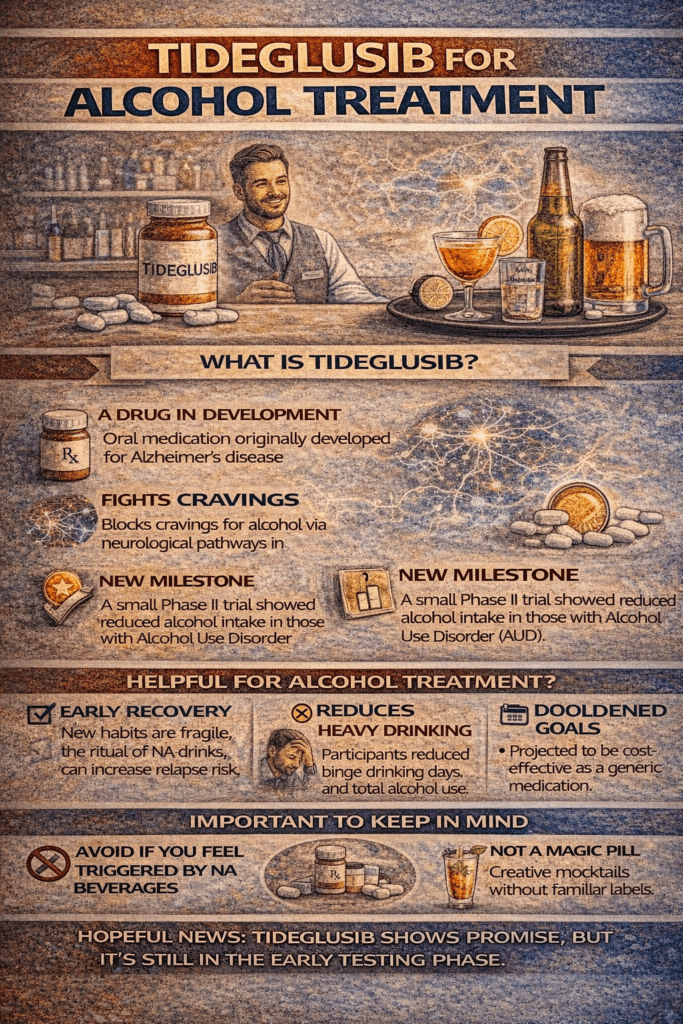
Tideglusib, a GSK-3β inhibitor initially developed for neurodegenerative diseases, is now being explored as a treatment for alcohol use disorder (AUD). Early research suggests it may reduce chronic alcohol intake by targeting brain pathways linked to addiction. Potential advantages include reduced relapse risk and non-daily dosing. However, disadvantages include limited human trial data and possible side effects. Ethical concerns involve off-label use and informed consent. Tideglusib is not yet FDA-approved for AUD and remains in the research phase.
Tideglusib: A Promising New Candidate in the Treatment of Alcohol Use Disorder
Tideglusib, a selective inhibitor of glycogen synthase kinase three beta (GSK3β), is emerging as a potential breakthrough in the treatment of alcohol use disorder (AUD). Preclinical research led by scientists at Virginia Commonwealth University (VCU) demonstrated that tideglusib significantly reduced both chronic alcohol consumption and binge drinking behaviors in animal models. Notably, these effects occurred without altering normal water intake or inducing anxiety-like side effects.
Source: VCU Scholars Compass, PubMed
The drug’s mechanism of action involves modulation of the Wnt/β-catenin signaling pathway, which plays a vital role in brain functions related to learning, memory, and reward. Tideglusib inhibits GSK3β, a key regulator in this pathway, thereby potentially restoring healthy neuronal signaling in areas of the brain impacted by alcohol use. This normalization may help reduce the reinforcing effects of alcohol and support long-term behavioral change.
Reference: PubMed
While these findings are encouraging, tideglusib is still in the early stages of investigation for AUD. More comprehensive clinical trials are needed to determine its safety, optimal dosage, and efficacy in human populations. Nonetheless, it represents a promising step forward in the search for new, effective treatments for alcohol addiction.
Tideglusib and Alcohol Use Disorder: Promising Potential, But With Important Caveats
Tideglusib, a selective inhibitor of glycogen synthase kinase three beta (GSK3β), has drawn attention for its potential to reduce chronic alcohol consumption and binge drinking behaviors. While early preclinical studies have shown encouraging results, several critical concerns must be addressed before this compound can be considered a viable treatment for alcohol use disorder (AUD).
Liver Health Risks
Clinical trials involving tideglusib have reported transient elevations in liver enzymes—specifically alanine aminotransferase (ALT) and aspartate aminotransferase (AST)—in some participants. These biomarkers suggest potential liver toxicity. This risk may be particularly concerning for individuals with pre-existing liver disease, a population already vulnerable in the context of AUD.
[Source: ResearchGate]
Side Effects and Monitoring Needs
Commonly reported side effects of tideglusib include nausea, fatigue, and headaches. While more serious complications like liver toxicity or cardiac arrhythmias are rare, their possibility warrants careful monitoring. Patients undergoing treatment with tideglusib would likely require routine liver function tests and cardiac assessments.
[Source: WikiMD]
Limited Human Clinical Evidence
Most of the evidence supporting tideglusib’s efficacy in treating alcohol use disorder stems from animal models. Human data remain sparse, and large-scale, peer-reviewed clinical trials are lacking. This gap makes it difficult to fully assess how well the drug works—or how safe it is—when used in real-world, diverse human populations.
Potential for Anhedonia
Interestingly, tideglusib not only reduced ethanol consumption in animal studies but also reduced sucrose intake. This suggests a potential dampening of reward sensitivity, raising concerns about anhedonia—a condition in which individuals lose the ability to feel pleasure from ordinarily enjoyable activities. If confirmed in humans, this side effect could negatively affect the overall quality of life.
[Source: PMC]
In summary, Tideglusib represents a novel and biologically informed approach to tackling alcohol use disorder. However, its promise comes with significant questions about safety, long-term effects, and impact on quality of life. Before this drug can be integrated into treatment protocols, rigorous human clinical trials are essential to determine whether its benefits truly outweigh the risks.
Tideglusib for Alcohol Use Disorder: Promising Treatment or Ethical Minefield?
Tideglusib, a selective GSK3β inhibitor, has shown early promise in reducing alcohol consumption in preclinical studies. However, its experimental status in treating alcohol use disorder (AUD) introduces a range of ethical dilemmas that must be carefully considered before clinical application.
1. Safety vs. Experimental Use
Tideglusib is not currently FDA-approved for treating AUD. Using it outside of regulated trials raises ethical concerns about exposing patients to unknown risks.
Dilemma: Should clinicians consider an experimental treatment when human data are limited, even if preclinical results suggest benefits?
2. Informed Consent in Uncertain Terrain
Patients must be clearly informed that tideglusib is still experimental for AUD, with potential side effects such as liver toxicity and anhedonia, and uncertain long-term outcomes.
Challenge: Can clinicians ensure truly informed consent when even the scientific community lacks a complete understanding of the drug’s effects?
3. Access and Equity Concerns
If tideglusib eventually proves effective but is costly or not widely accessible, it may exacerbate existing health disparities—particularly in marginalized communities already burdened by addiction.
Ethical Issue: How can we ensure equitable access to promising but potentially expensive therapies?
4. Autonomy and Altered Brain Function
Because tideglusib may interfere with reward pathways in the brain, patients could experience a reduction in pleasure from everyday activities—a state known as anhedonia.
Concern: Could this diminish a person’s autonomy, motivation, or overall quality of life, even as it reduces alcohol cravings?
5. Off-Label Use and Clinical Integrity
Prescribing tideglusib off-label—outside of clinical trials—without robust evidence could conflict with ethical standards and regulatory frameworks.
Question: How do providers balance the urgency of innovation with the responsibility to uphold evidence-based medical practice?
6. Risk of Over-Medicalizing Addiction
Focusing solely on pharmacological solutions like tideglusib may overlook the complex psychological, social, and environmental factors driving addiction.
Ethical Consideration: Are we risking an overly medical model that neglects holistic, person-centered care?
In summary, Tideglusib’s potential in treating alcohol use disorder opens exciting doors but also poses serious ethical challenges—especially related to patient safety, informed consent, access, and quality of life. Navigating these issues responsibly requires a commitment to transparent communication, robust clinical trials, and integrative care models that respect both scientific evidence and the lived experiences of people with addiction.
FDA Approval for Tideglusib in Alcohol Use Disorder: Where It Stands and How It Could Be Accelerated
Tideglusib, an experimental drug with promising preclinical results for reducing alcohol consumption, is not yet FDA-approved for alcohol use disorder (AUD). In fact, there is currently no established timeline for such approval, as the drug is still in the early stages of research for this indication.
Understanding the FDA Approval Process
For any new drug or new use of an existing drug, the FDA approval process follows several key phases:
- Preclinical Research: Laboratory and animal studies to evaluate safety and potential effectiveness (several years).
- Phase 1 Clinical Trials: Safety testing in a small group of healthy volunteers (months to 1 year).
- Phase 2 Clinical Trials: Testing for efficacy and dose response in people with the condition (1–2 years).
- Phase 3 Clinical Trials: Large-scale trials to confirm effectiveness and monitor side effects (2–4 years).
- FDA Review: Submission of a New Drug Application (NDA), with review times ranging from 6 months (priority) to 1 year (standard).
Total estimated time: 5 to 10 years, from early testing to potential approval.
Current Status of Tideglusib for AUD
As of now:
- ✅ Tideglusib has not entered Phase 3 trials for alcohol use disorder.
- 🚫 No public timeline exists for its approval in this context.
- 🔬 Approval is likely several years away, even if early human trials prove successful.
That said, several FDA programs exist that can accelerate approval for treatments addressing severe conditions like AUD.
Pathways to Accelerate Approval
1. Fast Track Designation
- Reserved for drugs that address severe conditions with unmet needs.
- Allows frequent communication with the FDA and rolling data submission.
2. Breakthrough Therapy Designation
- Requires early clinical evidence showing substantial improvement over current treatments.
- Provides intensive FDA guidance and faster development timelines.
3. Accelerated Approval
- Based on surrogate endpoints (e.g., changes in biomarkers) that are reasonably predictive of benefit.
- Requires post-marketing confirmation of clinical outcomes.
4. Priority Review
- Speeds FDA review from 10 months to 6 months.
- Granted, if the treatment offers significant improvements in safety or efficacy.
5. Orphan Drug Designation
- Designed for rare diseases, it does not apply to AUD due to its high prevalence.
Additional Strategies to Expedite Approval
- Strong Early Data: Phase 1/2 trials must clearly demonstrate safety and effectiveness.
- Adaptive Trial Designs: Allow researchers to adjust the study protocol as results emerge.
- Collaborative Research: Partnerships between researchers, industry, and regulators can streamline progress.
- Patient Advocacy: Demonstrating strong patient demand can influence regulatory prioritization.
In summary, tideglusib’s future as a treatment for alcohol use disorder depends on its performance in early human trials. If it demonstrates strong safety and effectiveness, it may qualify for FDA programs like Fast Track or Breakthrough Therapy Designation, which could accelerate approval. Still, close collaboration with the FDA and well-executed clinical trials are essential to move this experimental drug from the lab to the clinic.
Why Tideglusib Could Be Denied FDA Approval for Alcohol Use Disorder
Tideglusib, a drug under investigation for reducing alcohol consumption, has shown early promise in preclinical models. However, like any experimental treatment, its path to FDA approval for alcohol use disorder (AUD) is not guaranteed. Several factors could lead the FDA to deny approval, even if early data are encouraging.
1. Insufficient Efficacy
The most common reason for drug rejection is a lack of clear clinical benefit. If tideglusib fails to show statistically and clinically significant reductions in alcohol use—or does not outperform placebo or standard treatments—approval is unlikely. The FDA requires robust evidence of efficacy through well-designed clinical trials.
2. Safety Concerns
Tideglusib has been associated with side effects such as liver enzyme elevations, fatigue, and headaches. If larger human trials reveal serious adverse events (e.g., liver toxicity, cardiac arrhythmias), the risk profile may be deemed unacceptable, especially for a condition like AUD that often requires long-term treatment.
3. Poor Trial Design or Weak Data
The FDA places heavy emphasis on high-quality clinical evidence. Trials with small sample sizes, poor control groups, design flaws, or inconsistent results can undermine the credibility of findings. Without well-structured, reproducible evidence, approval may be denied.
4. Unfavorable Benefit-Risk Balance
Even if tideglusib shows some effectiveness, it must offer clear benefits that outweigh its risks—especially compared to existing approved treatments like naltrexone, acamprosate, or behavioral therapies. If tideglusib’s advantages are marginal or its risks are substantial, the FDA may rule against its use.
5. Manufacturing or Quality Control Issues
FDA approval also depends on the ability to produce the drug safely, consistently, and at scale. Problems with manufacturing, drug formulation, or long-term stability can delay or prevent approval.
6. Failure to Meet Regulatory Requirements
Approval requires a complete, transparent submission. Missing or inadequate data on:
- Pharmacokinetics
- Drug interactions
- Long-term safety
- Dosing protocols
…can lead to rejection. Regulatory noncompliance—whether due to incomplete data or protocol violations—can be a dealbreaker.
In summary, while tideglusib holds potential as a novel treatment for alcohol use disorder, the FDA will only approve it if the drug meets rigorous standards for safety, efficacy, quality, and regulatory compliance. Without convincing evidence across these domains, approval may be denied. Continued research, strong trial design, and careful risk assessment will be critical to determining its future.
Frequently Asked Questions
Here are some common questions:
Question: Summarize common reasons for denial with examples from other addiction medications.
Answer: a summary of common reasons the FDA denies approval for addiction medications, with examples from past cases:
Common Reasons for FDA Denial of Addiction Medications
- Lack of Demonstrated Efficacy
- If clinical trials fail to show statistically significant and clinically meaningful benefits.
- Example: The drug ALKS 5461 (a kappa-opioid receptor antagonist for depression and possibly addiction) was rejected in 2017 due to insufficient evidence of efficacy.
- Safety Concerns
- Severe or frequent adverse effects that outweigh benefits.
- Example: TA-NIC, a nicotine vaccine, failed FDA approval partly because of safety concerns and inconsistent immune response.
- Poor Trial Design or Insufficient Data
- Trials with small sample sizes, short duration, or methodological flaws.
- Example: Several experimental medications for cocaine use disorder were denied because trials lacked power or had inconsistent endpoints.
- Unfavorable Benefit-Risk Balance
- When risks like liver toxicity, cardiac issues, or psychiatric side effects outweigh the treatment benefits, the treatment is considered ineffective.
- Example: Lorcaserin, initially approved for weight loss, was withdrawn due to cancer risk concerns, showing how safety shifts benefit-risk balance.
- Manufacturing or Quality Problems
- Inability to produce the drug consistently and safely.
- Example: Drugs may be delayed or denied if manufacturing facilities fail inspections or if drug purity is inadequate.
- Regulatory or Submission Deficiencies
- Incomplete or poor documentation.
- Example: FDA rejects applications if critical information on dosing, interactions, or long-term effects is missing.
In summary, approval depends on clear evidence of effectiveness, acceptable safety, good trial design, and manufacturing quality. Many promising addiction treatments have failed due to one or more of these factors.
Question: How have these pathways been used for other addiction treatments?
Answer: FDA accelerated pathways have been used for addiction treatments in the past:
1. Fast Track Designation
- Example: Buprenorphine received Fast Track status during its development for opioid use disorder because it addressed a serious condition with unmet need.
- This allowed for more frequent communication with the FDA and rolling submission of data, speeding up the process.
2. Breakthrough Therapy Designation
- Example: Vivitrol (naltrexone extended-release) for alcohol and opioid dependence benefited from expedited guidance due to early promising efficacy.
- Breakthrough Therapy status provides intensive FDA guidance and priority review.
3. Accelerated Approval
- While not common for addiction medications, this pathway has been used in related areas:
- Example: Some smoking cessation drugs were evaluated using surrogate endpoints (e.g., biomarker reductions) to expedite approval.
- This pathway requires post-approval studies to confirm benefit.
4. Priority Review
- Many addiction treatment drugs receive Priority Review once the NDA is submitted because they address severe conditions.
- Example: Suboxone (buprenorphine/naloxone) underwent priority review to expedite the FDA decision.
In summary, these pathways have helped bring addiction medications to market faster by:
- Allowing early and frequent FDA engagement,
- Using surrogate or intermediate endpoints,
- Prioritizing reviews for severe conditions.
For tideglusib, showing clear benefits in early trials could make it eligible for similar accelerated programs.
Question: How have FDA-accelerated pathways been used for addiction treatments in the past?
Answer: detailed examples of clinical trial designs that helped addiction treatments secure FDA accelerated pathways like Fast Track, Breakthrough Therapy, and Accelerated Approval:
1. Buprenorphine (for Opioid Use Disorder) — Fast Track & Priority Review
- Trial Design Highlights:
- Randomized Controlled Trials (RCTs) comparing buprenorphine to placebo or methadone.
- Large sample sizes (hundreds of participants) are needed to demonstrate a statistically significant reduction in opioid use.
- Multiple endpoints: opioid abstinence verified by urine drug screens, retention in treatment, and safety.
- Adaptive dose titration to optimize efficacy and minimize side effects.
- Longer duration (12 weeks or more) to show sustained benefit.
- Why it helped:
Clear, robust evidence on both efficacy and safety showed substantial improvement over existing options, supporting Fast Track and Priority Review.
2. Vivitrol (Extended-release Naltrexone) — Breakthrough Therapy
- Trial Design Highlights:
- RCTs with placebo-controlled, double-blind design.
- Primary outcome: time to relapse or percentage of abstinent days.
- Use of patient-reported outcomes and biological verification (urine toxicology).
- Inclusion of high-risk populations (e.g., recently detoxified patients).
- Additional safety monitoring for liver function and injection site reactions.
- Why it helped:
Demonstrated rapid and clinically meaningful improvement in relapse prevention with an easy-to-administer formulation, justifying expedited FDA guidance.
3. Smoking Cessation Drugs (e.g., Varenicline) — Accelerated Approval
- Trial Design Highlights:
- Use of surrogate endpoints, such as 4-week continuous abstinence rates during treatment.
- Early-phase studies to identify optimal dosing.
- Inclusion of diverse smoker populations, including those with psychiatric comorbidities.
- Safety studies focusing on neuropsychiatric adverse events.
- Why it helped:
Surrogate markers predictive of long-term cessation allowed earlier FDA approval, with commitment to post-marketing confirmatory studies.
4. Extended-release Injectable Naltrexone for Alcohol Use Disorder
- Trial Design Highlights:
- Multicenter, placebo-controlled, double-blind RCTs.
- Primary endpoints: reduction in heavy-drinking days and total abstinence days.
- Use of validated scales for craving and quality of life.
- Rigorous safety assessments for liver enzymes and injection site reactions.
- Why it helped:
Strong statistical and clinical evidence from well-designed trials led to FDA approval and Priority Review designation.
Key Trial Design Features That Support Accelerated Pathways:
| Feature | Purpose |
|---|---|
| Randomized Controlled Design | Reduce bias, provide strong evidence |
| Clinically Meaningful Endpoints | Show real patient benefits (abstinence, relapse prevention) |
| Biomarker or Surrogate Endpoints | Allow earlier assessment of effect |
| Adaptive Dosing | Optimize safety and efficacy |
| Inclusion of High-Risk Groups | Demonstrate benefit in real-world populations |
| Safety Monitoring | Detect and manage adverse effects early |
| Patient-Reported Outcomes | Capture quality of life, cravings, and adherence |
| Multicenter Trials | Increase generalizability and data robustness |
If Tideglusib’s developers design trials incorporating these elements, exceptionally robust endpoints, and safety data, it could improve the chances of gaining FDA accelerated designations.
Conclusion
Tideglusib shows promise as a novel treatment for alcohol use disorder by targeting key brain pathways involved in addiction. Its potential benefits—such as reducing alcohol intake and relapse risk—must be weighed against limited human data, possible safety concerns, and ethical issues like equitable access and informed consent. While its mechanism offers a fresh approach to AUD treatment, tideglusib is not yet FDA-approved and remains in the investigational stage. Ongoing research and carefully designed clinical trials will be essential to determine its safety, effectiveness, and place in future addiction care.
Video: How Tideglusib Breaks the Addiction Cycle #shorts #brainhealth