Sleep issues are common during detoxification, caused by disruptions in brain pathways that regulate neurotransmitters like GABA, dopamine, and serotonin. These changes often lead to insomnia and poor sleep quality. Managing sleep problems involves self-care practices such as good sleep hygiene, family support in creating a stable environment, and community resources, such as counseling and support groups. Together, these strategies help improve sleep and support recovery.
Sleep and Opioid Detox: Why Rest Is a Critical Medicine for Recovery
🛌 Sleep and Opioid Detox: A Vital Yet Overlooked Part of Recovery
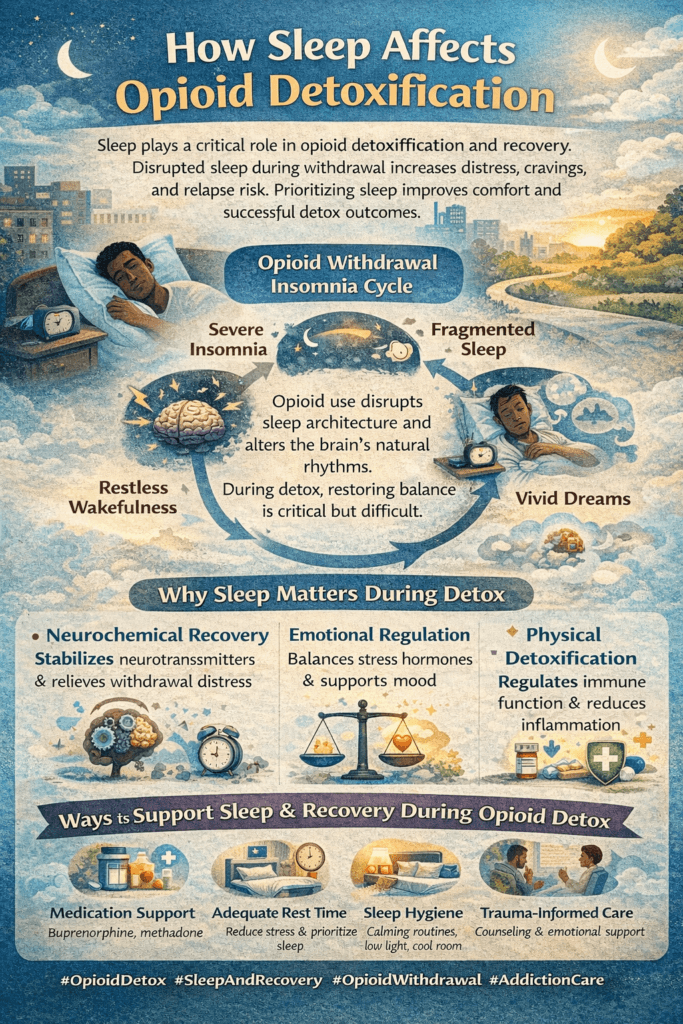
Sleep plays a critical role in opioid detoxification and long-term recovery—both physiologically and psychologically. Unfortunately, it’s also one of the first things to break down during withdrawal. Many individuals in detox suffer from severe sleep disturbances just when their bodies and brains need rest the most.
Here’s how sleep and opioid detoxification are closely intertwined—and why addressing sleep is essential for healing and relapse prevention:
😴 1. Opioid Withdrawal Severely Disrupts Sleep
Sleep problems are among the most common—and distressing—symptoms during detox. These may include:
- Insomnia
- Fragmented or shallow sleep
- Restless leg syndrome
- Vivid nightmares
For many, these disruptions don’t end when acute withdrawal fades. In Post-Acute Withdrawal Syndrome (PAWS), sleep problems can last weeks or months.
Why it matters:
Sleep loss intensifies other withdrawal symptoms—like anxiety, irritability, and impulsivity. This makes it harder to cope, increasing the risk of relapse.
