential strategy is psychoeducation. Reading credible resources, attending educational therapy sessions, or participating in recovery workshops helps individuals understand how the brain’s reward system becomes overstimulated and why cravings occur. Knowledge reduces fear and confusion, allowing people to interpret urges as temporary neurological signals rather than commands that must be obeyed.
Mindful awareness is another effective approach. When a craving arises, individuals can mentally label it as a brain-based response—“This is my reward system activating”—rather than identifying with it emotionally. This cognitive distancing technique strengthens involvement of the prefrontal cortex, improving impulse regulation and decision-making.
Tracking triggers and patterns further reinforces insight. Recording when cravings occur, what emotions are present, and how they are handled transforms abstract neuroscience into practical, personal data. Over time, patterns emerge that help individuals predict high-risk situations and prepare coping responses in advance.
Cognitive reframing is also important. Instead of thinking, “I’m weak for wanting this,” individuals can reframe the thought as, “My brain is conditioned to expect this, but I can retrain it.” This shift promotes self-compassion while reinforcing personal agency.
Behavioral substitution strengthens recovery at a biological level. Engaging in exercise, creative work, social connection, or meaningful tasks stimulates the release of natural dopamine. These activities gradually retrain reward pathways, proving through experience that pleasure and motivation can exist without substances.
Consistency is key because neuroplasticity depends on repetition. The brain changes through repeated experiences, not isolated efforts. Daily practice of healthy behaviors reinforces new neural pathways and weakens conditioned responses tied to substance use.
Finally, patience is a scientific strategy. Brain healing takes time. Dopamine systems, stress circuits, and executive functioning do not normalize overnight. Recognizing recovery as a gradual neurological process prevents discouragement and supports persistence.
Self-management grounded in neuroscience transforms recovery from guesswork into informed action. By learning how addiction affects the brain and applying that knowledge intentionally, individuals gain clarity, confidence, and resilience. Understanding the hijacked brain is not just educational—it is empowering because it reveals that healing is not only possible but also biologically achievable.
Family Support Strategies to Understand the Science of the Hijacked Brain in Addiction
Understanding addiction through neuroscience can transform how families respond to a loved one’s struggles. The concept of a “hijacked brain” explains that addiction alters neural systems responsible for reward, motivation, stress response, and impulse control. These biological changes can make behaviors appear irrational or repetitive, even when the person genuinely wants to stop. When families understand this science, they shift from frustration and blame toward empathy and constructive support—an essential transition for recovery.
One of the most effective family strategies is shared education. Learning together through therapy sessions, workshops, books, or reputable medical resources helps families understand how substances affect dopamine pathways and decision-making circuits. This knowledge reframes behaviors that once seemed intentional as symptoms of altered brain function, reducing conflict and improving communication.
Another key approach is to change the language and expectations. Instead of interpreting cravings or setbacks as signs of weakness, families can recognize them as neurological signals. This perspective encourages supportive responses such as, “How can I help you through this?” rather than criticism. Compassionate language lowers stress, which directly reduces relapse risk because stress is a major trigger for cravings.
Creating a low-stress environment is also vital. Since addiction heightens sensitivity in the brain’s stress systems, chaotic or confrontational environments can intensify urges. Families who prioritize calm communication, predictable routines, and emotional safety help regulate these stress responses and support healing.
Encouraging skill-building further reinforces recovery. Families can support participation in therapy, coping-skills training, mindfulness practices, or structured activities that strengthen the prefrontal cortex—the region responsible for decision-making and impulse control. Over time, these practices help restore balance between craving signals and self-regulation.
Boundaries are another essential strategy. Understanding brain science does not mean excusing harmful behavior. Healthy boundaries protect both the individual and the family system while reinforcing responsibility and accountability. Clear expectations combined with compassion create a stable environment where recovery can grow.
Families should also care for themselves. Learning about addiction neuroscience often brings relief, but supporting someone in recovery can still be emotionally demanding. Support groups, counseling, and self-care help families maintain resilience and avoid burnout.
Family support grounded in scientific understanding becomes a powerful tool for recovery. When loved ones recognize that addiction reflects changes in brain function rather than moral failure, they respond with patience, structure, and empathy. This informed approach strengthens relationships, reduces stigma, and creates an environment that makes healing more likely.
Community Strategies to Understand the Science of the Hijacked Brain in Addiction
Addiction is often misunderstood at the societal level, leading to stigma, misinformation, and barriers to treatment. Yet neuroscience has clearly demonstrated that addiction alters brain circuitry involved in reward, motivation, stress regulation, and decision-making. When communities understand the science of the “hijacked brain,” they become more capable of supporting prevention, treatment access, and long-term recovery. Community-level strategies are essential because addiction is not only an individual issue—it is a public health issue shaped by education, culture, and available resources.
One key strategy is public education initiatives. Community workshops, school programs, healthcare seminars, and public awareness campaigns can teach how substances affect dopamine pathways, impulse control, and emotional regulation. When people learn that addiction involves biological changes rather than moral weakness, attitudes shift from blame to compassion. This change reduces stigma, making individuals more likely to seek help early.
Healthcare system integration is another critical approach. Training primary care providers, emergency personnel, social workers, and educators in addiction neuroscience ensures consistent messaging across institutions. When professionals share accurate information about how addiction affects the brain, communities receive unified, evidence-based guidance instead of conflicting narratives.
Peer-led education programs also play a powerful role. Individuals in recovery who share their experiences alongside scientific explanations help bridge the gap between theory and lived reality. Hearing both personal stories and brain-based explanations strengthens understanding and reduces misconceptions.
Community partnerships further strengthen knowledge. Collaboration among schools, treatment centers, faith organizations, and public health departments creates networks that widely distribute accurate information. Resource fairs, health screenings, and recovery awareness events allow communities to learn about addiction science in accessible, nonjudgmental environments.
Media and digital platforms can amplify these efforts. Educational videos, podcasts, infographics, and social campaigns can translate complex neuroscience into clear, relatable language. When accurate information is widely available, myths about addiction lose influence.
Finally, stigma-reduction campaigns grounded in neuroscience promote cultural change. Language matters. Communities that adopt person-first language—such as “person with substance use disorder” rather than labels—reinforce dignity and understanding. This shift supports recovery engagement and social reintegration.
Community strategies that emphasize education, collaboration, professional training, peer involvement, and stigma reduction help society understand the science behind addiction. When communities recognize that addiction reflects altered brain function rather than moral failure, they become environments that foster recovery instead of judgment. Knowledge transforms perception—and transformed perception saves lives.
Frequently Asked Questions
Here are some common questions:
1. What does “hijacked brain” mean in addiction?
It refers to the way addictive substances or behaviors alter brain circuits involved in reward, motivation, memory, and self-control. These changes can make cravings feel automatic and difficult to resist, even when a person wants to stop.
2. Which part of the brain is most affected by addiction?
Addiction primarily affects the reward pathway (including the ventral tegmental area and nucleus accumbens), the prefrontal cortex responsible for decision-making, and stress-related regions such as the amygdala.
3. Why does dopamine play such a big role?
Dopamine is a neurotransmitter that signals pleasure, motivation, and learning. Addictive substances cause unusually high dopamine surges, teaching the brain to prioritize the substance over natural rewards like food, relationships, or achievement.
4. Does addiction permanently damage the brain?
Not necessarily. While addiction can cause significant changes in brain function, the brain has neuroplasticity—the ability to heal and reorganize. With sustained recovery, many neural pathways can improve.
5. Why do cravings happen even after long periods of sobriety?
The brain stores powerful memories that link substances to pleasure or relief. Environmental cues, stress, or emotions can reactivate these pathways, triggering cravings even years later.
6. Is addiction really a disease or just a bad habit?
Scientific research shows addiction involves measurable brain changes, genetic vulnerability, and environmental influences. This supports the medical model that addiction is a chronic brain condition rather than simply a habit.
7. How does addiction affect decision-making?
Addiction weakens activity in the prefrontal cortex, which is responsible for judgment and impulse control. This makes it harder to evaluate consequences or resist urges.
8. Why do people continue using substances despite negative consequences?
Because brain circuits that prioritize reward become overactive while self-control systems weaken. The brain essentially learns that the substance is essential for survival, even when it is harmful.
9. Can understanding the brain science actually help recovery?
Yes. Learning how addiction affects the brain often reduces shame and increases motivation for treatment. It helps individuals recognize cravings as biological signals rather than personal failures.
10. What is the most hopeful scientific fact about addiction?
The brain can change. With therapy, healthy routines, medication when appropriate, and supportive environments, neural circuits can gradually stabilize. Recovery is not only possible—it is biologically supported.
Conclusion
Recognizing how addiction affects the brain transforms both treatment and perspective. The concept of a “hijacked brain” highlights that addictive behaviors arise from altered neural pathways rather than personal weakness. This knowledge reduces stigma, supports evidence-based care, and empowers individuals to engage in recovery with hope rather than shame. Importantly, neuroscience shows that the brain can heal through neuroplasticity. With sustained support, therapy, and healthy behavioral change, damaged pathways can reorganize and strengthen. Understanding the science behind addiction does more than explain the struggle—it illuminates the path forward, demonstrating that recovery is not only possible, but biologically achievable.
Video: