Addiction care during pregnancy requires a careful balance of medical safety, emotional support, and compassionate, evidence-based treatment. Pregnancy can serve as a powerful catalyst for recovery, inspiring many women to seek help for the first time; however, it also introduces significant physical changes, emotional vulnerability, and social pressures that can complicate substance use disorders. Effective addiction care recognizes substance use disorder as a chronic and treatable health condition rather than a moral failing, reducing shame and encouraging honest engagement in treatment. Early screening, medical stabilization, trauma-informed counseling, and coordinated prenatal care are essential in protecting both maternal health and fetal development. When healthcare providers integrate addiction treatment with obstetric services, they not only reduce risks such as preterm birth, withdrawal complications, and developmental harm, but also build trusting relationships that motivate expecting mothers to remain in care. By replacing stigma with support and punishment with partnership, addiction care during pregnancy creates a foundation for healthier pregnancies, safer deliveries, and long-term recovery for mothers and their children.
Addiction Care During Pregnancy: Evidence-Based
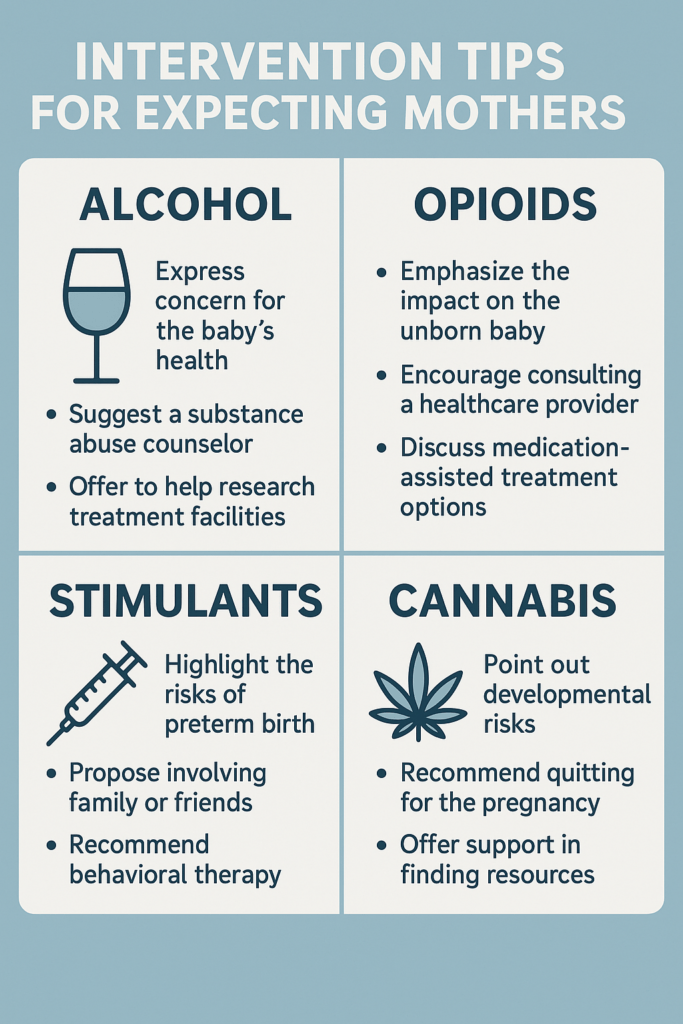
Intervention Tips for Expectant Mothers
Substance use during pregnancy presents complex medical, emotional, and social challenges that
require compassionate, evidence-based care. Expectant mothers with addiction need specialized
interventions that protect fetal development while supporting maternal recovery without stigma or
punishment. Effective addiction care during pregnancy focuses on early screening, medical
stabilization, trauma-informed support, and coordinated prenatal treatment. Because each substance
carries unique risks to both mother and baby, intervention strategies must be tailored by addiction type
while also addressing housing stability, mental health, family involvement, and postpartum planning.
The following guide outlines intervention tips for expecting mothers affected by different forms of
addiction, organized by substance and focused on health, prenatal safety, and long-term recovery
support.
- Alcohol Use
Early screening using standardized tools at prenatal visits. Encourage open discussion about alcohol use and fetal risks, including Fetal Alcohol Spectrum Disorders. Connect mothers to specialized perinatal addiction treatment programs. Provide folic acid, thiamine, and prenatal vitamins to address nutritional deficiencies. Educate family members about maintaining an alcohol-free home environment. - Opioid Use (Heroin, Prescription Painkillers, Fentanyl)
Offer medication-assisted treatment with buprenorphine or methadone under prenatal supervision, as
sudden withdrawal increases miscarriage and preterm labor risk. Apply trauma-informed care to reduce
stigma. Integrate obstetrics, addiction medicine, and social services. Educate families about Neonatal
Abstinence Syndrome and post-delivery care planning. Maintain treatment after delivery to reduce
relapse risk. - Nicotine (Cigarettes and Vaping)
Use behavioral counseling as first-line treatment. Consider supervised nicotine replacement therapy
when counseling alone is insufficient. Remove smoking triggers and encouragea smoke-free
environments. Teach breathing, mindfulness, and prenatal relaxation techniques for stress
management. - Cannabis Use
Explain the risks, including low birth weight and potential neurodevelopmental effects. Offer safer coping options for nausea, anxiety, and sleep. Encourage honest disclosure through supportive, non-punitive care. Conduct monitoring only when clinically indicated and with informed consent. - Stimulants (Cocaine and Methamphetamine)
Connect to integrated prenatal and addiction care services immediately. Address dehydration and
malnutrition. Promote sleep hygiene, gentle exercise, and mindfulness. Provide fetal growth scans and
maternal cardiovascular assessments. Encourage recovery groups for pregnant women. - Sedatives and Benzodiazepines
Provide gradual medical tapering under supervision. Offer non-pharmacologic anxiety management
such as CBT and relaxation training. Coordinate psychiatry, obstetrics, and addiction specialists.
Prepare for possible neonatal sedation or withdrawal.
Holistic and Psychosocial Support
Address underlying trauma with compassion. Provide peer recovery mentorship. Connect mothers to
housing and nutrition assistance programs. Include breastfeeding guidance, parenting education, and
relapse prevention planning.
In summary, addiction care during pregnancy is most effective when it combines medical expertise, emotional support, and respect for maternal dignity. Early intervention, medication-assisted treatment when needed, trauma-informed counseling, and coordinated prenatal services significantly reduce risks to both mother and baby. Compassionate and evidence-based care creates the strongest foundation for
healthy pregnancies, safer deliveries, and long-term recovery. Supporting expecting mothers through
addiction treatment is an investment in stronger families and healthier future generations
Family Support Strategies for Expectant Mothers with Addiction
Pregnancy can be a powerful turning point in recovery, but it can also be a time of intense vulnerability. Expectant mothers facing addiction often experience fear, guilt, stigma, and overwhelming stress while trying to protect both their own health and their baby’s development. Family support during this period is one of the strongest predictors of successful treatment engagement and long-term recovery. When families provide emotional safety, practical assistance, and informed encouragement, they help transform addiction care from an individual struggle into a shared healing journey.
This guide explores how family support strategies strengthen recovery for expecting mothers across emotional, practical, and systemic levels of care.
💞 Emotional Support and Stability
Family plays a critical role in creating emotional safety. Many expecting mothers with addiction carry shame or fear of judgment, which can prevent them from seeking help. Compassionate family support reduces these emotional barriers and promotes honesty in treatment.
How this helps:
Encourages openness about struggles without fear of criticism.
Reduces isolation, a major trigger for relapse.
Strengthens self-worth and motivation for recovery.
Example:
A partner or parent who attends prenatal visits or therapy sessions communicates acceptance and shared responsibility, reinforcing that the mother is not alone in her recovery.
🏡 Healthy Home Environment
A stable home environment is essential for both maternal and fetal well-being. Chaotic or substance-exposed environments increase stress and relapse risk.
How this helps:
Removes triggers such as alcohol, drugs, or using peers from the home.
Encourages healthy routines, such as proper sleep, nutrition, and prenatal care.
Creates predictability, which reduces anxiety and emotional instability.
Example:
Family members taking over childcare or financial responsibilities during early recovery allow the mother to focus on treatment and prenatal health.
🩺 Encouragement of Treatment and Follow-Through
Families strongly influence whether expecting mothers enter treatment and remain engaged.
How this helps:
Assists with researching programs, scheduling appointments, and providing transportation.
Participates in family therapy or parenting classes to build trust and accountability.
Reinforces medical recommendations, improving adherence to medication-assisted treatment and counseling plans.
Family involvement often bridges the gap between intention and sustained participation in treatment.
🧠 Education and Understanding Addiction as a Disease
Families who understand addiction as a chronic medical condition become more effective and compassionate supporters.
How this helps:
Reduces blame and stigma.
Improves communication about triggers, cravings, and relapse prevention.
Equips family members to recognize early warning signs and respond calmly rather than react emotionally.
Education replaces judgment with empathy — a cornerstone of recovery.
👶 Parenting Preparation and Postpartum Support
Recovery does not end at delivery. The postpartum period carries a high risk for relapse and postpartum depression.
How this helps:
Assists with newborn care, allowing the mother to rest and continue treatment.
Monitors for mood changes or relapse risk.
Supports bonding while managing stress safely.
A prepared family safety plan during postpartum weeks protects both mother and baby.
🤝 Connection to Community Resources
Families often serve as bridges to broader support systems.
How this helps:
Connects mothers to WIC, Medicaid, housing assistance, and perinatal treatment programs.
Encourages participation in peer recovery groups such as Mothers in Recovery or SMART Recovery for Women. Expands the social network, reducing isolation and improving long-term recovery stability. Community connection ensures recovery is not limited to the home alone.
In summary, when families are educated, compassionate, and actively engaged, they transform a mother’s recovery from a solitary struggle into a shared journey of healing. Family involvement increases treatment participation, stabilizes emotional health, and creates a nurturing environment where both mother and baby can thrive. Supporting expecting mothers through addiction recovery is not only an act of care for one individual — it is an investment in healthier families and stronger future generations.
Community Resource Strategies to Support
Expectant Mothers with Addiction
Expectant mothers affected by addiction benefit most when healthcare, social services, and community
networks work together. Community resource strategies improve treatment access, reduce stigma, and
strengthen maternal–infant wellness. This handout outlines key community-based supports that help
stabilize recovery during pregnancy and after delivery.
🏥 1. Integrated Prenatal and Addiction Treatment Programs
Perinatal clinics combine obstetric, addiction, and mental health care. Medication-assisted treatment, such as buprenorphine or methadone, is provided within prenatal services to improve maternal and fetal
outcomes.
🧑🤝🧑 2. Peer Recovery and Mentorship Programs
Mothers in recovery programs and peer mentors provide emotional support, guidance through services,
and encouragement throughout pregnancy and postpartum recovery.
🏡 3. Safe Housing and Shelter Support
Maternity homes, sober-living residences, and transitional housing protect mothers and infants from
unsafe or triggering environments.
🍎 4. Nutrition and Financial Assistance
WIC, SNAP, and TANF programs ensure access to food, prenatal education, and essential resources
for healthy fetal development.
🧠 5. Mental Health and Trauma Services
Community counseling, trauma-informed therapy, and behavioral health partnerships address
underlying emotional causes of addiction and reduce the risk of relapse.
🩹 6. Harm Reduction and Outreach
Mobile clinics, naloxone distribution, and outreach services improve safety, prenatal engagement, and
early treatment access.
📚 7. Legal and Advocacy Support
Legal aid services and advocacy programs protect maternal rights and promote treatment-first
approaches over punitive responses.
🌈 8. Postpartum and Parenting Support
Home-visiting programs, parenting classes, and continued treatment services support bonding, prevent
relapse, and strengthen family stability.
When community organizations, healthcare systems, and recovery networks collaborate, expecting
mothers receive the support needed to heal, deliver healthy babies, and sustain long-term recovery.
Strong community care builds stronger families and healthier futures
Frequently Asked Questions
Here are some common questions:
Is it safe to seek help for addiction while pregnant?
Yes. Seeking treatment during pregnancy is the safest and healthiest choice for both mother and baby. Healthcare providers focus on medical support and harm reduction, not punishment, and early care greatly improves outcomes.
Can stopping substances suddenly harm the baby?
In some cases, yes. Abrupt withdrawal from opioids, benzodiazepines, or alcohol can cause miscarriage, preterm labor, or fetal distress. Medical supervision is essential for safe stabilization.
What treatments are used for opioid addiction during pregnancy?
Medication-assisted treatment with buprenorphine or methadone is the standard of care. These medications stabilize the mother, reduce the risk of relapse, and improve prenatal outcomes.
Will my baby be born addicted?
Babies are not “addicted,” but some may experience neonatal abstinence syndrome (NAS), a temporary withdrawal condition that can be safely treated after birth. Medical teams monitor and manage this carefully.
Can I receive counseling during pregnancy?
Yes. Behavioral therapy, trauma-informed counseling, and peer recovery support are strongly encouraged and safe throughout pregnancy.
Is cannabis safe for pregnancy-related nausea or pain?
No amount of cannabis is considered safe during pregnancy. Cannabis exposure is linked to low birth weight and potential neurodevelopmental effects. Safer medical alternatives should be discussed with a provider.
Can I quit smoking while pregnant?
Yes. Behavioral counseling is the first-line treatment. If needed, nicotine replacement therapy may be used under medical supervision.
Will child protective services automatically be involved?
Policies vary by state, but seeking prenatal treatment voluntarily often reduces legal risk and demonstrates commitment to care. Providers aim to support families, not separate them.
Are addiction medications safe while breastfeeding?
Many are. Methadone and buprenorphine are generally compatible with breastfeeding under medical guidance. Each situation is assessed individually.
What support is available after delivery?
Postpartum care may include continued treatment, mental health services, home-visiting programs, parenting support, and relapse prevention planning.
Conclusion
Comprehensive addiction care during pregnancy protects both mother and child by addressing substance use with dignity, medical expertise, and consistent support. When interventions include medication-assisted treatment, mental health services, family involvement, and postpartum planning, recovery becomes more attainable and sustainable. While each pregnancy and recovery journey is unique, compassionate, coordinated, and evidence-based care creates the strongest foundation for healthy births, stable parenting, and long-term sobriety. Supporting expecting mothers in recovery is not only a medical responsibility—it is an investment in future generations.
Video: This Could Save Your Baby’s Life If You’re Pregnant and Addicted #pregnancy #recovery #baby