🧬 2. Sleep Is When the Brain Repairs Itself
Opioid use disrupts essential brain systems, including:
- The hypothalamic-pituitary-adrenal (HPA) axis (which regulates stress)
- Dopamine and serotonin pathways (linked to mood and motivation)
- Pain processing circuits
During sleep—profound sleep—the body engages in:
- Neurotransmitter replenishment
- Hormonal balancing
- Immune system recovery
- Cellular detox and repair
Good sleep = faster emotional and neurological recovery.
🔁 3. Sleep Loss Can Reinforce the Addiction Cycle
When you don’t sleep well:
- Stress levels rise
- Impulse control drops
- Cravings increase
Sleep-deprived brains are more likely to seek short-term relief—like opioids—to feel “normal” again. Complicating matters, opioids themselves disrupt regular sleep cycles, suppressing REM and slow-wave sleep.
This creates a dangerous loop: using opioids to sleep, then needing sleep because of withdrawal.
🧘 4. Supporting Sleep During Detox Can Prevent Relapse
Treating sleep is not secondary—it’s foundational. Effective strategies include:
🛏️ Sleep Hygiene
- Consistent sleep schedule
- Dark, cool, quiet bedroom
- Avoid caffeine and screens before bed
💊 Medication Support
- Non-addictive aids like trazodone, hydroxyzine, or clonidine
🧠 Behavioral Therapies
- Cognitive Behavioral Therapy for Insomnia (CBT-I)
🧘 Mindfulness and Relaxation
- Meditation
- Deep breathing
- Guided imagery
These approaches can ease sleep onset and improve quality over time.
In summary, sleep isn’t a luxury during opioid detox—it’s a core part of recovery. It helps regulate mood, balance stress hormones, repair brain chemistry, and reduce the risk of relapse. By addressing sleep problems early, individuals in recovery have a much better chance at long-term success.
Insomnia During Opioid Detox: How Withdrawal Disrupts the Brain’s Sleep Systems
Insomnia and the Brain in Opioid Detox: Understanding the Neurological Roots of Sleeplessness
Sleep is one of the first casualties of opioid withdrawal. Many individuals going through detox experience intense insomnia—difficulty falling asleep, staying asleep, or getting restful, restorative sleep. But why?
During opioid detoxification, several brain systems that regulate sleep, stress, and emotional stability become disrupted. The result: a brain stuck in overdrive, unable to power down—even when the body is exhausted.
Below is a breakdown of the central brain pathways affected by insomnia during opioid withdrawal:
🧠 1. HPA Axis – Stress Regulation
What it does:
The hypothalamic-pituitary-adrenal (HPA) axis manages the body’s stress response and influences the circadian rhythm.
During detox:
The HPA axis becomes overactive, producing excessive cortisol (the stress hormone), which results in:
- Hyperarousal
- Difficulty falling asleep
- Nighttime awakenings
💥 Why it matters: The brain stays on high alert, making it nearly impossible to wind down.
🧠 2. VLPO – Sleep Initiation Center
What it does:
The ventrolateral preoptic nucleus (VLPO), located in the hypothalamus, promotes sleep by releasing GABA, a calming neurotransmitter that quiets the brain’s arousal centers.
During detox:
Long-term opioid use impairs GABA signaling and suppresses VLPO activity, making it harder for the brain to “switch off.”
😵 Result: The brain forgets how to enter sleep mode naturally.
🧠 3. Orexin System – Arousal and Wakefulness
What it does:
Orexin (hypocretin) keeps the brain awake and alert.
During detox:
The orexin system becomes dysregulated, leading to:
- Nighttime hyper-alertness
- Increased sensitivity to noise or stress
- Difficulty staying asleep
🔥 Even small thoughts or disturbances can jolt the brain awake.
🧠 4. Locus Coeruleus – Norepinephrine and Fight-or-Flight
What it does:
This brain region releases norepinephrine, a neurotransmitter linked to alertness, anxiety, and arousal.
