Quitting the toughest drugs, such as opioids, methamphetamine, and cocaine, is a challenge due to the profound induction of neurological changes. These substances alter the brain’s structure and function, making cessation complex. This introduction explores the daunting task of quitting these substances, delving into the neurological alterations contributing to addiction. It highlights the importance of comprehensive strategies, including self-management, family support, and community resources, to facilitate the journey toward sobriety while mitigating withdrawal symptoms. Understanding this complex interplay is crucial for those seeking to break free from the clutches of addiction.
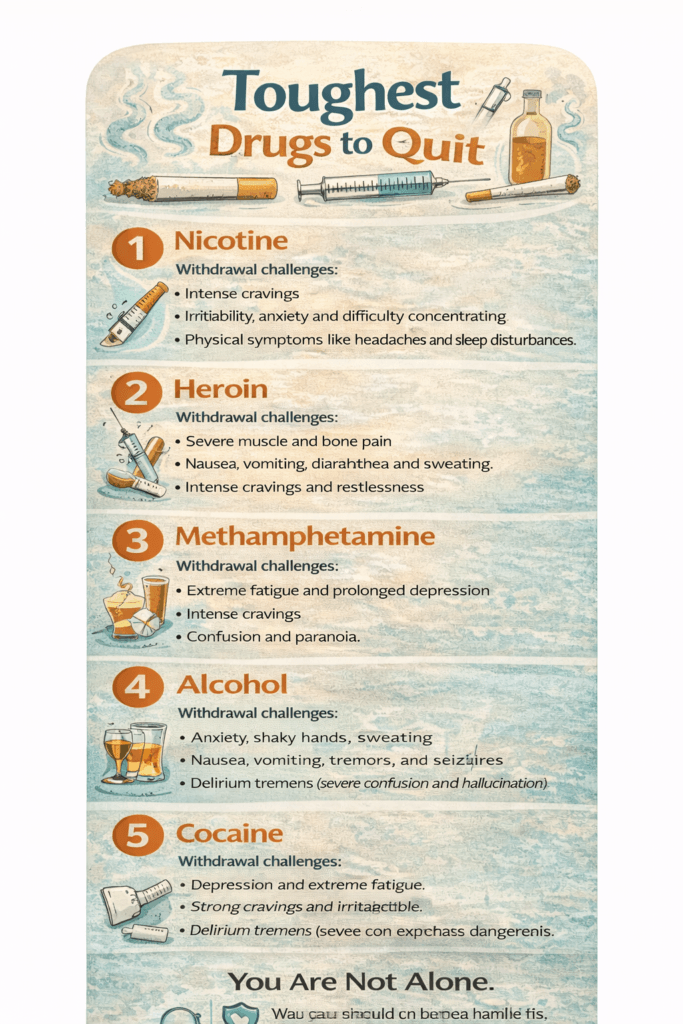
Understanding Withdrawal Challenges: A Look at Difficult Drugs to Quit
The process of quitting drugs can be incredibly challenging, with withdrawal symptoms varying wildly depending on the substance, the level of dependency, and individual factors. Here’s a closer look at some drugs known for their complicated withdrawal processes and the risks involved:
1. Opioids (Heroin, Oxycodone, Fentanyl)
- Withdrawal Symptoms: Intense symptoms include nausea, vomiting, muscle aches, anxiety, diarrhea, and insomnia.
- Risks: While opioid withdrawal is rarely life-threatening, the discomfort can be so severe that it often leads to relapse without professional support. Medical-assisted treatments like methadone or buprenorphine can help ease the process.
2. Benzodiazepine (Xanax, Valium, Ativan)
- Withdrawal Symptoms: Symptoms can include severe anxiety, insomnia, tremors, seizures, and, in extreme cases, delirium.
- Risks: Abruptly stopping benzodiazepines is dangerous. Withdrawal requires gradual tapering under medical supervision to prevent seizures and life-threatening complications.
3. Alcohol
- Withdrawal Symptoms: Mild symptoms include tremors, sweating, and anxiety, while severe cases may involve hallucinations, confusion, and seizures.
- Risks: Delirium tremens (DT), a severe form of alcohol withdrawal, can be life-threatening and requires immediate medical intervention. Medications like benzodiazepines are often used to manage symptoms safely.
4. Nicotine
- Withdrawal Symptoms: Symptoms include irritability, intense cravings, difficulty concentrating, changes in mood, and sleep disturbances.
- Risks: While not life-threatening, nicotine withdrawal is psychologically challenging due to the highly addictive nature of the substance. Nicotine replacement therapies (patches, gum) can support cessation efforts.
5. Stimulants (Cocaine, Methamphetamine)
- Withdrawal Symptoms: Symptoms can include fatigue, depression, increased appetite, vivid dreams, and sleep disturbances.
- Risks: Withdrawal from stimulants is generally not life-threatening, but the risk of depression and suicidal ideation is a significant concern. Professional mental health support is essential during recovery.
6. Cannabis
- Withdrawal Symptoms: Irritability, insomnia, reduced appetite, restlessness, and mood changes are common during cannabis withdrawal.
- Risks: Although withdrawal is less severe compared to other substances, it can still disrupt daily functioning, especially for heavy users. Behavioral therapies are often effective in overcoming cannabis dependency.
Why Professional Help is Essential
Quitting any substance can be a daunting process. Factors like the duration of use, the substance involved, and individual health conditions make withdrawal experiences unique. Professional help ensures:
- Safe Monitoring: Medical professionals can manage potentially life-threatening symptoms, especially for alcohol and benzodiazepine withdrawal.
- Tailored Treatment: Treatment plans can include medications, counseling, and support groups to address both physical and psychological challenges.
- Relapse Prevention: With the guidance of healthcare providers, individuals are more likely to achieve sustained recovery.
The journey to recovery is different for everyone, but understanding the challenges and risks of withdrawal is the first step toward successful treatment. If you or someone you know is struggling with addiction, seek professional assistance to ensure a safe and supportive transition to a healthier life. Recovery is not only possible but attainable with the right help.
Neurological Changes in Drug Addiction: Understanding the Brain’s Role in the Struggle to Quit”
Drug addiction is a complex disorder that goes beyond mere willpower. It involves significant neurological changes that affect the brain’s reward system, decision-making processes, and ability to regulate behavior. These changes help explain why addiction is so difficult to overcome and why relapse is common. Here are some of the key neurological changes associated with drug addiction:
1. Dopamine Release and the Reward System
- How It Works: Drugs of abuse, including stimulants, opioids, and alcohol, often trigger a massive release of dopamine in the brain’s reward system.
- The Effect: Dopamine is a neurotransmitter that plays a central role in pleasure and reward. Over time, the brain becomes accustomed to the heightened levels of dopamine, making it harder to experience pleasure from natural rewards like food, social interactions, or hobbies without using the drug.
- Why It’s Difficult to Quit: This diminished responsiveness to natural rewards leads to a cycle where the individual feels the need to keep using the drug to feel “normal” or experience pleasure.
2. Neuroplasticity and Brain Structure Changes
- How It Works: Chronic drug use induces neuroplastic changes—alterations in the brain’s structure and function. Neurons and synapses, the brain’s communication channels, are restructured in ways that reinforce drug-seeking behavior.
- The Effect: These changes create strong connections between drug use and environmental cues, such as places, people, or situations associated with substance use. This makes cravings and relapse more likely when these cues are encountered.
- Why It’s Difficult to Quit: These learned associations are difficult to break and can persist long after the individual has stopped using the drug.
3. Hijacking the Brain’s Learning and Memory Circuits
- How It Works: Drugs can hijack the brain’s circuits that are responsible for learning and memory. This leads to the formation of strong memories that associate drug use with pleasurable experiences.
- The Effect: These memories, deeply ingrained in the brain, contribute to intense cravings when the individual is exposed to drug-related stimuli.
- Why It’s Difficult to Quit: The brain’s strong connection between the pleasurable effects of drug use and specific memories or situations makes it difficult to resist the urge to relapse.
4. Changes in the Prefrontal Cortex
- How It Works: The prefrontal cortex, responsible for decision-making, impulse control, and considering long-term consequences, is significantly impacted by addiction.
- The Effect: With long-term drug use, the prefrontal cortex becomes less efficient in helping individuals make rational decisions or control impulses. This results in impaired judgment, difficulty resisting cravings, and the inability to make decisions that align with their long-term well-being.
- Why It’s Difficult to Quit: This dysfunction in the brain’s decision-making areas leads to the inability to stop drug use, even in the face of negative consequences.
5. Stress and the Amygdala
- How It Works: The amygdala, the brain region that processes emotions and stress, becomes altered during chronic drug use.
- The Effect: These changes can make the individual more sensitive to stress, which may trigger cravings and heighten the emotional responses that contribute to relapse.
- Why It’s Difficult to Quit: Stressful situations or emotional triggers can lead to overwhelming cravings, pushing individuals back into the cycle of addiction as a means of coping with discomfort.
6. Tolerance and Withdrawal
- How It Works: As drug use continues, the body develops tolerance, meaning the individual needs larger amounts of the substance to achieve the same effects.
- The Effect: Withdrawal symptoms—both physical and psychological—can become intense, including anxiety, sweating, nausea, and depression. These symptoms serve as a powerful motivator to continue using the drug to avoid discomfort.
- Why It’s Difficult to Quit: The physical discomfort of withdrawal can be so severe that individuals feel compelled to relapse to alleviate symptoms, making quitting feel nearly impossible.
7. Incentive Sensitization
- How It Works: According to the incentive sensitization theory, repeated drug use can “sensitize” the brain’s reward system to cues associated with drug use.
- The Effect: Over time, drug-related cues (like seeing a needle, entering a familiar bar, or hearing music associated with use) can trigger intense cravings.
- Why It’s Difficult to Quit: Even after a period of abstinence, the brain remains highly sensitive to these cues, increasing the risk of relapse.
8. Loss of Control
- How It Works: Addiction is often defined by a loss of control over drug use, despite knowing the negative consequences. Neurological changes in the brain’s reward system, stress responses, and impulse control mechanisms all contribute to this lack of control.
- The Effect: The brain becomes conditioned to prioritize the pursuit of drugs over other life goals or values, leading to compulsive behavior.
- Why It’s Difficult to Quit: The loss of control makes it harder to stop using drugs, even when an individual truly desires to quit.
Understanding the neurological changes that occur in the brain during addiction underscores the complexity of overcoming substance dependence. Addiction is not simply about lack of willpower; it is a chronic, relapsing disorder that alters the brain’s chemistry, structure, and function. Addiction treatment, therefore, needs to address these neurological changes through a combination of medical, psychological, and social interventions. With the proper support, individuals can begin to repair these brain functions and regain control over their lives.
Self-Management Strategies for Quitting Drugs and Easing Withdrawal Symptoms
Quitting drugs can be one of the most challenging experiences in a person’s life, often accompanied by withdrawal symptoms that range from physical discomfort to intense emotional strain. While professional guidance is essential for successful drug cessation, several self-management strategies can help individuals cope with withdrawal and support their recovery. Here are some effective self-management strategies to complement a comprehensive approach to quitting drugs:
1. Gradual Reduction
- What It Is: Gradually tapering off drug use, rather than quitting abruptly, can ease withdrawal symptoms.
- How It Helps: This approach allows the body to adjust more slowly to reduced drug levels, minimizing the shock to the system. It’s essential to do this under the supervision of a healthcare professional to ensure safety and effectiveness.
2. Hydration and Nutrition
- What It Is: Staying well-hydrated and eating a balanced diet during withdrawal is crucial for physical recovery.
- How It Helps: Proper nutrition supports the body’s healing process by replenishing vital nutrients depleted by drug use. Hydration can help alleviate headaches and fatigue, which are often associated with withdrawal.
3. Regular Exercise
- What It Is: Engaging in physical activity, such as walking, yoga, or more intense exercise, can provide relief during withdrawal.
- How It Helps: Exercise releases endorphins, the body’s natural mood enhancers, which can help combat feelings of depression, anxiety, and irritability during the withdrawal process.
4. Adequate Sleep
- What It Is: Prioritizing good sleep hygiene and maintaining a regular sleep schedule can support the body’s recovery.
- How It Helps: Sleep is essential for both physical and mental healing. Creating a comfortable sleep environment and avoiding stimulants before bed can help improve sleep quality during withdrawal.
5. Mindfulness and Relaxation Techniques
- What It Is: Practices like mindfulness meditation, deep breathing, and progressive muscle relaxation can help manage stress.
- How It Helps: These techniques can reduce anxiety and help individuals stay grounded during the emotional turbulence of withdrawal. They also promote emotional regulation and relaxation, providing a healthier coping mechanism.
6. Establishing a Routine
- What It Is: Creating a structured daily routine can help maintain a sense of purpose and stability during recovery.
- How It Helps: A consistent routine reduces uncertainty and helps keep the individual focused on daily goals, decreasing the likelihood of relapse due to boredom or stress.
7. Social Support
- What It Is: Building a network of friends, family, or peers who understand the challenges of quitting can be invaluable.
- How It Helps: Having a strong support system provides encouragement, accountability, and reassurance. Social connections help mitigate the isolation that many individuals feel during withdrawal, which can contribute to relapse.
8. Counseling and Therapy
- What It Is: Professional counseling or therapy, such as cognitive-behavioral therapy (CBT) or motivational enhancement therapy (MET), addresses the psychological aspects of addiction.
- How It Helps: Therapy helps individuals identify triggers, develop coping strategies, and address underlying emotional issues that contribute to substance use. It’s a vital part of long-term recovery.
9. Distraction Techniques
- What It Is: Engaging in activities that keep the mind occupied and divert attention away from cravings.
- How It Helps: Hobbies like reading, painting, or cooking provide an outlet for energy and focus, helping to combat the urge to use drugs as a way of coping with cravings.
10. Hygiene and Self-Care
- What It Is: Taking care of personal hygiene and practicing self-care can improve mental well-being.
- How It Helps: Feeling clean and well-groomed can boost self-esteem and provide a sense of normalcy during a difficult time. Personal care rituals also act as a positive distraction from withdrawal symptoms.
11. Setting Realistic Goals
- What It Is: Establishing small, achievable goals throughout the recovery process.
- How It Helps: Celebrating each small victory—whether it’s a week without drugs or managing a craving—can provide motivation and a sense of accomplishment, helping to maintain momentum in the recovery journey.
12. Educational Resources
- What It Is: Learning about the effects of addiction and the recovery process.
- How It Helps: Understanding addiction, withdrawal, and recovery can empower individuals to make informed decisions and better prepare for the challenges ahead. Education also reduces feelings of shame or guilt that often accompany addiction.
13. Journaling
- What It Is: Writing down thoughts, feelings, and progress in a journal.
- How It Helps: Journaling provides a safe space for self-reflection, helping individuals track their emotional journey, gain insights into their triggers, and stay motivated throughout recovery.
14. Hot and Cold Therapy
- What It Is: Alternating between hot and cold showers or compresses.
- How It Helps: These therapies can help alleviate physical discomfort, such as muscle aches or headaches, that are common during withdrawal. The temperature contrast can also help promote relaxation and stress relief.
15. Over-the-Counter Remedies
- What It Is: Some individuals find relief from specific symptoms with over-the-counter remedies, such as medications for nausea or pain.
- How It Helps: While non-prescription treatments can ease symptoms, it’s crucial to consult with a healthcare professional before using any medication to ensure they are safe and appropriate for the withdrawal process.
While self-management strategies can be beneficial, it’s important to remember that quitting drugs, especially in the face of withdrawal, requires professional guidance and support. These strategies should be used in conjunction with medical supervision and a comprehensive recovery plan tailored to the individual’s needs. By combining self-management with expert support, individuals can increase their chances of successfully overcoming addiction and achieving long-term recovery.
Family Support Strategies for Helping Loved Ones Quit Drugs and Cope with Withdrawal”
Recovering from drug addiction is a challenging journey, and the support of family members can be a crucial factor in helping someone overcome addiction and navigate the difficulties of withdrawal. Family involvement can provide emotional support, promote positive behavior changes, and help manage the recovery process effectively. Here are some family support strategies that can contribute to creating a supportive environment for recovery:
1. Education and Understanding
- What It Is: Family members should take the time to educate themselves about the specific drug, its withdrawal symptoms, and the recovery process.
- How It Helps: Understanding the complexities of addiction and withdrawal fosters empathy and allows family members to provide informed, compassionate support throughout the recovery process.
2. Open Communication
- What It Is: Establish open and honest communication within the family.
- How It Helps: Encouraging the individual to express their feelings, concerns, and experiences without judgment can foster a safe, supportive environment. Transparent communication strengthens trust and deepens familial bonds during recovery.
3. Participate in Treatment
- What It Is: Family members should consider attending family therapy sessions or support groups as part of the individual’s treatment plan.
- How It Helps: Being involved in the therapeutic process helps family members understand their roles in the recovery journey and equips them with tools to support the individual’s treatment and growth effectively.
4. Create a Sober Living Environment
- What It Is: Make the home a drug-free space by removing triggers and temptations.
- How It Helps: A sober living environment provides a stable and supportive backdrop for recovery, reducing the risk of relapse and encouraging the individual to focus on healing and maintaining sobriety.
5. Encourage Treatment Engagement
- What It Is: Encourage the individual to engage in professional treatment services, such as counseling, therapy, or a rehabilitation program.
- How It Helps: Supporting the individual’s commitment to recovery and helping them stay engaged in professional treatment provides them with the necessary tools and resources for lasting change.
6. Establish Boundaries
- What It Is: Set clear and healthy boundaries within the family.
- How It Helps: Boundaries promote accountability and ensure that the needs of both the recovering individual and the family are respected. Setting boundaries helps create a healthy and functional family dynamic during the recovery process.
7. Provide Emotional Support
- What It Is: Offer consistent emotional support through love, understanding, and encouragement.
- How It Helps: Acknowledge the individual’s efforts and progress, and celebrate milestones in their recovery. Positive reinforcement can help build their self-esteem and keep them motivated.
8. Participate in Supportive Activities
- What It Is: Engage in healthy, shared activities like exercising together, preparing nutritious meals, or going on family outings.
- How It Helps: Positive experiences strengthen family bonds and offer alternatives to drug use, creating a supportive, nurturing environment for recovery.
9. Avoid Enabling Behaviors
- What It Is: Be mindful of behaviors that might unintentionally enable drug use, such as minimizing the consequences or covering up for the individual.
- How It Helps: Enabling behaviors can hinder recovery and prolong the cycle of addiction. Setting clear, healthy limits and holding the individual accountable can encourage them to take responsibility for their recovery.
10. Plan for Crises
- What It Is: Develop a crisis plan for possible relapses or challenging situations.
- How It Helps: Knowing how to respond calmly and effectively to setbacks reduces the risk of panic or emotional reactions. A well-thought-out plan ensures that the family is prepared to support the individual during challenging moments.
11. Attend Support Groups
- What It Is: Family members should consider joining support groups for families of individuals struggling with addiction.
- How It Helps: Connecting with others facing similar challenges provides a sense of community and valuable insights into how others cope with the complexities of addiction recovery.
12. Encourage Healthy Coping Mechanisms
- What It Is: Help the individual develop healthy coping mechanisms for stress and emotional challenges.
- How It Helps: Encouraging new, healthier ways to manage emotions—such as through hobbies, exercise, or social support—can reduce the reliance on drugs as a coping mechanism.
13. Celebrate Achievements
- What It Is: Celebrate even the small victories in recovery.
- How It Helps: Recognizing progress helps boost motivation and self-esteem. It also reinforces the individual’s commitment to recovery by focusing on positive achievements rather than setbacks.
14. Be Patient
- What It Is: Understand that recovery is a long-term process.
- How It Helps: Patience is essential in managing expectations and handling setbacks. Recovery takes time, and family members must recognize that setbacks are part of the journey. Offering unwavering support, even during difficult times, is key.
15. Seek Professional Guidance
- What It Is: If necessary, consider seeking guidance from a family therapist or addiction counselor.
- How It Helps: Professional support provides additional tools and strategies to navigate family dynamics during recovery, ensuring everyone involved is equipped to handle the challenges of addiction recovery.
Family support is a cornerstone of successful addiction recovery. By fostering a compassionate, understanding, and proactive environment, families can play an instrumental role in helping their loved ones navigate the complexities of quitting drugs and managing withdrawal symptoms. With education, patience, and the right resources, families can create a solid foundation for lasting recovery and healing.
Community Support Strategies for Individuals in Recovery: Building a Network for Success
Community support is a powerful tool for individuals seeking to quit drugs and manage withdrawal symptoms. A strong community can provide emotional encouragement, practical resources, and a sense of belonging—vital components for successful recovery. Here are several community strategies that can contribute to a supportive environment for individuals in recovery:
1. Support Groups
- What It Is: Support groups, whether local or online, provide a space where individuals in recovery can share their experiences, challenges, and successes.
- How It Helps: These groups foster a sense of community and understanding, helping individuals realize they are not alone in their recovery journey. The shared experiences in support groups often lead to valuable insights and coping strategies.
2. Community-Based Treatment Programs
- What It Is: Local treatment programs offer a combination of counseling, therapy, and support services tailored to the needs of individuals in recovery.
- How It Helps: Community-based treatment programs provide accessible care, addressing not only addiction but also co-occurring mental health issues, social support, and other challenges. These programs are often designed to be affordable and inclusive, making treatment available to a broad range of people.
3. Recovery Community Organizations
- What It Is: Recovery community organizations (RCOs) focus on building connections through events, workshops, and social activities.
- How It Helps: These organizations promote a sense of belonging, empowerment, and shared purpose. By connecting with others who are also in recovery, individuals can gain motivation, guidance, and a network of peers who understand their journey.
4. Peer Mentoring Programs
- What It Is: Peer mentoring programs pair individuals in recovery with mentors who have successfully navigated addiction.
- How It Helps: Having a mentor who understands the struggles of addiction provides valuable support. Peer mentors offer guidance, encouragement, and practical advice, showing individuals that recovery is possible and giving hope for a brighter future.
5. Community Events and Workshops
- What It Is: Attend events and workshops focusing on addiction recovery, mental health, and overall well-being.
- How It Helps: These events offer education, networking opportunities, and the chance to build a broader support network. Workshops can equip individuals with new skills, coping strategies, and valuable information that fosters both personal and professional growth.
6. Employment and Vocational Training Programs
- What It Is: Explore community-based programs that help individuals in recovery find meaningful employment through job training and skill-building.
- How It Helps: Employment is an essential aspect of recovery, providing individuals with purpose, stability, and financial independence. Vocational training programs can increase an individual’s employability and contribute to long-term success in recovery.
7. Sober Living Homes
- What It Is: Sober living homes provide a structured and supportive environment for individuals transitioning from rehabilitation to independent living.
- How It Helps: These homes provide a safe, drug-free living environment that allows individuals to continue focusing on their recovery while reintegrating into society. They provide a supportive peer network and house rules that help prevent relapse.
8. Health Clinics and Counseling Services
- What It Is: Access to local health clinics and counseling services that offer mental health support, therapy, and addiction treatment resources.
- How It Helps: These services provide vital mental health support during recovery, addressing co-occurring conditions like depression, anxiety, or trauma that may affect an individual’s recovery process.
9. Community-Based Outreach Programs
- What It Is: These programs provide education, resources, and support to individuals struggling with addiction. They may also offer harm reduction initiatives and awareness campaigns.
- How It Helps: Outreach programs raise awareness and connect individuals with vital services, providing a bridge to treatment and other community resources that support recovery.
10. Faith-Based Organizations
- What It Is: Many faith-based organizations offer support, counseling, and community programs for those in recovery.
- How It Helps: For some individuals, faith and spirituality can provide the strength and support needed to overcome addiction. These organizations often offer counseling services, group meetings, and a supportive community.
11. Community Fitness and Wellness Programs
- What It Is: Participate in local fitness and wellness programs that promote mental and physical health.
- How It Helps: Regular physical activity has been shown to improve mood, reduce stress, and help manage withdrawal symptoms. Community wellness programs provide a healthy outlet for managing emotions and building physical strength, which can complement addiction recovery efforts.
12. Public Awareness Campaigns
- What It Is: Participate in or support public campaigns that aim to reduce the stigma around addiction and promote understanding.
- How It Helps: Reducing stigma encourages more people to seek help and fosters a supportive environment for those in recovery. Public awareness initiatives can foster an atmosphere in which individuals feel safer and more empowered to seek treatment.
13. Community-Based Therapeutic Services
- What It Is: Services like acupuncture, massage therapy, or holistic therapies that complement traditional addiction treatments.
- How It Helps: These therapies help manage stress, ease withdrawal symptoms, and promote overall well-being. Many individuals in recovery find holistic approaches to be beneficial for their physical and emotional healing.
14. Educational Initiatives
- What It Is: Work with educational institutions to implement programs that educate students, parents, and teachers about the risks of drug use.
- How It Helps: Education and prevention programs play an essential role in reducing drug use and helping young people make informed decisions. These initiatives contribute to a drug-free community and offer support for those in recovery.
15. Legal and Advocacy Resources
- What It Is: Connect with community organizations that provide legal guidance and advocacy services related to addiction, such as employment discrimination.
- How It Helps: Legal and advocacy resources can help individuals in recovery navigate legal challenges and advocate for their rights, ensuring that they are treated fairly as they rebuild their lives.
Building a network of support is crucial for individuals in recovery. Community strategies that offer emotional encouragement, access to resources, and opportunities for personal growth can provide the foundation needed to maintain sobriety. A diverse and inclusive community is key to supporting individuals as they transition from addiction to a healthier, drug-free life. By participating in these community initiatives, individuals in recovery can benefit from a comprehensive support system that empowers them to achieve long-term success.
Frequently Asked Questions
Here are some common questions:
What makes a drug difficult to quit?
Drugs are harder to quit when they cause intense withdrawal, strong cravings, rapid brain reward changes, and emotional dependence. The more a substance alters survival and stress circuits in the brain, the harder stopping becomes.
Which drugs are considered the hardest to quit?
Opioids (fentanyl, heroin, prescription painkillers), alcohol, benzodiazepines, nicotine, and methamphetamine are consistently ranked among the most difficult due to withdrawal severity and relapse risk.
Why are opioids so hard to quit?
Opioids deeply affect pain, pleasure, and survival pathways. Withdrawal causes severe physical symptoms and emotional distress. Cravings remain strong long after detox.
Why is alcohol withdrawal dangerous?
Alcohol withdrawal can cause seizures, heart instability, and delirium. Medical supervision is often required to quit safely.
Why are benzodiazepines difficult to stop?
These medications change brain calming systems. Stopping suddenly can cause panic, insomnia, tremors, or seizures. Slow medical tapering is necessary.
Why is nicotine on the list if it’s legal?
Nicotine rapidly reinforces dependence and creates strong habitual behavior. Withdrawal causes irritability, anxiety, and concentration problems, making relapse common.
Why is methamphetamine so hard to quit?
Meth causes extreme dopamine release. After quitting, the brain struggles to produce normal pleasure, leading to depression, fatigue, and intense cravings.
Is fentanyl harder to quit than heroin?
Yes. Fentanyl is more potent and fast-acting, causing stronger dependence and more severe withdrawal.
Why do people relapse even after detox?
Detox clears the drug from the body, but brain changes and emotional triggers remain. Recovery requires long-term treatment, not just detox.
Is willpower enough to quit these drugs?
No. Addiction is a brain disease. Willpower alone cannot override withdrawal biology and craving circuits. Medical and behavioral treatment is needed.
Are medications available to help quitting?
Yes. Medications like buprenorphine, methadone, naltrexone, acamprosate, and nicotine replacement reduce withdrawal and relapse risk.
Does trauma or mental illness make quitting harder?
Yes. Untreated anxiety, depression, PTSD, or chronic pain increase relapse risk. Integrated treatment improves outcomes.
Can people fully recover from severe addiction?
Yes. Long-term recovery is common with proper treatment, support, and lifestyle change.
What is the most important factor in successful quitting?
Consistent treatment engagement, social support, coping skills, and relapse-prevention planning.
Where can someone get help?
Medical providers, addiction treatment centers, therapy, peer recovery groups, and crisis services provide support.
Conclusion
Overcoming the formidable challenge of quitting the toughest drugs necessitates a multifaceted approach. The profound neurological changes induced by substances like opioids, methamphetamine, and cocaine underscore the complexity of addiction. However, by integrating self-management strategies, seeking unwavering family support, and tapping into community resources, individuals can enhance their chances of a successful recovery with minimized withdrawal symptoms. Recognizing the intricate interplay between neurological factors and the support mechanisms available is essential. As we collectively strive to address the unique hurdles posed by each drug, fostering a comprehensive understanding and implementing tailored strategies is crucial in paving the way for individuals to reclaim their lives from the grips of addiction.
Video: