Dialectical Behavioral Therapy (DBT) is a dynamic therapeutic approach renowned for addressing a range of mental health challenges, including addiction, by emphasizing emotional regulation, interpersonal effectiveness, and mindfulness. Initially developed for borderline personality disorder, DBT has evolved into a versatile tool, combining cognitive-behavioral and mindfulness strategies to enhance coping skills. While offering advantages such as improved emotional regulation, DBT presents ethical dilemmas like informed consent and cultural competence. Integrating family support strategies is pivotal for optimal outcomes, highlighting the collaborative role of families in the recovery journey. This introduction explores the nuanced aspects of DBT, encompassing its uses, advantages, challenges, ethical considerations, and the crucial role of family support.
Dialectical Behavioral Therapy (DBT): A Comprehensive Approach to Addiction Recovery
Dialectical Behavioral Therapy (DBT) is a structured and evidence-based therapeutic approach that was originally developed for individuals with borderline personality disorder. Over time, its effectiveness has extended to various mental health conditions, including substance use disorders and addiction. By blending cognitive-behavioral techniques with principles of mindfulness and acceptance, DBT addresses the multifaceted challenges associated with addiction.
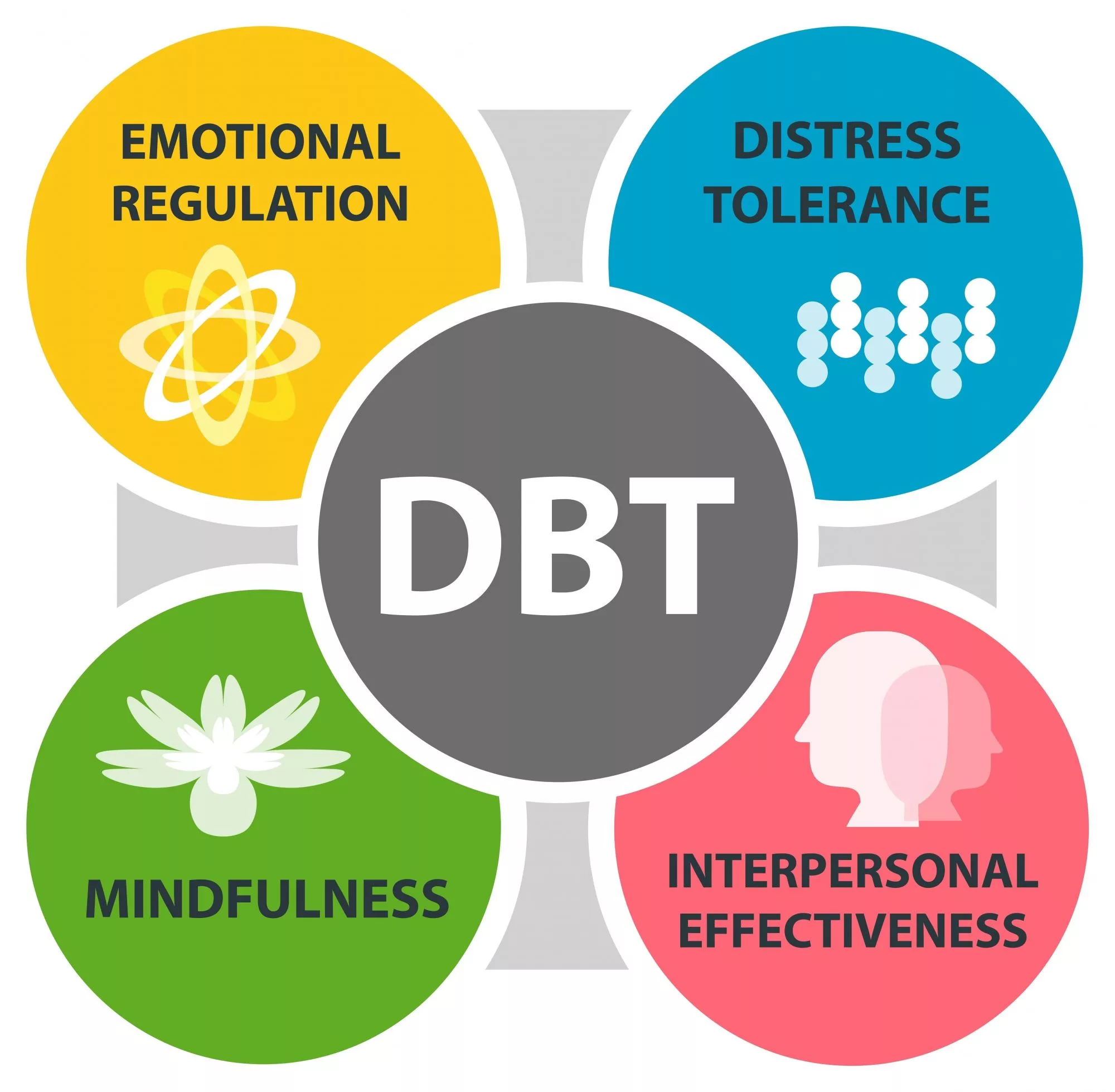
Core Components of DBT in Addiction Therapy
1. Mindfulness
Mindfulness is a cornerstone of DBT, emphasizing present-moment awareness without judgment. For individuals in recovery, mindfulness fosters the ability to observe and experience thoughts and emotions without becoming overwhelmed. This skill helps reduce impulsivity and fosters a non-reactive mindset, which is particularly beneficial for avoiding substance use triggers.
