The “Fenty Fold” refers to deep nasal folds or tissue indentations that can develop in chronic fentanyl users. Fentanyl, a synthetic opioid 50–100 times more potent than morphine, carries a high risk of rapid dependency and severe systemic effects. Intranasal use or injection can cause vascular compromise, tissue damage, and loss of skin elasticity, especially in the face. These folds are worsened by lifestyle factors linked to long-term opioid use, such as poor nutrition, dehydration, and neglect of self-care. Management includes stopping fentanyl use, lifestyle interventions to support recovery, cosmetic treatments like dermal fillers or microneedling, and, in severe cases, surgical reconstruction.
The “Fenty Fold”: Understanding the Dangerous Posture Linked to Fentanyl Use
The “Fenty Fold” (also called the “fentanyl fold” or “fenty lean”) is a troubling physical posture often observed in people under the influence of fentanyl or similar substances like xylazine. Individuals appear bent forward at the waist, with heads lowered, knees slightly bent, and bodies stiff, resembling a frozen collapse. This posture can last for long periods, creating serious risks such as restricted breathing and poor circulation.
This phenomenon stems from fentanyl’s powerful effects on the central nervous system. As a synthetic opioid, fentanyl rapidly crosses the blood–brain barrier, leading to sedation and muscle rigidity. When the trunk muscles become rigid, the bent-over “fold” posture emerges. At the same time, fentanyl’s depressant effects slow breathing, heightening the risk of dangerous respiratory complications.
The Fenty Fold is becoming more visible in areas hardest hit by the opioid crisis, such as San Francisco. It serves as a stark visual marker of the drug’s devastating impact. Recognizing this posture is vital, as it can signal overdose or severe complications. If you see someone exhibiting the Fenty Fold, seek medical help immediately. Emergency responders can administer naloxone (Narcan), a life-saving medication that reverses opioid overdoses.
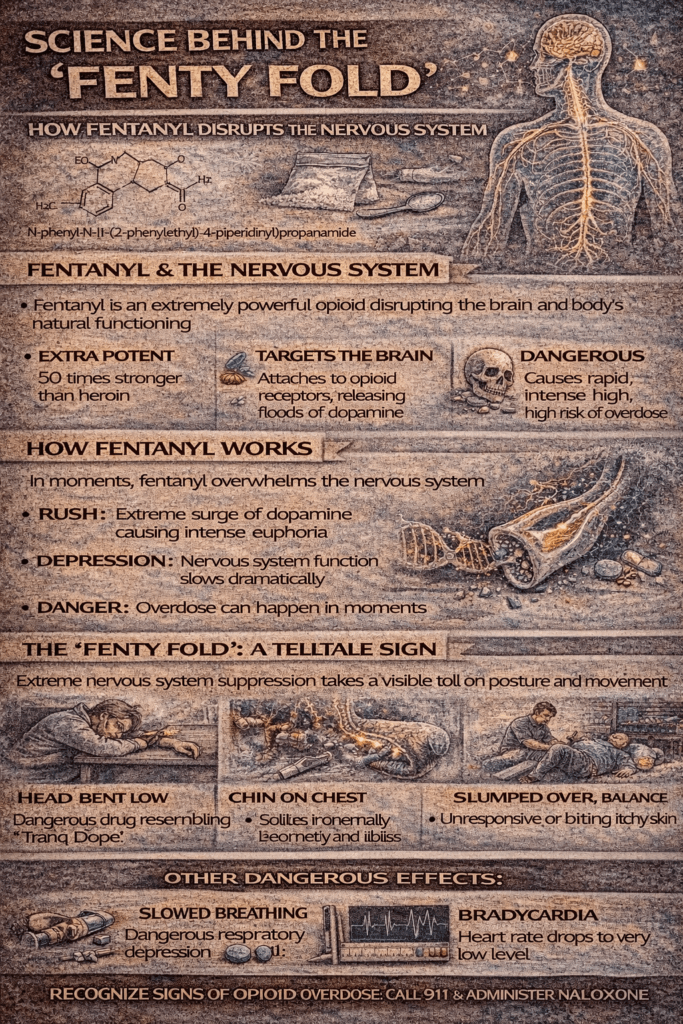
The Science Behind the “Fenty Fold”: How Fentanyl Disrupts the Nervous System
The “Fenty Fold” is a distinctive and dangerous posture seen in individuals using fentanyl, marked by a bent-over, rigid stance. This phenomenon stems from fentanyl’s profound effects on the central nervous system (CNS) and muscles, which can quickly become life-threatening.
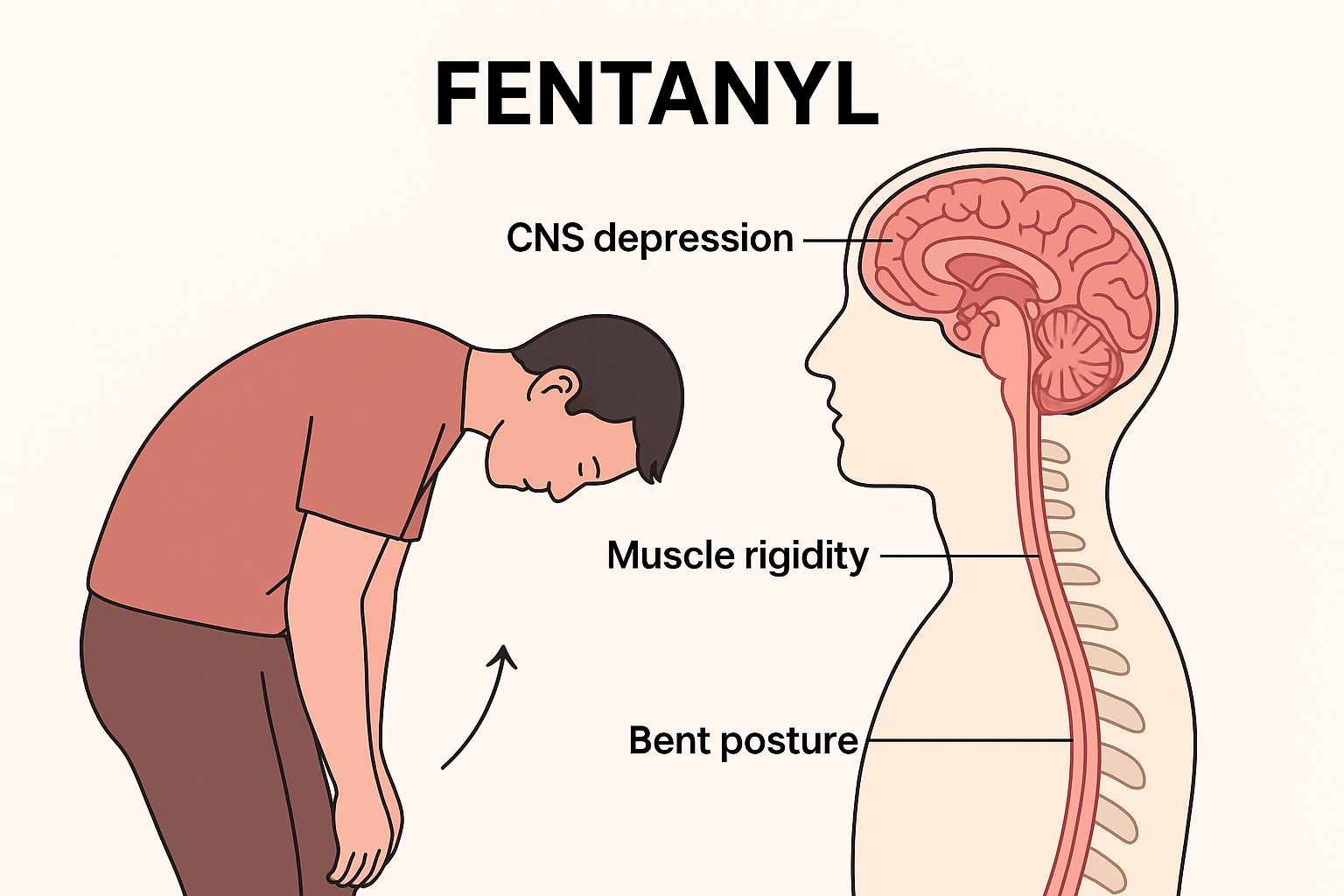
CNS Depression
Fentanyl binds strongly to mu-opioid receptors in the brain and spinal cord, depressing the brain’s respiratory centers. This slows breathing, sometimes to the point of complete respiratory arrest. Along with slowed respiration, CNS depression also causes sedation, altered consciousness, and impaired motor control.
Muscle Rigidity
A hallmark effect of fentanyl is opioid-induced muscle rigidity, often referred to as “wooden chest.” This rigidity affects the trunk, chest wall, abdomen, and back muscles, forcing the body into a bent-over or “folded” posture. Severe rigidity can further impair breathing, compounding the risk of respiratory failure.
Brainstem and Spinal Cord Involvement
By acting on the brainstem, fentanyl disrupts critical functions such as breathing, heart rate, and blood pressure. Its effects on the spinal cord contribute to impaired posture and movement control, explaining the Fenty Fold’s frozen, collapsed appearance.
Risk of Hypoxia
When CNS depression and rigidity prevent effective breathing, oxygen supply to the brain falls dangerously low. Without rapid intervention, this can lead to hypoxic brain injury or even death.
Summary
The Fenty Fold is not just a physical posture—it is a warning sign of fentanyl’s devastating impact on the nervous system. Sedation, rigidity, and respiratory depression combine to create a life-threatening state that demands urgent medical attention.
The “Fenty Fold”: Can Skin Damage from Chronic Fentanyl Use Be Reversed?
The “Fenty Fold” is an informal term used to describe deep nasal folds or tissue indentations seen in some chronic fentanyl users. While it is not a recognized medical diagnosis, it reflects fundamental changes in skin and soft tissue health linked to prolonged opioid use. These visible changes highlight how addiction affects not only internal health but also outward appearance — often serving as a physical reminder of the toll fentanyl can take on the body.
Why Does the Fenty Fold Develop?
Several factors contribute to the formation of the Fenty Fold:
- Vascular compromise: Fentanyl and other opioids can damage blood vessels and reduce circulation, depriving skin of vital oxygen and nutrients.
- Repeated trauma: Intranasal use can irritate nasal passages, while intravenous injection can cause localized tissue damage and scarring that indirectly affects facial structure.
- Poor nutrition and hydration: Chronic opioid use is often linked with malnutrition, dehydration, and lack of self-care, which weaken skin elasticity.
- Loss of collagen and elasticity: Over time, the skin loses structural proteins, leading to sagging and deepened folds.
Together, these factors create visible indentations that may become permanent without intervention.
Can the Fenty Fold Be Reversed?
The answer depends on the severity of the tissue damage. Minor skin changes may improve once a person stops fentanyl use and restores overall health, but deeper folds and structural changes are less likely to heal on their own entirely. Still, a combination of recovery and medical care can lead to meaningful improvements.
Steps Toward Recovery
- Cessation of fentanyl use
- The first and most crucial step is stopping fentanyl. Continued use only worsens tissue breakdown. Recovery allows the body’s natural healing processes to begin.
- Medical and cosmetic interventions
- Dermal fillers can temporarily reduce deep folds.
- Fat grafting uses the person’s own tissue for longer-lasting results.
- Skin resurfacing treatments (such as microneedling or laser therapy) improve skin texture and stimulate collagen production.
- Surgical correction may be recommended for severe or irreversible changes.
- Supportive lifestyle care
- Proper nutrition, including protein, vitamins, and minerals, supports tissue repair.
- Hydration restores skin elasticity.
- Sleep and self-care promote overall healing and visible improvements in skin health.
The Bigger Picture: Healing Beyond Appearance
The Fenty Fold is more than a cosmetic issue — it is a sign of the body under stress from substance use. Addressing it requires not just aesthetic repair but also treatment for the underlying addiction. Counseling, medication-assisted treatment (MAT), and community support are critical in sustaining recovery and preventing further health complications.
In summary, while the Fenty Fold is not a formal diagnosis, it reflects real and sometimes lasting changes from chronic fentanyl use. Complete reversal is unlikely if the damage is severe, but with fentanyl cessation, lifestyle improvements, and targeted medical interventions, significant improvement is possible. Healing the body inside and out is part of the larger journey toward recovery and reclaiming health.
Why Fentanyl Causes the “Fenty Fold” More Severely Than Other Opioids
The so-called “Fenty Fold” refers to deep nasal folds or indentations that appear in some chronic fentanyl users. While not a formal medical diagnosis, this visible change reflects the profound impact fentanyl has on skin, connective tissue, and overall health. What makes fentanyl different from other opioids like codeine, hydrocodone, or even heroin is its unique combination of potency, routes of administration, and systemic effects.
Potency and Chronic Use
Fentanyl is 50–100 times stronger than morphine. Even minor, repeated doses can cause prolonged episodes of poor circulation and reduced oxygen delivery to tissues. Over time, this vascular compromise damages skin elasticity and weakens the subcutaneous tissue that supports facial structure, contributing to deep folds and indentations.
Route of Administration
Many fentanyl users snort or inject the drug. Intranasal use can damage nasal cartilage and soft tissue, accelerating skin collapse in the nose and midface region. Injection use may not directly damage facial tissue, but it leads to systemic effects such as infections, circulatory problems, and malnutrition, all of which undermine skin and tissue health.
Rapid Addiction and Lifestyle Effects
Because fentanyl acts so quickly in the brain, dependence and addiction often develop faster than with less potent opioids. This rapid spiral contributes to the neglect of nutrition, hydration, and self-care — factors critical for skin health. Compared to users of weaker opioids, fentanyl users are more likely to experience accelerated tissue breakdown linked to poor lifestyle conditions.
Skin and Connective Tissue Changes
Long-term fentanyl use breaks down collagen and elastin, the proteins responsible for skin firmness and elasticity. With thinner skin and less subcutaneous fat, the nasal region is particularly vulnerable, making folds more pronounced. These changes tend to occur more quickly and severely in fentanyl users than in those using milder opioids.
In summary, the Fenty Fold develops not just because of drug use, but because of how fentanyl uniquely affects the body. Its extreme potency, common routes of use, and rapid lifestyle deterioration combine to accelerate skin and tissue damage beyond what is typically seen with other opioids. Recognizing these signs can help highlight the urgency of addressing fentanyl use disorder, both for visible recovery and for overall health.
Realistic Interventions to Improve or Reverse the “Fenty Fold”
The “Fenty Fold” — deep nasal folds or indentations associated with chronic fentanyl use — reflects lasting changes to skin and underlying tissue. While complete reversal is not always possible, meaningful improvement can be achieved through a combination of recovery, medical care, and cosmetic interventions. Here are the most realistic approaches:
1. Cessation and Overall Recovery
- Stop fentanyl use: Prevents further tissue and vascular damage.
- Nutrition and hydration: Protein, vitamins C and E, zinc, and adequate water intake help rebuild collagen and restore elasticity.
- General health: Treating infections, maintaining circulation, and stabilizing weight support skin repair.
- Timeline: Some improvement may be visible within weeks to months, though deeper folds often persist without additional treatment.
2. Non-Surgical Cosmetic Options
- Dermal fillers: Hyaluronic acid or other fillers can smooth out indentations. Results last 6–18 months.
- Fat grafting: Uses the person’s own fat for longer-lasting volume restoration, though it requires a surgical procedure.
- Skin resurfacing or microneedling: Stimulates collagen growth, improving texture and firmness. Most effective for mild or surface-level changes.
3. Surgical Interventions
- Rhinoplasty or reconstructive surgery: In cases of severe tissue or cartilage collapse, surgery may be necessary to rebuild the nasal structure.
- Combination approaches: Surgery combined with fillers or fat grafting can yield the most natural and lasting improvements.
4. Realistic Expectations
- Mild folds: Often respond well to non-surgical treatments.
- Severe, long-term folds: Typically require surgical correction; non-surgical methods may only partially improve appearance.
- Maintenance: Cosmetic improvements, especially non-surgical ones, usually require repeat treatments over time.
In summary, while spontaneous reversal of the Fenty Fold is unlikely, especially in severe cases, significant improvement is possible. The most effective path combines fentanyl cessation, improved health and nutrition, and targeted cosmetic or surgical interventions. With realistic expectations and professional guidance, individuals can restore both health and appearance as part of long-term recovery.
Frequently Asked Questions
Here are some common questions:
Question: Provide a simple diagram showing how fentanyl affects the brain, muscles, and posture to cause the Fentanyl Fold.
Answer: Fentanyl Fold diagram
Question: Provide a step-by-step roadmap for repairing “Fenty Fold” damage after chronic fentanyl use, combining lifestyle, medical, and cosmetic strategies:
Answer: Practical step-by-step roadmap for repairing “Fenty Fold” damage after chronic fentanyl use, combining lifestyle, medical, and cosmetic strategies:
Step 1: Immediate Cessation and Medical Stabilization (Weeks 0–4)
- Stop fentanyl use completely; seek medical supervision if needed to manage withdrawal.
- Medical evaluation: Check for infections, malnutrition, and any tissue damage.
- Hydration and basic nutrition: Begin a diet rich in protein, vitamins C & E, zinc, and healthy fats to support collagen synthesis.
- Gentle skin care: Moisturizers and sun protection to prevent further skin degradation.
Step 2: Lifestyle and Skin Recovery (Weeks 4–12)
- Nutrition optimization: Focus on protein (lean meats, legumes), antioxidants, and omega-3 fatty acids.
- Hydration: Drink 2–3 liters of water per day, depending on body weight and activity.
- Exercise: Improves circulation, oxygenation, and overall skin health.
- Topical treatments: Retinoids or peptides may improve skin thickness and elasticity over months.
Step 3: Non-Surgical Cosmetic Interventions (Months 3–6)
- Dermal fillers: Temporarily fill indentations and smooth folds. Repeat every 6–18 months as needed.
- Microneedling or laser resurfacing: Stimulates collagen production; best for mild to moderate folds.
- Fat grafting (optional): For deeper folds, more lasting than fillers; requires a minor surgical procedure.
Step 4: Surgical Reconstruction (Months 6–12+)
- Consult a reconstructive or cosmetic surgeon if folds are severe or cartilage collapse is present.
- Options: Rhinoplasty, tissue grafts, or a combination with fillers/fat grafting for the best results.
- Recovery: Surgical recovery can take several weeks, with final results visible after months.
Step 5: Maintenance and Long-Term Care
- Avoid relapse: Continued opioid use will reverse progress.
- Regular skin care: Moisturizers, sun protection, and collagen-stimulating treatments as needed.
- Periodic cosmetic touch-ups: Fillers or minor procedures every 6–18 months, depending on the method used.
- Lifestyle reinforcement: Ongoing nutrition, exercise, and hydration maintain tissue health.
Key Takeaways:
Recovery is gradual; patience and a combination approach yield the best results.
Early intervention, along with lifestyle changes, can prevent worsening and improve mild folds.
Moderate folds respond well to fillers, microneedling, or fat grafting.
Severe or long-term damage usually requires surgical reconstruction.
Question: Can Medicare or Medicaid pay for the surgical reconstruction of Fentys fold damage?
Answer: Medicare generally does not cover purely cosmetic surgery, i.e., done for appearance without medical or functional necessity. Medicare+1
However, Medicare may cover reconstructive surgery if it is considered medically necessary because of injury, illness, congenital defect, or other damage that impairs function. Some guidance:
- If the reconstruction is needed to restore normal function or fix a deformity caused by damage, it has a better chance of being covered. Healthline+2Insurance News Desk+2
- Medicare will cover procedures like breast reconstruction after mastectomy as an example of when reconstructive/plastic surgery is covered. Medicare.org+1
So, if the damage from FGM/C or something similar causes functional problems (urine flow, pain, risk of infection, sexual function, childbirth complications, etc.), then it may qualify as medically necessary, and thus potentially eligible for coverage under Medicare.
Medicaid
Medicaid is state-run (with federal guidelines), so whether reconstruction is covered depends heavily on which state you are in, what the state’s Medicaid program allows, and whether the procedure is documented as medically necessary.
Key points:
- Some states’ Medicaid explicitly covers female genital surgical services or reconstruction under their genitourinary services, especially when impairment of function is involved. Florida AHCA+1
- There is evidence that Medicaid sometimes covers deinfibulation (the procedure to open closed or fused labia from infibulation or other types of FGM) when that is needed for medical reasons. However, clitoral restoration is much less likely to be covered. Dame Magazine
- For example, in California (MediCal), some FGM‐related procedures do have coverage (“medically necessary procedures relating to FGM/C that fall under certain CPT codes”) for deinfibulation, but not clitoral restoration. Dame Magazine
What Would You Need to Demonstrate to Get Coverage
If you are considering trying to have Medicare or Medicaid pay for reconstructive surgery for damage (e.g., FGM/C or similar), here are what you’d likely need:
- Medical documentation that the damage is causing or has caused functional impairment, such as difficulty urinating, infections, sexual dysfunction, childbirth complications, pain, etc.
- Diagnostic evaluations and possibly recommendations from specialists (OB/GYN, urology, plastic/reconstructive surgery) that demonstrate that the reconstructive surgery is likely to restore some necessary function or relieve medical problems, not purely aesthetic.
- Use of correct procedure codes (CPT or similar), which match the covered services in the state Medicaid or Medicare policy. If there are specific codes for FGM‐related surgeries (like deinfibulation), those help.
- Pre‐authorization or prior approval, especially for reconstructive genital surgery. Payors often need to review and approve the necessity in advance.
- Knowing your state’s Medicaid policy is essential because it may explicitly include or exclude specific genital reconstructive procedures.
For Medicaid, whether you can get coverage—and how easily—will depend a lot on your state’s specific Medicaid rules.
Yes, Medicare or Medicaid may pay for surgical reconstruction of “Fenty‐fold” damage (assuming that means damage from FGM/C or similar) — but only if the surgery is medically necessary, not purely cosmetic, and you can meet the requirements (documentation, functional impairment).
The coverage is much more likely for deinfibulation (opening closed labia) than for more complex restoration (e.g., clitoral restoration), which is much more often denied.
Conclusion
The Fenty Fold highlights the severe physical toll that chronic fentanyl use can have on facial tissue, driven by the drug’s extreme potency and its effects on circulation, skin, and connective tissue. While lifestyle changes such as proper nutrition, hydration, and overall health support tissue recovery, more significant improvements often require cosmetic interventions such as dermal fillers, fat grafting, microneedling, or surgical reconstruction. Early cessation of fentanyl use, combined with a tailored medical and cosmetic plan, offers the best chance to prevent further damage and restore facial appearance, emphasizing that both recovery from addiction and repair of its physical effects are achievable with the right approach.
Video: The Hidden Dangers of Fentanyl Addiction