Addiction as a disease process changes how we see, treat, and manage it. This perspective shifts the focus from blaming the individual to recognizing that addiction involves complex interactions in the brain, the environment, and personal history. This article explores the disease model of addiction, examining its scientific foundations and the treatment methods employed. Whether you’re studying this topic for personal reasons or to help someone else, this discussion offers a layman’s explanation of a subject that affects so many lives.
Understanding Addiction as a Disease
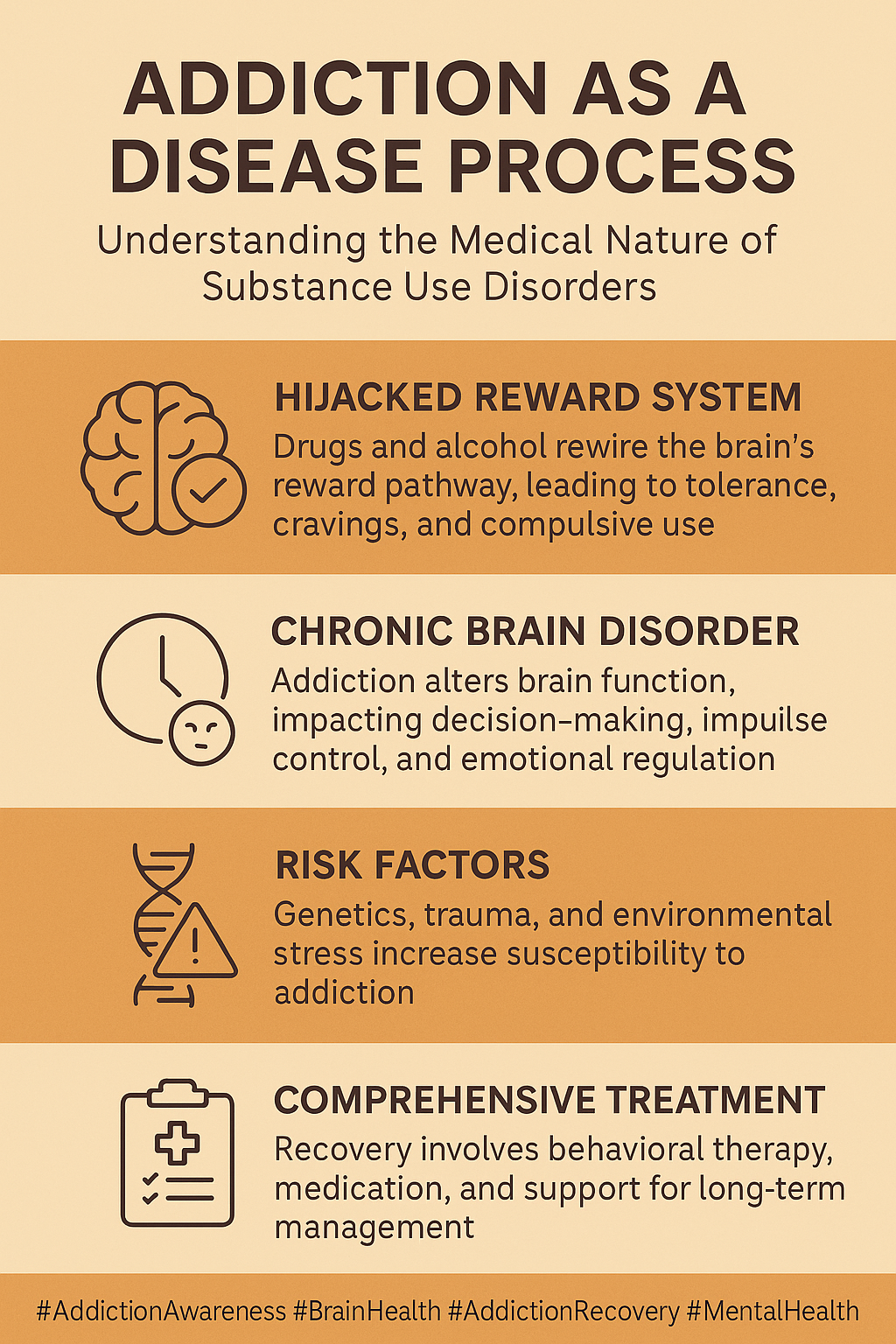
Addiction is often misunderstood as a simple matter of willpower or moral failing. However, research shows that addiction is a disease affecting how brain circuits function. Drawing on decades of research in neuroscience and psychology, experts now see addiction as a chronic condition that alters the brain’s reward, memory, and motivation systems. This understanding helps remove stigmas and directs our focus toward treatment and recovery rather than blame.
Historically, addiction was seen as a personal weakness rather than a medical condition. With advances in brain imaging and genetic studies, it has become clear that repeated use of substances or engagement in certain behaviors can lead to permanent changes in the brain. These changes affect decision-making and impulse control. Recognizing addiction as a disease enables health professionals to adopt approaches similar to those used in treating other chronic conditions, such as diabetes, where ongoing management is key.
Moreover, viewing addiction in medical terms helps society shift its perspective away from judgment and toward compassion and care. Public health policies now favor prevention and early intervention over punishment and incarceration. This shift is crucial, as it enables greater investment in education, community programs, and support services that ultimately benefit everyone affected by addiction.
Biological and Psychological Foundations
The biological basis of addiction centers on the brain’s reward system. Substances and certain compulsive behaviors can trigger the release of neurotransmitters. Dopamine is one of the most critical chemicals involved; it reinforces pleasurable activities, routinely making the brain want to repeat them. Over time, repeated exposure to addictive substances can lead to a significant change in the way neurons communicate, making it difficult for the individual to experience pleasure from everyday activities.
Psychologically, addiction often intertwines with patterns of behavior and coping strategies developed over time. Many people turn to substance use when faced with stress, trauma, or overwhelming emotions. The brain gradually learns to depend on external substances for the feeling of reward, creating a cycle that is hard to break. This connection between biology and behavior is what drives the compulsive nature of addiction. A person’s background, personal experiences, and even genetic predispositions can play a role in how addiction manifests.
Key terms in understanding the neurobiology of addiction include:
- Neuroplasticity: The ability of the brain to change and adapt, which can be both a path to recovery and a reason why relapse may occur.
- Genetic Predisposition: Some individuals inherit genes that make them more likely to develop addictive behaviors when exposed to specific triggers.
- Reward Pathways: Neural circuits activated during pleasurable activities reinforce these behaviors and may pave the way for addiction.
This blend of biological and psychological factors reinforces that addiction is not a weakness but a complex condition that benefits from all-in-one treatment strategies.
Additional research has also shown that changes in gene expression and alterations in brain structure occur over time, reinforcing the chronic nature of addiction. Scientists are continually working to break down these processes to understand better how each element interacts and to develop targeted therapies.
Psychosocial and Environmental Factors
The social and environmental context of a person’s life plays a significant role in the development and persistence of addiction. Family dynamics, peer pressure, and economic challenges can all contribute to the development of addictive behaviors. For instance, growing up in a home where substances were easily accessible or where unhealthy coping mechanisms were modeled can elevate one’s risk of falling into addictive patterns.
Stressful life events, such as the loss of a loved one or job-related pressures, also increase vulnerability. In situations where immediate surroundings lack a stable support network, individuals might turn to substances or behaviors as a way to escape pain or anxiety. This illustrates how addiction is intricately linked with both internal struggles and external pressures.
Factors that often contribute include:
- Social Isolation: A lack of community involvement or fulfilling relationships can drive someone to find solace in addictive substances.
- Economic Instability: Financial pressures may increase psychological stress, prompting individuals to seek temporary relief through substance use.
- Exposure to Addiction: Living in environments where drug use is widespread makes it more likely for individuals to adopt similar behaviors, perpetuating cycles of addiction.
Furthermore, cultural attitudes and societal norms can significantly influence how addiction is addressed. When communities collaborate to enhance living conditions and offer support, recovery becomes more attainable. There is a growing recognition that successful treatment must address not only the physical aspects of addiction but also the emotional and environmental influences at play.
Managing Addiction: Treatment and Recovery
Addiction treatment usually requires a multifaceted approach. When addiction is viewed as a disease, treatment strategies focus on both addressing the biological aspects and providing the psychological support necessary for change. Both medication and therapy work best when combined; one method on its own is rarely enough. The goal is to guide individuals toward long-term recovery through a range of techniques.
One typical regimen integrates:
- Medical Intervention: Medications can help manage withdrawal symptoms and reduce cravings. For example, drugs like methadone or buprenorphine help patients deal with opioid addiction by stabilizing brain chemistry.
- Cognitive Behavioral Therapy (CBT): Therapy helps individuals address negative thought patterns and develop healthier coping strategies. CBT is designed to provide practical tools that reduce the urge to revert to addictive behaviors during times of stress.
- Support Groups: Community support through 12-step programs or other group therapies is vital in sustaining long-term recovery. Sharing experiences with others who understand similar challenges can build resilience and reduce feelings of isolation.
- Holistic Approaches: Incorporating mindfulness exercises, regular physical activity, and creative therapies, such as art or music therapy, can enhance overall well-being. These practices help restore balance in life and address the emotional consequences of addiction.
Recovery is not a one-time event but a continuous process. Those who struggle with addiction must keep a sharp eye on their recovery, consistently engaging in follow-ups with healthcare professionals, support groups, and sometimes even relapse prevention planning. This ongoing management ensures that setbacks are addressed promptly and that the progress made is maintained over time.
Many treatment centers now emphasize relapse prevention and long-term maintenance, recognizing that addiction is a chronic condition that can reappear if the underlying issues are not continuously managed. By combining structured therapies with community support, rehabilitation programs help individuals rebuild their lives and regain control over their futures.
Frequently Asked Questions
Addressing common queries can help clarify the complexities surrounding addiction as a disease. Here are some questions that often arise:
Question: Why is addiction considered a disease?
Answer: Research has shown that addiction changes the way the brain works. These alterations affect decision-making, behavior, and impulse control, much as other chronic diseases do. Recognizing addiction as a disease shifts the focus toward treatment and support rather than blame.
Question: What role do genetics play in addiction?
Answer: Genetics can increase the likelihood of addiction by influencing how susceptibility develops. However, only one of several factors—along with environment and personal experiences—contributes to the condition.
Question: How effective are current treatments in managing addiction?
Answer: While there is no one-size-fits-all cure for addiction, many treatment options help manage its symptoms successfully. Combining medications, therapy, and community support often leads to better outcomes. It is essential to understand that recovery is a progressive process and requires ongoing effort.
Wrapping Up
Understanding addiction as a disease provides a more compassionate and effective pathway toward recovery. By acknowledging that addiction involves both brain changes and environmental factors, treatment can be more holistic and tailored to individual needs. This shift in perspective has led to more integrated treatment models and continuous support systems that address the chronic nature of addiction.
There is still much to learn about the intricacies of addiction. However, embracing its complexity is necessary to reduce stigma and offer adequate care. Viewing addiction through the lens of a disease reshapes the conversation around prevention, intervention, and rehabilitation. It encourages the development of community programs, educational campaigns, and policy reforms that support immediate recovery and long-term wellness.
Recovery is not a linear process, and every individual’s journey is unique. Continuous research, community engagement, and accessible treatment options are all components of a broader strategy to ease the impact of addiction. Each step taken toward understanding and addressing the condition brings us closer to a society where those struggling with addiction feel safe to seek help and rebuild their lives.
Additional support and proactive outreach from communities can play a pivotal role in sustaining recovery. Family members, friends, and co-workers can contribute to a supportive environment by offering empathy and practical assistance. Historically, the stigma associated with addiction prevented many from reaching out for help; today, however, increased awareness is leading to more supportive networks and innovative treatment methods. Over time, this collective effort can help transform lives and reduce the overall burden of addiction.
In conclusion, it is essential to acknowledge that addiction is a multifaceted condition. By combining medical interventions with psychological support and a strong social network, we can offer a lifeline to those struggling with this disease. The path to recovery may be rocky, but with ongoing care and community support, lasting change is within reach.
Video: The Surprising Science Behind Addiction