2. Distress Tolerance
Distress tolerance equips individuals with strategies to cope with crises and stress without resorting to destructive behaviors like substance abuse. By focusing on acceptance and resilience, individuals learn healthier ways to manage distress, such as self-soothing techniques, distraction methods, and crisis survival strategies.
3. Emotion Regulation
Intense emotions often contribute to substance use as a coping mechanism. DBT focuses on identifying, understanding, and regulating emotions effectively. By cultivating emotional awareness and control, individuals can decrease their vulnerability to emotional triggers and build a more balanced emotional life.
4. Interpersonal Effectiveness
Relationships and social interactions play a significant role in addiction and recovery. DBT helps individuals develop effective communication skills, assertiveness, and the ability to set and maintain healthy boundaries. Strengthening interpersonal skills reduces feelings of isolation and fosters a supportive social network that bolsters recovery.
Dialectical Principles: Balancing Acceptance and Change
DBT operates on the principle of dialectics—acknowledging and accepting current realities while simultaneously striving for positive change. This balance is particularly crucial in addiction therapy, where individuals must confront the challenges of their past while working toward a healthier future.
Effectiveness of DBT in Addiction Therapy
Research demonstrates that DBT is effective in:
- Reducing substance use.
- Enhancing emotional regulation and well-being.
- Improving interpersonal relationships.
- Supporting long-term recovery and relapse prevention.
Holistic and Tailored Approach
DBT’s integrative approach addresses the intricate interplay of addiction, mental health challenges, and interpersonal issues. By tailoring interventions to meet individual needs, therapists create a comprehensive framework that promotes sustained recovery and personal growth.
In summary, dialectical Behavioral Therapy offers a transformative approach to addiction recovery. Its focus on mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness provides individuals with the tools to navigate the complexities of addiction and build a more fulfilling, substance-free life. By combining acceptance with actionable change, DBT empowers individuals to achieve lasting recovery and improved overall well-being.
Advantages of Dialectical Behavioral Therapy (DBT) in Addiction Recovery
Dialectical Behavioral Therapy (DBT) has emerged as a highly effective and adaptable approach for addressing addiction, offering a range of benefits that make it particularly valuable in recovery. By combining evidence-based techniques with a holistic framework, DBT equips individuals with the tools needed to overcome substance use challenges.
Key Advantages of DBT in Addiction Therapy
1. Comprehensive Approach
DBT tackles multiple factors that contribute to addiction, such as emotional dysregulation, impulsivity, and interpersonal struggles. This multifaceted approach provides a thorough framework for understanding and treating the complexities of addiction.
2. Mindfulness Integration
Mindfulness practices form the core of DBT, encouraging present-moment awareness and non-judgmental acceptance. These skills help individuals manage cravings, reduce impulsive reactions, and enhance overall emotional well-being, fostering resilience in recovery.
3. Emotion Regulation
Many individuals turn to substances to cope with intense emotions. DBT equips them with tools to identify, understand, and regulate their emotions, reducing the emotional triggers that can lead to substance use.
4. Interpersonal Effectiveness
Social connections often play a crucial role in recovery. DBT enhances communication, assertiveness, and boundary-setting skills, helping individuals build and maintain healthier relationships. This can reduce feelings of isolation and create a more supportive recovery environment.
5. Distress Tolerance
One of DBT’s key components is teaching strategies for coping with distress without resorting to maladaptive behaviors like substance use. These skills are essential for navigating high-stress situations and preventing relapse.
6. Individualized Treatment
DBT’s flexibility allows therapists to tailor interventions to address specific concerns for each client. This personalized approach ensures that therapy is both relevant and effective for the individual’s unique challenges and goals.
7. Research-Based Effectiveness
Supported by extensive empirical research, DBT has proven effective in treating addiction and co-occurring mental health issues. Its evidence-based framework gives clients and therapists confidence in its application and potential for positive outcomes.
8. Dialectical Approach
DBT embraces a dialectical perspective, balancing acceptance of the present with a commitment to change. This dual focus helps individuals develop a balanced mindset, fostering self-compassion while actively working toward a healthier, substance-free life.
9. Holistic Treatment
Recognizing the interconnectedness of mental health, emotional regulation, and relationships, DBT provides a holistic approach to treatment. This comprehensive perspective addresses the diverse factors that influence addiction and recovery.
10. Relapse Prevention
DBT’s emphasis on distress tolerance, emotion regulation, and mindfulness equips individuals with the skills needed to manage triggers and stressors, reducing the likelihood of relapse and supporting long-term recovery.
Dialectical Behavioral Therapy offers a well-rounded and research-supported approach to addiction recovery. Its focus on mindfulness, emotional regulation, and interpersonal skills provides individuals with the tools to navigate the challenges of recovery effectively. By addressing the root causes of addiction and fostering resilience, DBT paves the way for sustained recovery and improved quality of life.
Challenges and Disadvantages of Dialectical Behavioral Therapy (DBT) in Addiction Treatment
While Dialectical Behavioral Therapy (DBT) is widely regarded as an effective approach for addiction therapy, it is essential to recognize that it may not be the ideal fit for everyone. Below are some potential disadvantages and challenges associated with DBT in the context of addiction treatment:
Key Challenges of DBT
1. Time-Intensive
DBT typically requires a significant time investment, including individual therapy sessions, group skills training, and phone coaching. For individuals with demanding schedules or logistical constraints, this commitment may be difficult to sustain.
2. Structured Format
The highly structured nature of DBT, while beneficial for many, may not resonate with everyone. Some individuals prefer a more flexible or exploratory approach to therapy and may find DBT’s format overly prescriptive.
3. Limited Access to Therapists
Access to qualified DBT practitioners can be a challenge, especially in rural or less populated areas. This scarcity of trained therapists may limit the availability of DBT as a treatment option for many individuals.
4. High Level of Commitment Required
DBT requires consistent attendance and active participation in therapy sessions and skill-building activities. For individuals who struggle with motivation or face barriers such as transportation or childcare, maintaining this level of commitment can be difficult.
5. Suitability for Specific Diagnoses
While DBT has proven effective for a range of mental health conditions, it may not be the best fit for every diagnosis or individual. Some may find other therapeutic modalities more aligned with their needs and treatment goals.
6. Cognitive Demands
DBT involves learning new skills and applying them in real-life situations, which can be challenging for individuals with cognitive impairments or learning difficulties. This aspect of DBT may require additional support and adaptation to ensure accessibility.
7. Not a Quick Fix
DBT is a gradual process that focuses on building skills and fostering long-term change. Individuals seeking immediate relief may feel frustrated with the time it takes to see tangible results.
8. Challenges with Group Settings
Group skills training is a cornerstone of DBT, but not everyone is comfortable in group environments. Group dynamics can be challenging, and some individuals may struggle to share personal experiences or engage fully in this setting.
9. Resource-Intensive
The implementation of DBT often requires extensive resources, including trained therapists and organizational support. These resource demands can pose barriers to adopting DBT in underfunded or resource-limited settings.
10. Potential Overemphasis on Skills
In some cases, DBT may focus heavily on skill acquisition while insufficiently addressing the deeper, underlying issues contributing to addiction. This could limit the therapy’s ability to address root causes comprehensively.
Dialectical Behavioral Therapy offers a powerful framework for addressing addiction and related mental health challenges. However, it is essential to weigh these potential disadvantages against its benefits when considering its use. Individual preferences, diagnoses, and access to resources should play a critical role in determining the suitability of DBT for each person. With proper adaptation and support, DBT can remain an invaluable tool in addiction therapy despite its challenges.
Ethical Considerations in Dialectical Behavioral Therapy (DBT)
While Dialectical Behavioral Therapy (DBT) is widely recognized as an ethical and evidence-based therapeutic approach, it is not without its ethical complexities. Therapists practicing DBT must navigate a range of considerations to ensure they uphold professional standards and prioritize client well-being. Below are some of the potential ethical dilemmas associated with DBT:
Key Ethical Concerns in DBT
1. Informed Consent
Due to the structured nature of DBT, ensuring clients fully understand the therapy process is critical. Informed consent involves explaining the components of DBT—such as individual therapy, group skills training, and phone coaching—as well as potential risks and benefits. Therapists must provide this information clearly and comprehensively to support client autonomy.
2. Confidentiality in Group Settings
Group skills training is a core component of DBT, but maintaining confidentiality within a group setting can be challenging. Therapists must establish clear rules and educate participants about the limits of confidentiality, emphasizing the importance of mutual respect and discretion within the group.
3. Therapist Competence
DBT requires specialized training to ensure effective delivery. Ethical concerns arise when therapists practice DBT without adequate training or experience. Therapists must commit to continuous professional development and adhere to standards of competence in providing DBT interventions.
4. Cultural Competence
Therapists must be culturally aware and sensitive to the diverse backgrounds of their clients. Delivering DBT without considering cultural nuances can lead to misunderstandings or the imposition of inappropriate values. Tailoring interventions to align with the client’s cultural context is essential for ethical practice.
5. Balancing Structure with Client Autonomy
The structured framework of DBT may conflict with the principle of client autonomy if therapists impose their strategies without adequate collaboration. Ethical practice requires involving clients in decision-making and respecting their preferences and goals throughout therapy.
6. Applicability to Diagnoses
While DBT has proven effective for specific conditions such as borderline personality disorder and addiction, it may not be suitable for everyone. Therapists have an ethical obligation to assess the appropriateness of DBT for each client and ensure it aligns with their unique needs and challenges.
7. Resource Allocation
DBT is resource-intensive, often requiring trained therapists, group sessions, and organizational support. Ethical concerns arise when limited resources result in inequitable access to DBT services. Therapists and organizations must strive to allocate resources fairly and consider alternative solutions for underserved populations.
8. Managing Suicidal Ideation
DBT is frequently used for individuals with suicidal ideation. Balancing the ethical duty to protect clients from harm while respecting their autonomy and confidentiality can be complex. Therapists must carefully assess and document risks while maintaining a supportive therapeutic relationship.
9. Maintaining Professional Boundaries
Clear boundaries are essential to prevent ethical dilemmas and ensure a professional therapist-client relationship. Therapists must remain vigilant to avoid boundary violations, which can compromise the integrity of therapy.
10. Evaluating Treatment Outcomes
Regularly evaluating the effectiveness of DBT interventions is an ethical responsibility. Failing to monitor progress or adjust treatment plans when necessary can undermine the client’s therapeutic experience and outcomes.
Practicing Dialectical Behavioral Therapy ethically requires therapists to navigate a range of challenges, from ensuring informed consent to addressing cultural competence and maintaining professional boundaries. Regular supervision, ongoing training, and adherence to professional codes of ethics are essential to mitigating these dilemmas and fostering a therapeutic environment that prioritizes client well-being and respect. By addressing these ethical considerations thoughtfully, DBT practitioners can uphold the highest standards of care and support positive outcomes for their clients.
Enhancing Family Support in Dialectical Behavioral Therapy (DBT)
Family support plays a vital role in Dialectical Behavioral Therapy (DBT), providing a foundation for individuals to navigate the challenges of emotional regulation, interpersonal relationships, and recovery. By actively involving family members in the therapeutic process, DBT can create a more supportive and collaborative environment. Below are strategies to enhance family support within the DBT framework:
Strategies for Family Involvement in DBT
1. Education and Training
Providing family members with education about DBT principles is a crucial first step. Explaining the structure of therapy, such as individual sessions, group skills training, and the core modules of DBT, helps families understand how the therapy works. Training them in basic DBT skills enables families to better support their loved one’s progress.
2. Inclusion in Treatment
Encouraging family participation in aspects of treatment, such as family therapy sessions or skills training groups, fosters a sense of collaboration. By being actively involved, family members gain insights into the therapeutic process and contribute meaningfully to the individual’s journey.
3. Communication Skills Training
Teaching effective communication techniques to family members can reduce conflict and improve understanding within the family unit. Skills such as active listening, expressing emotions constructively, and using “I” statements are integral to creating a more harmonious environment.
4. Setting Boundaries
Helping families establish and maintain healthy boundaries prevents over-involvement (enmeshment) or detachment. Understanding the importance of boundaries supports healthier relationships and allows each family member to focus on their roles and responsibilities.
5. Practicing Mindfulness Together
Introducing mindfulness practices to the entire family promotes shared emotional regulation and stress reduction. Practicing mindfulness together can strengthen bonds and help family members manage their own emotions effectively.
6. Using Validation Techniques
Teaching family members how to validate their loved one’s experiences—even when they don’t agree—fosters empathy and improves communication. Validation helps individuals feel heard and understood, reducing emotional distress.
7. Collaborative Problem-Solving
Encouraging families to solve problems collaboratively strengthens their ability to navigate challenges together. Joint problem-solving sessions can help address practical issues while building a sense of shared responsibility and support.
8. Supporting Caregivers
Recognizing the emotional and physical toll on family caregivers is essential. Providing resources, support groups, and opportunities for respite ensures that caregivers maintain their own well-being, enabling them to continue supporting their loved one.
9. Teaching Emotional Regulation Tools
Equipping family members with tools to manage their own emotions positively influences the overall family atmosphere. When family members regulate their emotions effectively, they serve as role models and create a calmer environment.
10. Regular Family Meetings
Scheduling regular family meetings to discuss progress, challenges, and goals fosters open communication. These meetings ensure alignment and strengthen the family’s collective commitment to the individual’s recovery.
11. Celebrating Progress
Recognizing and celebrating milestones or achievements—no matter how small—reinforces positive behaviors and creates a motivating atmosphere. This shared sense of accomplishment boosts the individual’s commitment to DBT.
12. Addressing Stigma
Challenging stigma and misconceptions about mental health and addiction within the family is essential. Promoting a supportive and nonjudgmental attitude helps create an environment conducive to healing and recovery.
Incorporating family support strategies into Dialectical Behavioral Therapy acknowledges the vital role families play in recovery. By fostering collaboration, teaching skills, and addressing emotional dynamics, these strategies strengthen the overall effectiveness of DBT. Tailoring the approach to the specific needs and dynamics of each family ensures the best outcomes, contributing to sustained recovery and a healthier family system.
Frequently Asked Questions
Here are some common questions:
1. What is Dialectical Behavior Therapy (DBT)?
DBT is an evidence-based psychotherapy originally developed to treat intense emotional dysregulation. It is now widely used for addiction, especially when substance use is driven by strong emotions or trauma.
2. Why is DBT effective for addiction treatment?
DBT helps individuals manage overwhelming emotions, reduce impulsive behaviors, and build healthy coping skills that replace substance use.
3. What types of addiction does DBT help treat?
DBT is effective for alcohol, opioid, stimulant, nicotine, cannabis, and behavioral addictions, particularly when co-occurring with mood disorders or trauma.
4. How does DBT address cravings?
DBT teaches distress-tolerance and emotion-regulation skills to help individuals ride out cravings without acting on them.
5. What are the four main skill areas in DBT?
Mindfulness, Distress Tolerance, Emotion Regulation, and Interpersonal Effectiveness.
6. How does mindfulness help addiction recovery?
It increases awareness of thoughts, emotions, and urges, creating space to choose healthier responses instead of impulsive use.
7. What is distress tolerance in DBT?
Distress tolerance skills help individuals survive emotional pain without making the situation worse through substance use.
8. How does emotion regulation reduce addiction risk?
It teaches how to understand emotions, reduce vulnerability to emotional extremes, and increase positive experiences.
9. How does interpersonal effectiveness support recovery?
It strengthens communication, boundary-setting, and relationship stability, reducing relational triggers for substance use.
10. What happens in a DBT addiction therapy session?
Sessions include skills training, behavior tracking, crisis planning, and real-life application of coping strategies.
11. Can DBT be combined with medication-assisted treatment?
Yes. DBT works well alongside medications and medical addiction care.
12. Is DBT helpful for trauma-related addiction?
Yes. DBT is especially effective for individuals with trauma histories and emotional sensitivity.
13. How long does DBT treatment last?
Standard programs last 6–12 months, though shorter formats exist.
14. Does DBT reduce relapse?
Yes. Studies show DBT lowers relapse rates by improving emotional control and stress tolerance.
15. What is the biggest benefit of DBT in addiction recovery?
It teaches people how to live with difficult emotions without escaping through substances.
Conclusion
Dialectical Behavioral Therapy (DBT) emerges as a dynamic and adaptable therapeutic modality with substantial potential for addressing diverse mental health challenges, including addiction. Its emphasis on emotional regulation, mindfulness, and interpersonal effectiveness underscores its holistic approach to well-being. While DBT offers notable advantages such as improved coping skills and enhanced emotional regulation, it is essential to navigate its inherent challenges, including ethical dilemmas surrounding consent and cultural competence. Moreover, the integration of family support strategies enhances the therapeutic landscape, recognizing the vital role families play in the recovery process. DBT stands as a comprehensive and effective approach, showcasing the significance of collaboration, cultural sensitivity, and tailored family involvement in achieving positive outcomes in the realm of mental health and addiction recovery.
Video: