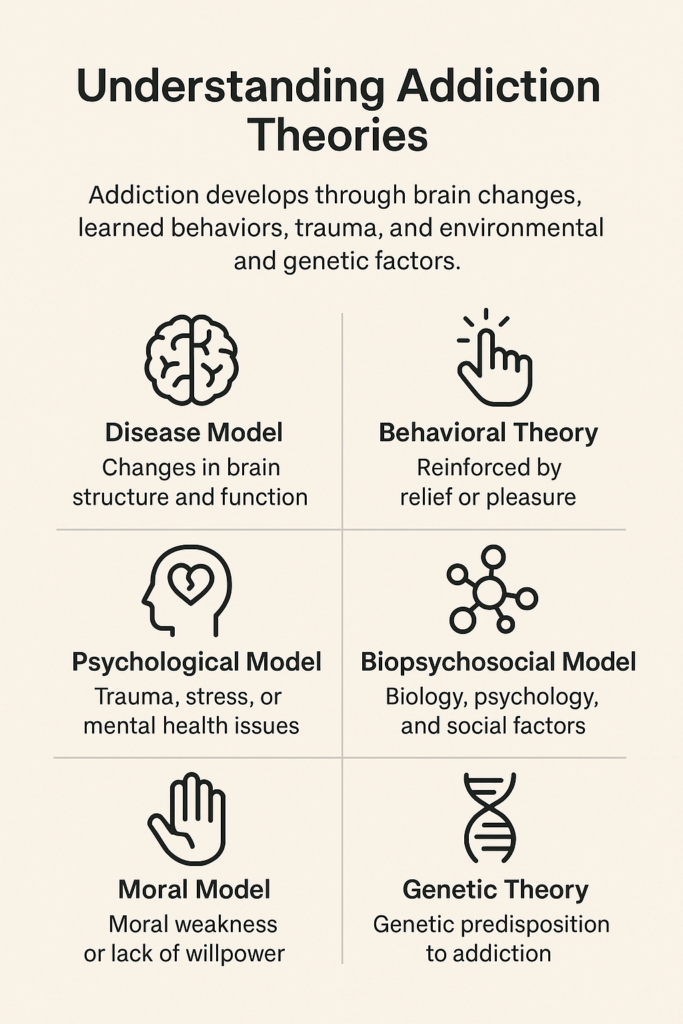
Addiction theories provide an understanding of substance use disorders and guideline treatment approaches. These theories, which include biological, psychological, and social perspectives, tailor interventions to individual needs. While they offer benefits, such as improved treatment options, barriers like stigma and accessibility can hinder their effectiveness. Ethical dilemmas may arise regarding treatment prioritization and individual autonomy. Community resource strategies are vital to overcoming these challenges and fostering collaboration among healthcare providers, support groups, and educational programs. By implementing these strategies, communities can enhance support systems and promote effective recovery for patients with addiction.
Understanding Theories of Addiction: A Simple Guide
Addiction is a complicated issue that scientists and researchers try to understand through different theories. These theories help explain why people become addicted to substances like drugs or alcohol and how they can recover. Here’s an easy-to-understand guide to some of the main ideas behind addiction:
1. Biological Theories
- Genetics: Some people may be born with genes that make them more likely to develop an addiction. This means addiction can sometimes run in families.
- Brain Changes: Drugs and alcohol change how the brain works, especially in areas that control feelings of pleasure. The more someone uses, the more their brain gets used to needing the substance to feel good, which can lead to addiction.
2. Psychological Theories
- Cognitive Behavioral Theory (CBT): This theory says addiction happens because people learn to rely on substances to cope with stress, anxiety, or other problems. Over time, these habits become hard to break.
- Psychodynamic Theory: This idea suggests that unresolved emotional issues, like past trauma or hidden feelings, may push someone to use substances as a way to deal with pain or difficult emotions.
3. Social and Environmental Theories
- Social Learning: According to this theory, people can develop addictions by watching and learning from others, especially friends or family who use substances.
- Environmental Influences: Where someone lives, who they hang out with, and what’s available around them (like easy access to drugs or alcohol) can increase the risk of addiction.
4. Developmental Theories
- Life Stages: This theory examines how different life stages, such as childhood or the teenage years, can influence addiction. People who experience trauma or problems early in life may be more likely to develop addiction later.
- Adverse Childhood Experiences (ACEs): Bad experiences in childhood, like abuse or neglect, increase the chance that someone will struggle with addiction as they get older.
5. Behavioral Theories
- Reward and Reinforcement: When people use drugs or alcohol, they often feel good, which makes them want to keep using. This theory explains addiction as a habit people develop because they are “rewarded” by the good feelings from the substance.
- Triggers: Certain things, like a place or a person, can remind someone of using drugs or alcohol, causing cravings. Over time, the brain connects these triggers with the desire to use the substance.
6. Integrated Theories
- Biopsychosocial Model: This model explains addiction as a mix of many things: genetics, mental health, and social environment. It shows that a combination of biology, emotions, and life circumstances influences addiction.
- Public Health Approach: This theory views addiction not just as an individual problem but as something affected by the community, such as the availability of treatment options and prevention programs.
7. Existential and Spiritual Theories
- Existential Theory: Some people turn to substances because they search for meaning or purpose in life and feel lost or empty.
- Spiritual Models: Some believe addiction comes from a lack of spiritual connection, and recovery involves finding a sense of purpose or belonging through spirituality.
Addiction is influenced by many factors—biological, psychological, social, and even spiritual. Each theory offers a different perspective on why addiction happens and how it can be treated. Understanding these different views helps us create better ways to support people in recovery and help them overcome addiction.
Treatment Options Based on Theories of Addiction
Understanding the different theories of addiction helps shape effective treatment options. Here’s a breakdown of treatment strategies aligned with various theories:
1. Biological Theories
Medication-Assisted Treatment (MAT): Medications like methadone, buprenorphine, and naltrexone can help manage cravings and withdrawal symptoms. This approach recognizes the biological factors influencing addiction.
Genetic Counseling: Individuals with a family history of addiction may benefit from counseling to understand their genetic predispositions, allowing for tailored prevention and treatment strategies.
2. Psychological Theories
Cognitive Behavioral Therapy (CBT): This therapy helps individuals identify and change negative thought patterns and behaviors that contribute to addiction. It equips them with practical skills to cope with cravings.
Psychodynamic Therapy: This approach focuses on exploring underlying emotional issues and traumas that may lead to substance use, fostering deeper self-understanding.
3. Social and Environmental Theories
Support Groups: Programs like Alcoholics Anonymous (AA) and SMART Recovery create communities where individuals share experiences and support each other in preventing relapse.
Family Therapy: Involving family members in treatment addresses family dynamics that may contribute to addiction, promoting a healthier home environment.
4. Developmental Theories
Early Intervention Programs: Targeting at-risk youth with support and resources can help prevent the onset of addiction, focusing on healthy development.
Trauma-Informed Care: Recognizing and addressing past traumas through specialized therapy can reduce the risk of future substance use.
5. Behavioral Theories
Contingency Management: This approach rewards positive behaviors, such as remaining sober or attending therapy sessions, reinforcing recovery efforts.
Trigger Management: Individuals learn to identify and cope with triggers using techniques like urge surfing, which helps them ride out cravings without acting on them.
6. Integrated Theories
Holistic Approaches: Combining medical, psychological, and social interventions provides comprehensive care that addresses the whole person.
Comprehensive Treatment Plans: Tailoring treatment to include various modalities—such as therapy, medication, and support groups—ensures that individual needs are met.
7. Existential and Spiritual Theories
Mindfulness and Meditation: These practices help individuals find meaning and reduce stress, fostering a sense of calm during recovery.
Spiritual Counseling: Integrating spiritual beliefs into recovery can enhance a sense of purpose and connection, supporting overall well-being.
By implementing treatment options that align with various addiction theories, professionals can offer personalized care that addresses the unique needs of individuals in recovery. This holistic approach enhances treatment effectiveness and supports long-term recovery and overall well-being.
Overcoming Barriers to Addiction Treatment: Understanding Challenges in Applying Theories of Addiction
When it comes to treating addiction, various theories offer valuable insights, but they also come with barriers that can hinder effective treatment. Understanding these challenges is crucial for creating successful recovery strategies. Here’s a breakdown of the barriers associated with different addiction theories:
1. Biological Theories
- Stigma Around Medication: Many individuals fear being labeled or judged for using medication-assisted treatment (MAT), which can deter them from pursuing this effective option.
- Access to Medications: High costs and limited availability of essential medications can prevent those in need from receiving the treatment that could help them recover.
2. Psychological Theories
- Resistance to Therapy: Fear of facing emotional pain or past trauma can lead to resistance against engaging in therapy, limiting treatment progress.
- Emotional Readiness: Not everyone is mentally prepared to tackle deep-seated issues, making it difficult to engage fully in the therapeutic process.
3. Social and Environmental Theories
- Lack of Support Systems: A supportive network is vital for recovery. Without family or friends who understand and support the process, individuals may struggle to stay on track.
- Social Stigma: Negative societal attitudes toward addiction can discourage people from seeking help, leading to feelings of isolation and shame.
4. Developmental Theories
- Under-Recognition of Risk Factors: Early intervention is key, but insufficient awareness of identifying high-risk populations may lead to missed prevention opportunities.
- Ongoing Trauma Exposure: For individuals still facing traumatic or adverse conditions, recovery efforts may be severely undermined.
5. Behavioral Theories
- Inconsistent Reinforcement: Behavioral therapies often rely on consistent rewards to motivate change. However, inconsistent application can reduce motivation and engagement.
- Difficulty Identifying Triggers: Many individuals may find it hard to pinpoint their triggers, which complicates implementing effective coping strategies.
6. Integrated Theories
- Fragmented Services: Lack of coordination among medical, psychological, and social services can lead to gaps in care, making it difficult for individuals to get comprehensive support.
- Complex Needs: Those with co-occurring issues may require more integrated care than is typically available, leading to inadequate treatment.
7. Existential and Spiritual Theories
- Personal Beliefs: Not everyone resonates with spiritual or existential concepts, which can limit the effectiveness of these approaches in specific populations.
- Cultural Differences: Cultural perceptions of spirituality may affect how these concepts are integrated into treatment, necessitating a tailored approach.
Recognizing and addressing these barriers is essential for improving addiction treatment outcomes. By understanding the challenges associated with each theory, healthcare providers can develop more effective, individualized treatment plans that foster recovery and support long-term healing.
Ethical Dilemmas in Addiction Treatment Theories
Addiction theories provide valuable frameworks for understanding substance use disorders, but they also come with ethical dilemmas that can complicate treatment. Here’s a look at some of these challenges across various theoretical perspectives:
1. Biological Theories
Determinism vs. Free Will: Viewing addiction primarily as a biological issue can lead to the perception that individuals have little control over their behavior. This raises ethical concerns about personal responsibility and accountability.
Stigmatization: Such a perspective may label individuals as “sick,” overshadowing their capacity for change and fostering stigma.
2. Psychological Theories
Informed Consent: Heavy reliance on psychological interventions can obscure the risks and benefits, complicating informed consent.
Therapeutic Boundaries: Close emotional ties in therapy can blur professional boundaries, leading to ethical concerns in therapist-client dynamics.
3. Social and Environmental Theories
Blame and Responsibility: These theories might focus on environmental factors, which could diminish individual accountability and the role of personal choice.
Resource Allocation: Addressing social factors may require substantial community resources, raising ethical questions about equitable distribution.
4. Developmental Theories
Historical Context: Emphasizing early life experiences may over-pathologize behaviors influenced by current circumstances, potentially undermining individual agency.
Potential for Labeling: Labeling children and adolescents based on their developmental history can affect their future opportunities and treatment options.
5. Behavioral Theories
Informed Consent and Autonomy: Behavior modification techniques may limit autonomy by focusing on external rewards instead of intrinsic motivation.
Cultural Sensitivity: Behavioral interventions may not account for cultural differences, raising ethical concerns about treatment efficacy and acceptance.
6. Integrated Theories
Complexity and Confusion: Integrating multiple theories can confuse patients and providers, complicating informed consent and treatment goals.
Resource Intensive: Coordinating care based on integrated theories can be resource-heavy, raising ethical questions about access and equality.
7. Existential and Spiritual Theories
Cultural and Personal Relevance: Not all individuals resonate with existential or spiritual approaches, leading to ethical dilemmas about imposing values that may not align with patients’ beliefs.
Subjectivity in Treatment: The subjective nature of existential healing makes it challenging to establish standardized ethical practices, leading to inconsistent care.
Each addiction theory presents unique ethical dilemmas that can complicate treatment. Addressing these concerns requires a thoughtful, inclusive approach that respects individual autonomy, cultural values, and the complex nature of addiction. Balancing scientific understanding with ethical considerations is essential for effective and compassionate care.
Community Resource Strategies for Implementing Addiction Theories in Treatment
Effective addiction treatment requires a multifaceted approach, leveraging community resources based on various addiction theories. Here are some strategies for implementing these theories in community settings:
1. Biological Theories
Medication-Assisted Treatment (MAT): Communities can enhance access to MAT for opioid and alcohol use disorders, ensuring individuals receive vital medications like methadone or buprenorphine alongside counseling.
Health Education Campaigns: Initiatives aimed at educating the public about the biological aspects of addiction can help reduce stigma and foster understanding.
2. Psychological Theories
Cognitive Behavioral Therapy (CBT) Programs: Establish community-based CBT workshops and support groups to assist individuals in identifying and changing negative thought patterns related to addiction.
Mental Health Services Integration: Collaborate with mental health providers to offer comprehensive care that addresses both addiction and underlying psychological issues.
3. Social and Environmental Theories
Community Outreach Programs: Develop initiatives that engage at-risk populations through education about addiction and its social influences, promoting healthier environments.
Supportive Housing Initiatives: Create sober living environments and transitional housing options to support recovery and reduce exposure to triggering social conditions.
4. Developmental Theories
Youth Prevention Programs: Implement school-based programs that educate young people about the risks of substance use and promote healthy coping strategies.
Family Support Services: Offer resources to help families understand the developmental impacts of addiction, fostering healthier dynamics and communication.
5. Behavioral Theories
Skill-Building Workshops: Organize community workshops on developing coping skills, stress management, and relapse-prevention strategies grounded in behavioral principles.
Positive Reinforcement Programs: Create community incentives for individuals who engage in healthy behaviors, such as staying sober or participating in recovery activities.
6. Integrated Theories
Holistic Treatment Centers: Establish centers that provide a range of services, including medical, psychological, and social support, to address addiction from multiple perspectives.
Collaborative Care Models: Foster partnerships among healthcare providers, social services, and community organizations to create coordinated care plans for individuals in recovery.
7. Existential and Spiritual Theories
Mindfulness and Meditation Programs: Offer community classes in mindfulness, yoga, and meditation to help individuals explore personal meaning and resilience in recovery.
Spiritual Support Groups: Create spaces for individuals seeking spiritual guidance or support through faith-based recovery programs.
8. Public Awareness Campaigns
Stigma Reduction Initiatives: Launch campaigns to raise awareness about addiction as a complex issue, emphasizing the importance of community support and available resources.
Educational Workshops: Host community forums and workshops to educate the public on addiction theories and their implications for treatment and recovery.
Community resource strategies grounded in addiction theories can significantly enhance treatment effectiveness and support recovery. By providing diverse resources and fostering collaboration among various stakeholders, communities can create supportive environments that address the complex nature of addiction.
Frequently Asked Questions
Here are some common questions:
How do brain-based theories explain cravings and relapse?
Brain-based theories show that addiction alters dopamine pathways, stress responses, and decision-making centers. Triggers can activate these pathways automatically, causing cravings even when someone is committed to recovery.
Why is trauma critical in addiction theories?
Trauma-informed theories recognize that adverse childhood experiences and chronic stress increase addiction risk. Substances may be used to numb emotional pain or regulate overwhelming feelings.
How do addiction theories influence treatment?
Understanding addiction theories helps tailor treatment approaches. For example, medications address brain chemistry, therapy addresses coping and trauma, and social supports address environmental risks.
Conclusion
Addiction theories play a crucial role in shaping our understanding and treatment of substance use disorders. By highlighting the biological, psychological, and social factors involved, these theories provide valuable insights that can enhance treatment effectiveness. However, challenges such as stigma, accessibility, and ethical dilemmas persist, complicating the recovery journey for many individuals. Community resource strategies are essential for addressing these barriers and fostering collaboration and support to facilitate recovery. By leveraging these strategies, communities can create a more inclusive and practical framework for addiction treatment, ultimately leading to better outcomes for those affected by addiction.
Video: Is Addiction a Brain Problem or a Choice? #shorts #addiction #psychology