Suicide risk assessment in crisis counseling calls is essential for identifying individuals at immediate risk of harm and providing timely intervention. Self-management strategies help individuals recognize warning signs and practice coping skills to maintain mental well-being. Family support is crucial for emotional stabilization and safety, while community resources, like crisis hotlines and mental health services, offer essential external support. Together, these strategies create a comprehensive approach to suicide prevention, addressing both immediate needs and long-term recovery.
Suicide Risk Assessment in Crisis Counseling Calls: A Guide to Ensuring Immediate Safety and Support
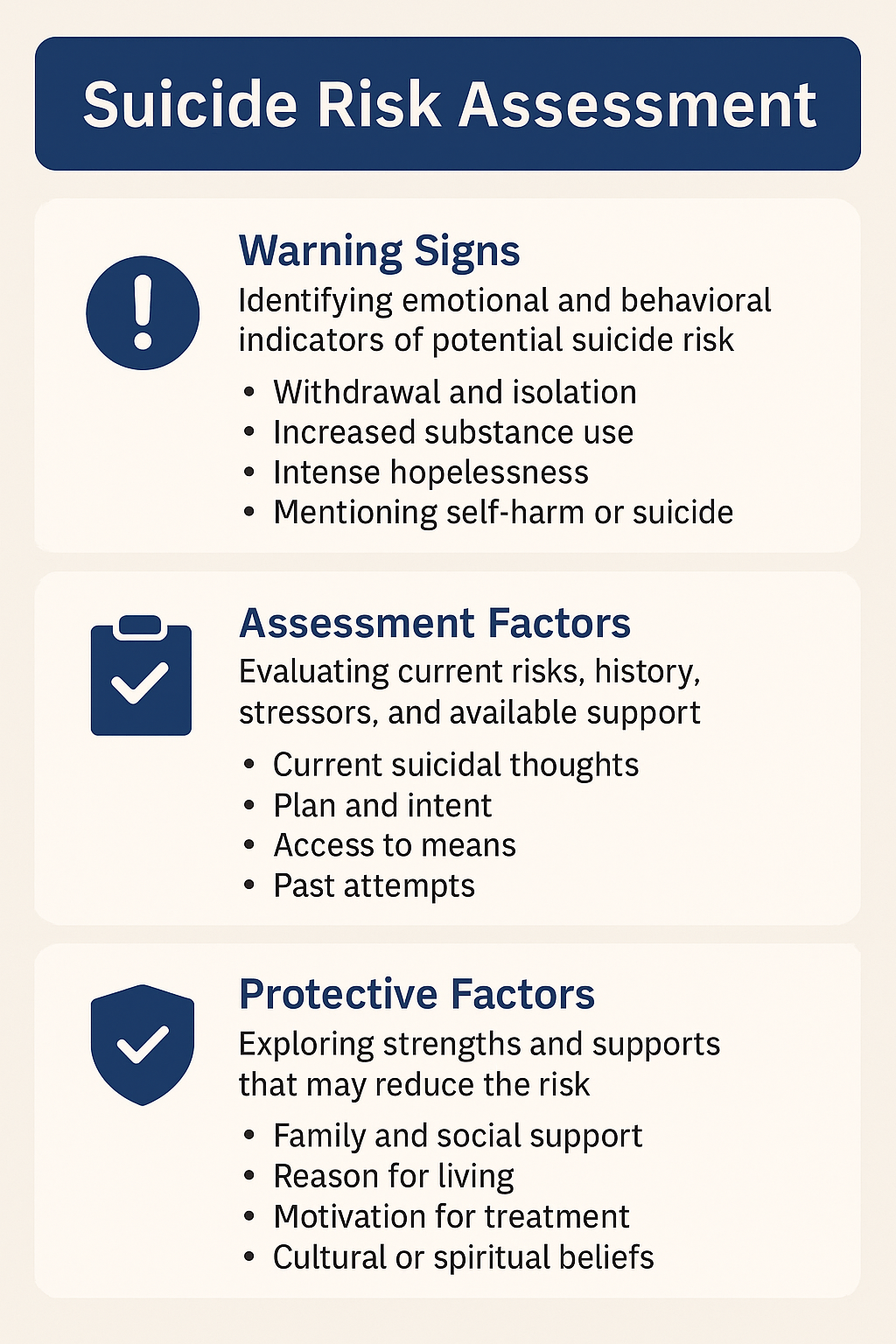
Suicide risk assessment in crisis counseling calls is a crucial process used by mental health professionals to evaluate whether an individual is at immediate risk of suicide and determine the level of intervention needed. These assessments help counselors understand the severity of suicidal ideation, identify risk and protective factors, and develop a response plan to ensure the individual’s safety. Here’s a look at the essential components of suicide risk assessment and how each step contributes to safeguarding those in crisis.
