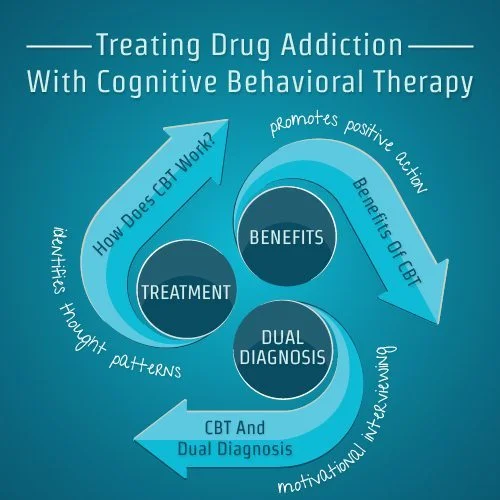
Cognitive Behavioral Therapy (CBT) is a pivotal approach in addiction therapy, adept at addressing the intricate dynamics of substance use disorders by targeting thought patterns and behaviors. Renowned for its adaptability and evidence-based efficacy, CBT guides individuals in understanding and transforming maladaptive habits. While its advantages include goal-oriented focus and versatility, ethical dilemmas may emerge, necessitating careful consideration. Recognizing the significance of family support in the recovery process, CBT integrates strategies to educate and engage family members. This exploration delves into the diverse facets of CBT in addiction therapy, encompassing applications, merits, challenges, and the vital role of family support on the journey to recovery.
Understanding Cognitive Behavioral Therapy (CBT): A Transformative Approach to Mental Health
Cognitive Behavioral Therapy (CBT) is one of the most widely recognized and evidence-based forms of psychotherapy. Built on the principle that thoughts, feelings, and behaviors are interconnected, CBT empowers individuals to identify and modify negative thought patterns and behaviors that contribute to emotional distress and dysfunctional actions.
This structured, goal-oriented, and typically short-term therapeutic approach is effective for addressing a range of mental health issues, including anxiety disorders, depression, phobias, and addiction. By focusing on present challenges rather than delving extensively into past experiences, CBT offers practical strategies for creating meaningful and lasting changes.
How CBT Works
CBT operates on the premise that:
- Thoughts Influence Emotions and Behaviors: Negative thought patterns can lead to emotional distress and maladaptive behaviors.
- Identifying and Challenging Negative Thoughts: Recognizing and reframing irrational or unhelpful thoughts can transform emotional responses and actions.
- Behavioral Change Enhances Well-being: Positive changes in behavior can reinforce healthier thought patterns, creating a cycle of improvement.
Core Components of CBT
- Identifying Negative Thought Patterns:
- Therapists guide individuals in recognizing automatic thoughts that contribute to their emotional struggles.
- These thoughts often stem from cognitive distortions, such as catastrophizing, black-and-white thinking, or overgeneralization.
- Challenging and Reframing Thoughts:
- Individuals learn to question the validity of their negative thoughts and replace them with more balanced and constructive perspectives.
- Behavioral Activation:
- Engaging in positive, goal-oriented activities helps individuals combat patterns of avoidance and inactivity.
- Developing Coping Strategies:
- CBT equips individuals with practical tools to manage stress, anxiety, and other challenges effectively.
- Collaborative and Transparent Process:
- CBT is a partnership between the therapist and the individual. Together, they set goals, track progress, and refine strategies to achieve desired outcomes.
Applications of CBT
CBT is highly versatile and can be adapted to address various mental health concerns, including:
- Anxiety Disorders: Helping individuals manage excessive worry and irrational fears.
- Depression: Encouraging engagement in rewarding activities and addressing negative self-perceptions.
- Addiction: Supporting individuals in breaking the cycle of substance use by identifying triggers and developing healthier coping mechanisms.
- Phobias and OCD: Reducing avoidance behaviors and challenging intrusive thoughts.
Why Choose CBT?
- Evidence-Based: Supported by extensive research, CBT has demonstrated effectiveness across diverse populations and conditions.
- Structured and Goal-Oriented: The focused nature of CBT makes it ideal for individuals seeking tangible outcomes within a defined timeframe.
- Empowers Individuals: By fostering self-awareness and equipping individuals with tools for self-management, CBT encourages long-term resilience.
Cognitive Behavioral Therapy is more than just a treatment—it’s a transformative process that enables individuals to reclaim control over their mental health and well-being. Through collaboration with skilled therapists, individuals can reframe negative thoughts, adopt healthier behaviors, and build a brighter future grounded in resilience and self-awareness. Whether addressing specific challenges or striving for personal growth, CBT offers a pathway to lasting change.
The Advantages of Cognitive Behavioral Therapy (CBT): Why It’s a Preferred Choice in Mental Health Care
Cognitive Behavioral Therapy (CBT) stands out as a leading approach in mental health treatment due to its practicality, adaptability, and proven effectiveness. Its structured nature and evidence-based foundation make it a valuable tool for addressing a variety of psychological challenges. Here’s a closer look at why CBT is widely regarded as a top therapeutic method.
Key Advantages of CBT
- Empirical Support
- CBT is one of the most extensively researched forms of psychotherapy, with a robust body of evidence validating its effectiveness for various mental health conditions. Its scientific backing instills confidence in its reliability and outcomes.
- Focused and Goal-Oriented
- The structured and goal-driven framework of CBT makes it highly efficient for addressing specific issues. By setting clear objectives, individuals can work toward tangible outcomes within a defined timeframe.
- Identifies and Restructures Negative Thought Patterns
- CBT enables individuals to recognize and challenge distorted thought patterns. By replacing these with healthier perspectives, clients experience improved emotional and behavioral responses, fostering overall well-being.
- Practical Coping Strategies
- CBT emphasizes the development of actionable coping techniques to manage stress, anxiety, and other challenges effectively. These skills empower individuals to face life’s obstacles with greater resilience.
- Collaborative Approach
- The partnership between therapist and client is central to CBT. Together, they identify problems, set goals, and craft strategies for change, creating a sense of involvement and ownership in the recovery process.
- Versatility Across Disorders
- CBT is effective for a broad range of mental health conditions, including anxiety, depression, phobias, post-traumatic stress disorder (PTSD), and substance use disorders. Its adaptability makes it a go-to treatment for diverse needs.
- Present-Focused
- Unlike some therapies that delve into past experiences, CBT primarily targets current thoughts and behaviors. This focus on the present makes it practical and relevant, addressing immediate challenges and concerns.
- Skill-Building for Independence
- CBT equips individuals with lifelong skills to manage their thoughts, emotions, and actions. These tools foster independence and provide resilience against future setbacks, contributing to sustained mental health.
- Active Client Engagement
- Clients in CBT often engage in activities like homework assignments and self-monitoring exercises. This active participation extends the benefits of therapy beyond sessions and reinforces progress.
- Adaptability to Individual Needs
- CBT’s flexible framework allows therapists to tailor the approach to each client’s unique challenges, ensuring that therapy is personalized and effective.
- Brief and Cost-Effective
- CBT’s structured, time-limited format often yields significant results in a shorter duration compared to other therapeutic methods. This efficiency makes it an accessible and affordable option for many.
Cognitive Behavioral Therapy has earned its reputation as a gold standard in psychotherapy due to its practicality, adaptability, and proven results. Its ability to empower individuals with skills for managing their mental health independently, combined with its focus on present-day challenges, makes it an invaluable tool for recovery and growth. Whether addressing specific disorders or promoting general well-being, CBT offers a pathway to meaningful and lasting change.
Recognizing the Potential Disadvantages of Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is widely celebrated for its effectiveness and versatility in treating various mental health conditions. However, like any therapeutic approach, it has certain limitations that may affect its suitability for specific individuals or situations. Understanding these potential drawbacks can help ensure that therapy is tailored to meet individual needs effectively.
Key Disadvantages of CBT
- May Not Address Underlying Causes
- CBT often focuses on addressing present issues rather than delving deeply into past experiences or underlying causes. For individuals dealing with complex, deeply rooted psychological issues, additional exploration may be required.
- Not Suitable for Everyone
- Some individuals may prefer approaches that prioritize emotional depth or an exploration of past experiences. CBT’s structured, cognitive focus may not resonate with everyone.
- Requires Active Participation
- CBT heavily relies on the individual’s active engagement. Success is tied to the willingness to participate fully in sessions and complete assignments. For those unmotivated or struggling with commitment, this may pose a challenge.
- May Oversimplify Complex Issues
- The premise that changing thoughts leads to changes in emotions and behaviors can sometimes oversimplify the intricacies of certain psychological challenges, especially those with roots in traumatic or multifaceted experiences.
- Potential for Superficial Treatment
- The structured, goal-oriented nature of CBT can occasionally lead to superficial treatment, addressing immediate symptoms without deeply exploring a person’s broader life experiences or challenges.
- Focus on Symptom Reduction
- While effective for managing symptoms, CBT may not prioritize personal growth or self-discovery. Individuals seeking a more holistic or exploratory therapeutic experience may find it limiting.
- May Not Suit Cultural Differences
- CBT’s emphasis on cognitive restructuring may not align with cultural values that focus more on collective or contextual factors. Adapting CBT to respect cultural differences is crucial for its effectiveness.
- Limited Effectiveness for Severe Mental Illness
- Although CBT is beneficial for various mental health conditions, its effectiveness may be limited when dealing with severe mental illnesses. In such cases, it is often used as part of a broader, integrated treatment plan.
- Homework and Time Commitment
- Regular practice and homework assignments are integral to CBT. For individuals with limited time or those who struggle with consistency, this can be a significant barrier to success.
- May Not Address Interpersonal Dynamics
- CBT primarily focuses on the individual’s thoughts and behaviors, potentially overlooking interpersonal or relational issues that contribute to the problem. Therapies that focus on relationships might be more appropriate in such cases.
While CBT is an evidence-based and highly effective therapeutic approach, it is not a one-size-fits-all solution. Understanding its potential limitations ensures that individuals and therapists can make informed decisions about its appropriateness based on the individual’s unique needs and goals. In some cases, combining CBT with other modalities or tailoring its application can provide a more comprehensive and personalized approach to mental health care.
Ethical Considerations in Cognitive Behavioral Therapy (CBT): Navigating Common Dilemmas
Cognitive Behavioral Therapy (CBT) is widely recognized for its effectiveness and structured approach in addressing various mental health concerns. However, like all therapeutic modalities, it is not without its ethical challenges. Therapists practicing CBT must be prepared to navigate these dilemmas while upholding the highest ethical standards.
Key Ethical Considerations in CBT
- Informed Consent
- Therapists must ensure clients fully understand the nature, goals, and potential risks of CBT. Communicating these concepts effectively can be challenging, particularly with vulnerable populations or individuals with cognitive impairments.
- Cultural Competence
- CBT interventions should respect and reflect the client’s cultural background. Ethical dilemmas may arise when therapists lack cultural sensitivity, potentially leading to misinterpretations or interventions that do not align with the client’s values.
- Confidentiality
- Protecting client confidentiality is a cornerstone of ethical practice. However, dilemmas emerge when therapists encounter situations involving potential harm to the client or others, requiring careful deliberation about breaching confidentiality.
- Client Autonomy
- CBT emphasizes collaboration, but ethical challenges can arise if clients feel pressured to conform to the therapist’s agenda. Ensuring genuine consent and respecting client autonomy are critical for ethical practice.
- Dual Relationships
- Therapists must avoid dual relationships that can compromise professional boundaries. This can be especially challenging in small communities or when working with multiple family members, requiring careful ethical navigation.
- Competence and Training
- Delivering effective CBT requires appropriate training and competence. Ethical concerns arise when therapists work outside their areas of expertise or employ techniques for which they are not adequately trained.
- Potential Harm
- While CBT aims to foster positive change, there is a risk of harm if the therapy is ineffective or if therapists address issues beyond their scope of expertise. Ethical practice involves recognizing these risks and responding appropriately.
- Inequality in Access
- Barriers such as socioeconomic factors, geographic location, or systemic inequities can limit access to CBT. Addressing these disparities is an ethical responsibility for therapists and the broader mental health community.
- Therapist Bias
- Therapists must be aware of their biases and how these may influence the therapeutic process. Failing to acknowledge and address personal biases can compromise the quality and fairness of care.
- Ongoing Assessment
- Regularly assessing the effectiveness of CBT interventions is an ethical obligation. If a client is not making progress, therapists must reevaluate the treatment plan and consider alternative approaches to ensure the client’s well-being.
In summary, ethical practice is integral to providing effective and responsible CBT. By prioritizing informed consent, cultural competence, and ongoing assessment, therapists can navigate ethical dilemmas while maintaining their clients’ best interests. Regular supervision, adherence to professional ethical codes, and a commitment to ongoing learning are essential for upholding these standards and delivering high-quality care.
Enhancing Cognitive Behavioral Therapy (CBT) Through Family Support Strategies
Family support plays a crucial role in Cognitive Behavioral Therapy (CBT), particularly when addressing issues that involve or impact the entire family. Incorporating family members into the therapeutic process can enhance the effectiveness of CBT and contribute to long-term positive outcomes. Here are some strategies to integrate family support into CBT:
1. Psychoeducation for Family Members
Educating family members about the client’s mental health condition and the principles of CBT helps demystify the therapeutic process. By gaining a better understanding of the client’s challenges and the goals of therapy, families can provide informed and empathetic support.
2. Involving Family in Treatment Goals
Collaboratively setting goals that involve the entire family fosters a sense of shared responsibility and strengthens familial bonds. When the family participates in defining and supporting therapeutic objectives, the client benefits from a more unified and encouraging environment.
3. Communication Skills Training
CBT can equip families with effective communication techniques, such as active listening, expressing emotions constructively, and resolving conflicts. Improved communication enhances understanding and cooperation within the family, contributing to a healthier dynamic.
4. Behavioral Interventions at Home
Reinforcing CBT principles in the family setting helps solidify progress made in therapy. Families can learn and implement behavior modification techniques, providing consistent support for managing challenges and practicing positive behaviors at home.
5. Family Therapy Sessions
Integrating family therapy sessions alongside individual CBT sessions can address interpersonal conflicts and dynamics. These sessions create a safe space for open communication and collaborative problem-solving, promoting family cohesion.
6. Boundary Setting
CBT can help families establish and respect healthy boundaries, which are essential for maintaining trust and security. Clear boundaries prevent enmeshment and encourage each family member to take responsibility for their emotional well-being.
7. Positive Reinforcement for Supportive Behaviors
Recognizing and rewarding family members who actively contribute to the client’s therapeutic journey reinforces positive behavior. Celebrating milestones and expressing gratitude strengthens the collaborative relationship within the family.
8. Conflict Resolution Strategies
CBT can teach families effective methods for resolving conflicts constructively. Learning problem-solving skills and techniques to manage disagreements reduces tension and supports the overall well-being of the family unit.
9. Encouraging Empathy and Understanding
Through CBT, family members can gain insight into the client’s perspective and challenges. Developing empathy reduces judgment or stigma associated with mental health issues, fostering a supportive and compassionate environment.
10. Mindfulness Practices for the Family
Introducing mindfulness practices can help reduce stress and improve emotional regulation for all family members. Simple mindfulness exercises integrated into daily routines enhance overall family resilience and connection.
11. Family Involvement in Relapse Prevention
Including family members in relapse prevention planning ensures a comprehensive approach to sustaining progress. Families can help identify triggers, provide accountability, and assist in implementing coping strategies during challenging times.
In summary, the integration of family support strategies within CBT underscores the interconnectedness of individual and family well-being. By involving family members in the therapeutic process, CBT not only addresses the individual’s needs but also strengthens the family’s ability to function as a cohesive and supportive unit. This collaborative approach enhances the likelihood of sustained success and long-term positive outcomes.
Conclusion
Cognitive Behavioral Therapy (CBT) remains a pivotal force in addiction therapy, wielding its effectiveness through a systematic and goal-oriented approach. The model’s adaptability and evidence-based foundations contribute to its widespread application, empowering individuals to comprehend and modify detrimental patterns. Despite its merits, ethical considerations surface, emphasizing the need for practitioners to navigate issues of informed consent and confidentiality with diligence. As we reflect on the multifaceted nature of CBT, its integration of family support strategies emerges as a crucial element, acknowledging the profound impact of familial involvement on the path to recovery. In the complex landscape of addiction, CBT stands not only as a therapeutic tool but as a beacon illuminating the collaborative journey toward sustained healing and well-being.