1. Evaluating Suicidal Thoughts and Intent
Presence of Suicidal Thoughts: One of the first steps is to ask direct questions to determine if the individual is experiencing suicidal thoughts. Counselors assess the frequency, duration, and nature of these thoughts to gauge the level of risk.
Suicidal Plan: It’s critical to understand if the individual has developed a specific plan, as details around a chosen method, timing, and access to means (e.g., firearms or medications) indicate a higher risk. The more concrete and immediate the plan, the more urgent the intervention needed.
Intent to Act: Counselors also assess intent by exploring whether the individual intends to act on their thoughts or feels ambivalent. Intent to act is a high-risk indicator, while ambivalence may suggest fluctuating levels of risk that still require careful monitoring and support.
2. Assessing Risk Factors
Psychiatric History: A history of mental health conditions—such as depression, bipolar disorder, schizophrenia, or Borderline Personality Disorder (BPD)—increases suicide risk, mainly if there is a history of prior suicide attempts or self-harm.
Substance Abuse: Substance use, including alcohol or drugs, can elevate suicide risk due to increased impulsivity and impaired judgment, making it more likely for someone to act on suicidal thoughts.
Recent Stressors or Trauma: Life-altering events, like losing a loved one, experiencing a relationship breakdown, or job loss, can heighten suicide risk by contributing to a sense of hopelessness.
Social Support and Isolation: Limited social support or feeling isolated can intensify feelings of hopelessness, making the individual more vulnerable to suicidal thoughts. People lacking social connections may also lack access to helpful resources in a crisis.
3. Identifying Protective Factors
Social Support: A supportive network of family and friends can serve as a significant protective factor against suicide, providing reassurance and connection.
Religious or Spiritual Beliefs: For some individuals, a belief system or strong faith can act as a deterrent against suicide, as these beliefs may offer hope, comfort, or a sense of purpose.
Personal Coping Skills: Strong coping strategies and resilience are protective factors that reduce the likelihood of suicidal behavior, enabling individuals to manage stress and crises more effectively.
Future Goals or Plans: Having future aspirations or responsibilities, such as family obligations or career goals, can anchor individuals during distressing times, reducing the likelihood of acting on suicidal thoughts.
4. Behavioral Indicators
Mood and Emotional State: A counselor assesses the individual’s emotional state, watching for signs of hopelessness, despair, guilt, or anxiety, all of which are often linked to suicidal ideation.
Withdrawal or Isolation: Behavioral changes, such as withdrawing from loved ones, neglecting daily responsibilities, or giving away personal belongings, may signal an elevated risk of suicide and require immediate attention.
5. Assessing Imminence
Short-term Risk: Crisis counselors determine the immediate risk by assessing the individual’s current emotional and mental state. If someone expresses intent to act on suicidal thoughts immediately or within hours, they are considered high-risk and in need of urgent intervention.
Long-term Risk: Some individuals may report passive suicidal ideation, such as a distant or vague desire to live no longer. While concerning, this may not require immediate intervention but indicates a need for follow-up care and monitoring.
6. Collaborative Safety Planning
Creating a Safety Plan: When risk is identified, counselors often work with the individual to develop a safety plan, including coping strategies, emergency contacts, and steps to take if suicidal thoughts intensify. This may involve securing lethal means, involving family or friends, or connecting to a mental health professional.
Referral to Crisis Intervention: If the risk is high, counselors may refer individuals for immediate intervention, such as hospitalization, emergency services, or mental health care, to ensure their safety and provide intensive support.
7. Follow-up and Monitoring
Immediate Follow-Up: Crisis counselors often check in with the individual through follow-up calls or referrals to long-term therapy. This continued support can be essential in the days and weeks following a crisis.
Continuous Monitoring: Ongoing support and monitoring are crucial for individuals at risk. This might involve connecting them with additional resources, support groups, or outpatient therapy to address underlying factors and reduce the likelihood of future crises.
In summary, a suicide risk assessment in crisis counseling is designed to thoroughly understand an individual’s risk level, identify factors that increase or reduce that risk, and take immediate action to ensure safety. By combining structured questioning with empathy; counselors can gain a comprehensive view of the individual’s situation and create a plan that includes immediate intervention and longer-term support. With this approach, crisis counselors not only help prevent suicide in the short term but also connect individuals to resources that foster resilience, coping, and hope for the future.
Self-Management Strategies to Identify Suicide Risk in Crisis Situations
While mental health professionals often conduct suicide risk assessments, individuals can also develop self-management strategies to identify signs of distress in themselves or others and address them proactively. Recognizing and managing early warning signs, emotional regulation, and knowing when to seek help can prevent crises from escalating. Here are key strategies for identifying suicide risk in crises:
1. Develop Emotional Awareness
Recognize Warning Signs in Emotions: Be aware of emotional changes, such as intense sadness, feelings of hopelessness, or worthlessness. Experiencing emotional numbness or overwhelming stress can signal heightened suicide risk.
Monitor Mood Changes: Drastic mood swings or irritability may indicate that someone is struggling with thoughts of self-harm or suicidal ideation. Awareness of these shifts is crucial to intervening early.
2. Self-Monitoring of Thoughts
Identify Suicidal Thoughts: Reflect regularly on your thoughts. Thoughts such as “I wish I were dead” or “I can’t handle this anymore” are severe indicators of suicidal ideation. Awareness of these thoughts helps ensure timely intervention.
Assess for Specific Plans or Intent: If you notice thoughts developing into a plan, such as a method or a timeline, this indicates increased risk. Recognizing a plan early allows for action before it escalates.
3. Recognize Behavioral Indicators
Notice Changes in Behavior: Withdrawal from social interactions, neglecting daily activities, or engaging in risky behaviors may indicate an increased risk of suicide. Paying attention to these changes is crucial to prevent harm.
Observe Self-Destructive Behaviors: Self-harm or substance abuse can be linked to suicidal ideation. Taking these behaviors seriously can help individuals recognize their need for support.
4. Assess Risk Factors
Identify Personal Risk Factors: Mental health conditions like depression, anxiety, and Borderline Personality Disorder (BPD) can elevate risk, as can substance dependency or a history of trauma. Understanding your risk factors helps with early identification.
Recognize Contextual Stressors: Life changes such as a job loss or a breakup can trigger suicidal thoughts. Being mindful of these external factors can help individuals recognize potential crises early.
5. Strengthen Coping Mechanisms
Develop Emotional Regulation Skills: Learning to manage intense emotions—through mindfulness, breathing exercises, or grounding techniques—can reduce the emotional overwhelm that often accompanies suicidal thoughts.
Create Healthy Outlets for Stress: Regular stress management practices, like exercise, hobbies, or social activities, offer release for built-up tension and help prevent harmful coping mechanisms.
6. Engage in Reflective Journaling or Thought Records
Track and Reflect on Thoughts and Emotions: A journal can help individuals observe patterns in their emotions and thoughts, allowing them to catch early signs of distress and address recurring issues.
Document Feelings Regularly: Reflecting on past moments of distress provides insight into triggers and patterns, making it easier to recognize warning signs.
7. Use Suicide Risk Assessment Tools
Self-Assessment Tools: Many online resources or tools, like the PHQ-9 Depression Scale, help individuals assess their mood and risk factors. Although not substitutes for professional care, these can help identify when support may be needed.
Evaluate Frequency and Intensity of Suicidal Thoughts: Self-assessment tools focus on suicidal thoughts’ frequency and intensity, enabling early recognition of warning signs.
8. Build a Personal Safety Plan
Create a Crisis Plan: A plan is essential for moments of heightened risk. A safety plan should include:
- Reaching out to trusted individuals or professionals
- Utilizing coping strategies (e.g., grounding exercises)
- Listing emergency contacts (such as a helpline)
- Securing potentially dangerous items (e.g., medications, firearms)
Preemptive Steps: Acting quickly when feeling overwhelmed can prevent impulsive behaviors and allow time to seek support.
9. Engage in Support Networks
Reach Out for Support: Regular check-ins with trusted people can provide early warnings if they notice changes in behavior or emotions, offering a safety net during challenging times.
Participate in Support Groups: Peer support groups help with personal challenges and provide a community of people facing similar issues, which can reduce isolation.
10. Seek Professional Help
Therapeutic Intervention: If self-management strategies indicate suicide risk, reaching out to a mental health professional is essential. Therapy can provide the right interventions and build resilience.
Crisis Intervention: In urgent cases, contacting a counselor or visiting an emergency room ensures immediate support and prevents escalation.
In summary, self-management strategies for identifying suicide risk involve building self-awareness, understanding personal triggers, and developing a safety plan. By recognizing warning signs early, individuals can take action to prevent crises from worsening. Maintaining strong social connections, managing stress effectively, and seeking professional support when necessary are all vital components of managing suicide risk and fostering long-term resilience.
Family Support Strategies in Suicide Risk Assessment During Crisis Counseling Calls
Family support plays a pivotal role in suicide risk assessment during crisis counseling calls. Families can provide crucial emotional support, ensure immediate safety, and encourage long-term recovery. Effective family involvement helps stabilize individuals in crisis, address their immediate needs, and lay a foundation for healing. Here are critical strategies for family support during suicide risk assessment:
1. Encouraging Open Communication
Foster Honest Conversations: Families should create a safe and non-judgmental environment where individuals feel comfortable discussing their thoughts and feelings. This openness helps identify suicidal thoughts and allows for emotional expression.
Active Listening: Family members should listen attentively and without judgment, showing empathy and validating the individual’s feelings. This approach reduces feelings of isolation and fosters a sense of connection.
2. Recognizing Warning Signs and Risk Factors
Educate on Warning Signs: Families should understand the common signs of suicidal ideation, such as withdrawal, hopelessness, or sudden mood changes. Recognizing these signs early can enable timely intervention.
Identify Contributing Factors: Family members should be aware of personal factors that might heighten suicide risk, including mental health issues, substance abuse, relationship challenges, or traumatic experiences. Understanding these factors can help families provide relevant support.
3. Promoting Immediate Safety
Remove Access to Lethal Means: Family members should secure or remove items that could facilitate self-harm, like firearms, medications, or sharp objects, to prevent impulsive actions during intense moments of distress.
Provide Supervision and Presence: In high-risk situations, families may need to stay close to the individual, ensuring they’re not left alone during critical times. Continuous support can help prevent harm.
Ensure Immediate Support: If the person expresses an active suicide plan, family members should encourage or arrange for immediate intervention, whether by calling emergency services, contacting a crisis helpline, or visiting a hospital.
4. Coordinating with Crisis Counselors and Professionals
Collaborate with Professionals: Families can play an active role in the assessment process by sharing observations about the individual’s behavior and emotional state. Their insights may help the counselor gauge risk and recommend appropriate care.
Follow Counselor Guidance: Families should be open to the recommendations of crisis counselors, whether that involves arranging mental health support or other interventions. Following this guidance ensures the individual receives comprehensive care.
5. Establishing a Supportive Environment
Create a Stable Home Environment: Families should foster a nurturing, supportive space where the individual feels valued. Providing reassurance, encouragement, and consistent support can reinforce stability and hope.
Reinforce Hope and Recovery: Families should emphasize that recovery is possible and encourage their loved ones to seek ongoing treatment. This optimism can help counter feelings of hopelessness.
6. Building a Safety Plan
Develop a Personalized Crisis Plan: Families can work with the individual and counselors to develop a safety plan, which may include emergency contacts, coping strategies, and steps to take if suicidal thoughts arise. This plan offers guidance during moments of crisis.
Establish a Support Network: It’s essential to ensure the individual has a reliable support system, whether that includes trusted friends, family, or counselors they can reach out to in difficult moments.
7. Monitoring and Ongoing Support
Regular Check-Ins: Family members should maintain regular contact, especially in the days and weeks following a crisis, to monitor the individual’s emotional well-being and identify signs of deterioration.
Participate in Support Groups or Therapy: Families may benefit from attending support groups or therapy. These resources help family members understand suicide risk, develop supportive skills, and manage the stress of caregiving.
8. Encouraging Long-Term Treatment and Follow-Up
Encourage Adherence to Treatment: Families can play a critical role in motivating the individual to engage consistently with therapy, psychiatry, or medication. This support helps reduce the risk of relapse or future crises.
Reinforce the Importance of Recovery: Families should remind their loved ones that managing suicidal thoughts takes time and encourage long-term commitment to treatment. Highlighting the possibility of improvement can offer a needed boost to motivation.
9. Addressing Family Dynamics
Improve Communication Within the Family: If family dynamics contribute to distress, seeking family therapy can benefit everyone. This approach can reduce conflict, enhance communication, and foster a more supportive environment.
Seek Professional Guidance for Complex Family Situations: In complicated family dynamics, professional guidance can help ensure the family functions in a supportive way. Family therapy may be vital when a history of abuse, trauma, or dysfunction exists.
In summary, family involvement is essential in suicide risk assessment during crisis counseling calls. Families can provide critical support by recognizing warning signs, reducing risks, and coordinating with mental health professionals. By fostering a stable and supportive environment, families help individuals navigate crisis periods and work toward long-term recovery. Adequate family support not only aids immediate safety but also builds a foundation for healing, resilience, and hope for a better future.
Community Resource Strategies in Suicide Risk Assessment During Crisis Counseling Calls
Connecting individuals at risk of suicide with community resources during crisis counseling calls is vital for immediate intervention, ongoing care, and long-term support. Crisis counselors rely on local resources to enhance safety, reduce isolation, and provide specialized care, especially during suicide risk assessments. Here’s a look at the essential community resource strategies that counselors can leverage to support individuals at risk:
1. Referral to Crisis Hotlines and Helplines
National and Local Suicide Prevention Helplines: Crisis counselors should keep information on helplines like the National Suicide Prevention Lifeline (988) and other region-specific numbers. These resources provide 24/7 access to trained professionals, ensuring individuals can reach out during emergencies.
Text and Chat Services: For those uncomfortable with phone calls, services like the Crisis Text Line offer confidential texting options. Referrals to these services provide an accessible means for individuals to receive support in a safe and approachable way.
2. Emergency Medical Services and Crisis Intervention Teams
Emergency Response Teams: In cases of immediate danger, crisis counselors may need to contact emergency services or activate Crisis Intervention Teams (CITs) trained to handle mental health crises. CIT members are often skilled at de-escalating situations and ensuring individuals receive urgent care.
Hospitalization: When someone is at high risk, referral to a psychiatric hospital or crisis stabilization unit may be necessary for their safety. Hospitals provide intensive monitoring and treatment, creating a controlled environment for recovery.
3. Connection to Mental Health Services
Psychiatric Care: Crisis counselors can refer individuals to mental health professionals for urgent evaluation and management. Psychiatric care offers diagnosis, therapy, and medication as needed to address underlying conditions contributing to suicidal thoughts.
Therapists and Counselors: Local mental health clinics and individual therapists can provide continuous therapeutic support, helping individuals develop coping mechanisms to prevent future crises.
4. Support Groups and Peer Support Networks
Suicide Loss Support Groups: Many communities offer support groups for those grieving a loved one’s suicide. These groups provide emotional support and understanding, helping individuals process loss and find a sense of belonging.
Peer Support Programs: Peer groups connect individuals facing similar struggles, offering mutual understanding and reducing isolation. These groups, often led by peers or facilitated by mental health professionals, provide a supportive environment for people managing suicidal ideation.
5. Community Mental Health Centers
Local Crisis Centers: Some areas offer walk-in psychiatric assessments, immediate stabilization, and referrals to further care. These centers help individuals access critical support without the barriers of traditional appointments.
Mobile Crisis Units: Available in certain regions, mobile crisis teams offer on-site assistance. Staffed with mental health professionals, these teams provide support where individuals feel most comfortable, often helping those who might otherwise not seek care.
6. Social Services and Safety Net Programs
Financial and Housing Assistance: For those dealing with financial hardships or homelessness, social services can provide essential support, reducing some of the underlying stressors linked to suicidal thoughts.
Legal Services: Legal challenges like custody disputes or domestic violence can exacerbate a mental health crisis. Referring individuals to legal aid services can address some of these stressors, aiding overall crisis management.
7. Culturally Relevant Services
Culturally Specific Support: Referrals to culturally sensitive resources, like ethnic or LGBTQ+ community centers, provide tailored support for underserved populations, helping individuals feel seen and understood.
Religious or Spiritual Support: Faith-based organizations offer counseling and support groups for individuals seeking spiritual guidance. These services can provide comfort, guidance, and a sense of purpose to individuals experiencing distress.
8. School-Based Resources
School Counselors and Mental Health Programs: Counselors can refer youth to on-campus resources. Schools often have trained counselors to assess and connect students with additional mental health services.
Youth Suicide Prevention Programs: Many schools offer programs that educate students and staff on recognizing suicide risk signs and accessing support. These initiatives play an essential role in reducing stigma and encouraging early intervention.
9. Ongoing Follow-Up and Case Management
Community-Based Case Management: For individuals needing long-term care, case managers coordinate resources, ensuring continuous access to therapy, medication, and social services. Case management is vital for those struggling with continuity of care.
Aftercare Programs: Some organizations offer aftercare services for individuals leaving emergency or psychiatric care, providing continued check-ins and connections to local resources. This helps ease the transition into daily life and reduces the risk of re-entry into crisis.
10. Public Awareness Campaigns and Education
Community Education: Public campaigns on suicide prevention and mental health help reduce stigma and encourage people to seek help. By promoting awareness of warning signs and available resources, communities empower individuals to respond effectively to those at risk.
In summary, community resource strategies during suicide risk assessments allow crisis counselors to support individuals with a network of care tailored to their needs. By connecting them with immediate crisis services, ongoing mental health support, peer groups, and social services, counselors ensure those at risk have access to comprehensive support. These strategies create a safety net, offering care that addresses immediate risk, supports long-term recovery, and fosters a community aware of the importance of suicide prevention.
Conclusion
Suicide risk assessment in crisis counseling calls is a vital first step in identifying individuals at risk and providing immediate intervention. Individuals can better cope with distress and manage emotions by integrating self-management strategies, while family support offers crucial stability and safety. Additionally, community resource strategies ensure access to essential services and long-term support. Together, these approaches create a holistic and effective response to suicide prevention, emphasizing immediate care, emotional support, and ongoing resources for recovery.
Video: Is Someone You Know at RISK of Suicide?