During detox:
The locus coeruleus (LC) becomes hyperactive, flooding the brain with norepinephrine:
- Racing thoughts
- Restlessness and panic
- Blocked entry into deep sleep
🚫 It’s like the brain is stuck in fight-or-flight mode all night long.
🧠 5. Dopamine Pathways – Mood and Motivation
What they do:
The dopaminergic system (including the nucleus accumbens and ventral tegmental area) controls mood, pleasure, and drive.
During detox:
Dopamine levels plummet, causing:
- Low mood and emotional flatness (anhedonia)
- Poor daytime energy and rhythm
- Cravings for opioids to ease discomfort or “help sleep.”
📉 Low dopamine worsens both daytime fatigue and nighttime insomnia.
🧠 6. Thalamocortical Pathways – Sleep Architecture Control
What they do:
These pathways control transitions between sleep stages (like REM and deep sleep).
During detox:
Opioid withdrawal disrupts this system, leading to:
- Reduced REM sleep
- Suppressed slow-wave (deep) sleep
- Lighter, fragmented rest
⏳ Even if you fall asleep, it’s often not restorative.
🧠 Summary: Why Sleep Feels Impossible During Detox
Insomnia during opioid detox isn’t just a symptom—it’s a result of profound neurological disruption. Affected systems include:
- Stress regulators: HPA axis, locus coeruleus
- Sleep centers: VLPO, thalamus
- Key neurotransmitters: GABA, dopamine, norepinephrine
This imbalance creates a brain that’s alert, anxious, and dysregulated—precisely the opposite of what it needs for restful sleep.
🛠️ What Helps?
Understanding these systems helps guide better treatment strategies:
- Sleep hygiene: regular routines, screen limits, quiet environments
- Non-habit-forming sleep medications: e.g., trazodone, hydroxyzine
- CBT-I (Cognitive Behavioral Therapy for Insomnia)
- Mindfulness and relaxation practices
- Family and community support during early recovery
🌙 Final Thought
Sleep during detox isn’t just comfort—it’s recovery in action. Addressing insomnia early not only improves quality of life but also reduces relapse risk and helps the brain heal. Restoring sleep is one of the most important—and treatable—steps in opioid addiction recovery.
10 Proven Self-Management Strategies for Sleep During Opioid Detox
Restoring Rest: Practical Sleep Strategies for Opioid Detox and Recovery
Sleep disruptions are among the most challenging symptoms during opioid detoxification. Insomnia, restlessness, and fragmented sleep often persist due to withdrawal’s impact on brain chemistry, mood, and physical well-being.
But the good news? You can take action. The following self-management strategies are designed to restore sleep by addressing the biological, psychological, and behavioral disruptions caused by opioid withdrawal—and they support your long-term recovery.
😴 Self-Management Strategies for Better Sleep During Detox
🧘 1. Mindfulness & Relaxation Techniques
What to do:
Practice deep breathing, progressive muscle relaxation, or guided meditation before bedtime.
Why it works:
Calms an overactive nervous system, lowers stress hormones like cortisol and norepinephrine, and reduces anxiety.
Helpful tools:
Apps like Calm, Headspace, or Insight Timer offer free guided meditations.
🛏️ 2. Consistent Sleep-Wake Schedule
What to do:
Wake up and go to bed at the same time every day, even after a rough night.
Why it works:
Stabilizes your circadian rhythm, which is often disrupted during opioid withdrawal.
🕗 Remember: Consistency matters more than total sleep time.
☀️ 3. Morning Sunlight Exposure
What to do:
Spend 10–20 minutes outside in natural sunlight within an hour of waking.
Why it works:
Strengthens natural sleep-wake cues and boosts serotonin, improving both mood and sleep.
🚶 4. Daytime Movement
What to do:
Engage in light activity like walking, stretching, or gentle yoga.
Why it works:
Reduces restlessness, builds sleep pressure, and enhances mood regulation.
⚠️ Avoid intense workouts within 2–3 hours of bedtime.
🍵 5. Limit Caffeine and Stimulants
What to do:
Avoid caffeine, nicotine, and energy drinks after 2:00 PM.
Why it works:
These substances block adenosine and other sleep-promoting neurotransmitters, worsening anxiety and insomnia.
📴 6. Cut Back on Evening Screen Time
What to do:
Turn off screens at least 1 hour before bed.
Why it works:
Blue light suppresses melatonin, the body’s natural sleep hormone.
🌙 Try a “digital sunset” ritual with journaling, music, or reading instead.
📝 7. Use a Sleep Journal or Brain Dump
What to do:
Write down thoughts, worries, or to-do lists before bed.
Why it works:
Clears mental clutter and reduces rumination—a significant cause of insomnia during detox.
🌿 8. Consider Non-Habit-Forming Sleep Aids (If Needed)
Options:
- Melatonin
- Magnesium glycinate
- Herbal teas: Chamomile, valerian root
- Medications like trazodone or hydroxyzine (only under medical supervision)
Why it works:
Provides rest without addictive risks. Especially important for those on Medication-Assisted Treatment (MAT) like Suboxone.
🌡️ 9. Optimize Your Sleep Environment
Create a space that promotes rest:
- Cool temperature: 60–67°F (15–19°C)
- Darkness: Blackout curtains or eye masks
- Quiet: Use white noise, a fan, or earplugs
- Minimal clutter: A tidy space supports calm
Your environment talks to your nervous system—keep it peaceful.
🧠 10. Practice Sleep Acceptance, Not Perfection
What to do:
Remind yourself: “Even resting without sleep helps me recover.”
Why it works:
Eases the pressure to sleep, which can create anxiety and prolong insomnia.
🌿 Focus on healthy routines, not just hours slept. Sleep will gradually improve as the brain heals.
✅ Final Thoughts
Insomnia during opioid detox is deeply connected to brain chemistry—but you’re not powerless. These self-management strategies support the body’s natural healing and help re-establish a stable sleep pattern without relying on substances.
With patience, consistency, and self-compassion, sleep can become a powerful ally in your recovery journey.
Family Support Strategies for Insomnia During Opioid Detox
Supporting Rest: How Families Can Help Loved Ones Sleep During Opioid Withdrawal
Sleep is one of the most disrupted functions during opioid detox. Anxiety, hyperarousal, and imbalanced brain chemistry make it hard for the body and mind to rest. But family members play a critical role in supporting healthy sleep habits.
These family-based strategies are practical, compassionate, and rooted in neuroscience and behavioral support.
🛏️ 1. Create a Calm and Sleep-Friendly Environment
- Keep the home quiet, especially during the person’s sleep hours.
- Use soft lighting in the evening to help the brain wind down.
- Help limit stimulation, such as loud TV, phone calls, or active conversations.
- Use blackout curtains or white noise machines to minimize disruption.
🧠 Why it works: Reduces sensory overload and supports melatonin production, a key hormone for sleep.
🧘 2. Encourage Calming Nighttime Routines
- Support relaxing activities before bed, like:
- Gentle music or meditation
- Light stretching
- Journaling, reading, or quiet art
- Join them in a screen-free hour before bed as a family ritual.
🧠 Why it works: Creates consistent wind-down cues that tell the brain it’s time to sleep.
💬 3. Practice Patient, Reassuring Communication
- Avoid saying things like “Just go to sleep” or “You’ll feel better in the morning.”
- Validate the struggle: “I know sleep is hard right now. You’re doing your best.”
- Reassure gently: “This is temporary. You’re healing—even if it doesn’t feel like it.”
🧠 Why it works: Reduces anxiety and internal pressure that worsen insomnia.
🔄 4. Help Reinforce a Consistent Routine
- Encourage regular wake-up and bedtime every day.
- Start the morning together with sunlight or coffee to cue the circadian rhythm.
- Avoid letting them nap excessively or sleep all day, even if their sleep is poor.
🧠 Why it works: Helps reset biological clocks that have been disrupted by substance use.
⚠️ 5. Avoid Enabling or “Rescue” Behaviors
- Never offer alcohol, sedatives, or substances to help them sleep.
- Stick to routines and healthy boundaries—even when they’re irritable.
- Gently redirect toward evidence-based strategies instead of shortcuts.
🧠 Why it works: Reinforces long-term coping over short-term fixes.
🤝 6. Be a Nighttime Accountability Partner (If Invited)
- Offer to check in: “What’s your plan for winding down tonight?”
- Help them limit screens, social media, or triggering content before bed.
- Be available for a calm chat if they’re struggling late at night.
🧠 Why it works: Supports emotional regulation and reduces nighttime loneliness.
📘 7. Learn Together About Sleep in Recovery
- Read articles or watch videos together about sleep and detox.
- Join family support groups (e.g., Al-Anon, SMART Recovery Family & Friends).
- Consult a counselor about supporting without enabling.
🧠 Why it works: Informed families are more effective, confident, and emotionally steady.
📅 8. Support Daytime Wellness Habits
- Encourage gentle exercise, balanced meals, and hydration.
- Invite them to join you for a walk or shared household task.
- Address mood symptoms (like anxiety or depression) that affect sleep.
🧠 Why it works: A healthier day creates the foundation for better sleep at night.
💡 Bonus Tip for Caregivers
If you’re supporting someone in detox, take care of your own sleep and stress levels, too.
Your calm presence is one of the most powerful tools you can offer.
Final Thought:
Sleep doesn’t heal overnight—but consistent, compassionate support makes a world of difference. Families who understand the sleep challenges of detox can become vital allies in recovery.
9 Powerful Community Resources to Help Manage Insomnia During Detox
1. 🧠 Outpatient & Medical Detox Programs
These programs not only manage withdrawal symptoms, but many also monitor and address sleep disturbances. With access to licensed professionals, individuals can receive short-term sleep medications (when appropriate), nutritional support, and sleep hygiene education. Some programs also offer evening check-ins or low-stimulation recovery environments to aid rest.
2. 🤝 Peer Support Groups (AA, NA, SMART Recovery, Refuge Recovery)
Late-night cravings and anxiety are common during detox. Peer-led recovery meetings—especially online or in-person evening groups—create safe spaces to share, feel heard, and stay accountable. Many people fall asleep more easily after a group where they expressed emotions and connected with others who understand.
3. 🛏️ Sober Living Homes
Transitional housing offers more than sobriety—it supports routine, which is key to repairing sleep. These homes have curfews, quiet hours, and morning structure, all of which help reset the circadian rhythm. Living in a substance-free environment also reduces triggers that cause late-night anxiety or restlessness.
4. 🧘 Community Wellness Centers & Recovery Yoga Programs
Many local wellness centers (especially those focused on trauma-informed care or recovery) offer free or low-cost classes in meditation, gentle movement, breathwork, or yoga nidra. These practices reduce cortisol and help regulate the nervous system—making it easier to fall and stay asleep without substances.
5. 🩺 Sleep Clinics & Cognitive Behavioral Therapy for Insomnia (CBT-I)
Sleep clinics or therapists trained in CBT-I offer evidence-based support for people in recovery. CBT-I helps retrain the brain to associate bedtime with sleep instead of anxiety or cravings. It’s especially effective for people who are avoiding sleep medications due to addiction risk.
6. 📱 24/7 Crisis & Emotional Support Lines
Organizations such as SAMHSA, 988 Lifeline, and Warm Lines provide real-time support during sleepless nights. Talking to a trained peer or counselor at 2 am can lower anxiety, reduce the urge to use, and create emotional safety when the rest of the world is asleep.
7. 🎨 Libraries, Art Spaces & Recovery Community Centers
Calming creative outlets and low-stimulation environments—like late-evening art groups, journaling workshops, or speaker events—help relieve stress before bed. Many recovery hubs have nighttime programming that encourages connection without overstimulation.
8. 💼 Vocational Programs & Daytime Structure Support
Daytime activity directly impacts nighttime rest. Job training programs, volunteer groups, GED classes, or community work placements keep the body and brain active. A consistent daytime rhythm reduces oversleeping and napping, leading to a stronger sleep drive at night.
9. 🌿 Faith-Based & Spiritual Recovery Groups
Evening prayer circles, guided meditations, or spiritual mentorship within faith communities can ease mental tension, offer grounding, and build connection. For those who find comfort in faith or spirituality, these groups reduce nighttime loneliness and provide hope during hard detox nights.
Frequently Asked Questions
Here are some common questions:
Question: Provide a sleep hygiene checklist for detox.
Answer: practical and recovery-friendly Sleep Hygiene Checklist for Detox — designed specifically for people going through opioid withdrawal. This checklist supports natural sleep regulation, calms the nervous system, and helps reduce the risk of relapse.
Let me know if you’d like this in a printable PDF with calming colors and icons!
💤 Sleep Hygiene Checklist During Opioid Detox
✅ Use this checklist daily to support better sleep and healing during recovery.
🌙 Bedtime Routine (1–2 Hours Before Sleep)
- Dim the lights to signal “winding down” to the brain
- Take a warm shower or bath to relax muscles
- Do a calming activity (e.g., light reading, journaling, meditation)
- Avoid screen time (TV, phone, tablet) at least 60 minutes before bed
- Try herbal tea (e.g., chamomile or lemon balm) if approved by your provider
- Use calming scents like lavender or eucalyptus (optional)
🧠 Mental & Emotional Wind-Down
- Practice deep breathing or a short guided meditation
- Use a worry journal to write out stress or racing thoughts
- Repeat a calming affirmation (e.g., “My body is healing,” “Sleep will come in time”)
- Avoid heavy conversations or emotionally triggering content at night
🛏️ Sleep Environment Setup
- Keep the room cool, dark, and quiet
- Use blackout curtains or an eye mask if light is a problem
- Use white noise, a fan, or calming music if silence feels uncomfortable
- Keep the bed for sleep only (avoid eating, scrolling, or watching TV in bed)
☀️ Daytime Habits That Improve Sleep
- Wake up at the same time every day, even on weekends
- Get natural sunlight within 30–60 minutes of waking up (10–15 minutes outdoors)
- Do some gentle physical activity (e.g., walking, yoga)
- Avoid caffeine or stimulants after 2:00 PM
- Avoid naps longer than 30 minutes (or skip them if possible)
⚠️ Avoid These Before Bed
- No nicotine, caffeine, or energy drinks 4–6 hours before bed
- No large meals or sugary snacks right before sleeping
- No doomscrolling or emotionally intense TV or news
- Avoid using substances like alcohol, THC, or sedatives unless prescribed
💬 Optional Coping Supports
- Talk to a recovery peer, counselor, or sponsor if nighttime cravings increase
- Discuss sleep aids with a doctor (non-habit-forming medications may help)
- Attend support meetings (e.g., NA, SMART) to process triggers
- Keep a “bad night ≠ , bad day” mindset — recovery is still happening
📌 Final Reminder:
Sleep may take time to normalize during detox. That’s okay.
Be patient, stay consistent, and support your body with rest even when sleep is difficult.
Question: Provide a self-management toolkit.
Answer: A complete and user-friendly Sleep Self-Management Toolkit designed for individuals experiencing sleep issues during opioid detoxification and early recovery. It includes evidence-based tools to support rest, regulate the nervous system, and reduce the risk of relapse.
Sleep Self-Management Toolkit
For Use During Opioid Detox and Early Recovery
🧠 SECTION 1: Understanding Your Sleep Patterns
📝 Sleep Tracker (Use Daily)
| Date | Bedtime | Wake Time | Hours Slept | Sleep Quality (1–5) | Notes (Dreams, Waking, Cravings) |
|---|---|---|---|---|---|
🔄 SECTION 2: Sleep Hygiene Checklist
Daily Sleep Habits
✔️ [ ] Same bedtime and wake time every day
✔️ [ ] Morning sunlight exposure (10–20 min)
✔️ [ ] Gentle physical activity (yoga, walk)
✔️ [ ] No caffeine or nicotine after 2 PM
✔️ [ ] No naps over 30 min or after 3 PM
Evening Routine (1–2 Hours Before Bed)
✔️ [ ] Screens off or use blue light filters
✔️ [ ] Take a warm bath or shower
✔️ [ ] Journal or “brain dump” stressors
✔️ [ ] Do relaxation (e.g., breathing or body scan)
✔️ [ ] Try herbal tea (chamomile, lemon balm)
Sleep Environment
✔️ [ ] Dark (curtains/eye mask)
✔️ [ ] Cool (60–67°F / 15–19°C)
✔️ [ ] Quiet or white noise
✔️ [ ] Comfortable bedding
🧘 SECTION 3: Nighttime Coping Skills
Grounding Exercises
- 5-4-3-2-1 Senses Technique
- Cold water splash or an ice cube in the hand
- Visualization (e.g., peaceful forest or beach)
Breathing Techniques
- Box Breathing (4-4-4-4 count)
- 4-7-8 Breathing for calming
Affirmations
- “This discomfort is temporary.”
- “My brain and body are healing.”
- “Rest is helpful, even without full sleep.”
💊 SECTION 4: Sleep Support Options (Talk to Your Doctor)
| Drink 30–60 minutes before sleep | Type | Notes |
|---|---|---|
| Trazodone | Prescription sleep aid | Non-addictive, commonly used |
| Hydroxyzine | Anti-anxiety/antihistamine | Helps with sleep & cravings |
| Melatonin (1–3 mg) | Natural hormone | Best 1–2 hrs before bed |
| Magnesium glycinate | Supplement | Calms nervous system |
| Chamomile, valerian tea | Herbal remedy | Drink 30–60 min before sleep |
📓 SECTION 5: Weekly Reflection & Goal Setting
How was your sleep this week?
✍️ ___________________________________________________
What helped improve your sleep?
✍️ ___________________________________________________
What made it harder to sleep?
✍️ ___________________________________________________
One sleep goal for next week:
🟩 ___________________________________________________
🌱 SECTION 6: Support & Safety Plan
If I Can’t Sleep & Feel Anxious or Triggered:
- Do a breathing or grounding technique
- Read a calm book or listen to music
- Text/call a peer or sponsor
- Attend a late-night recovery meeting (online)
- Remind myself: “Sleep will return—this is part of healing.”
Question: Provide a family sleep support guide.
Answer: A printable-friendly Family Sleep Support Guide to help families support a loved one experiencing insomnia during detoxification. It includes simple actions, reminders, and routines that promote rest, reduce anxiety, and protect recovery progress.
💞 Family Sleep Support Guide
Helping Your Loved One Manage Insomnia During Detoxification
🧠 Why Sleep Matters in Detox
During opioid detox, the brain struggles to regulate sleep due to withdrawal-related changes in stress hormones, dopamine, and circadian rhythms. Insomnia is common and temporary, but it can increase cravings and relapse risk if not addressed with compassion and structure.
🛏️ 1. Create a Sleep-Friendly Home Environment
✔️ Reduce noise, especially in the evening
✔️ Keep lighting soft and dim after sunset
✔️ Avoid arguing, loud TV, or phone calls near bedtime
✔️ Use blackout curtains, a white noise machine, or a fan
📝 “We keep the home quiet after ___ PM to support their sleep routine.”
🧘 2. Support Calming Bedtime Routines
✔️ Encourage relaxing habits like:
- Reading
- Listening to soft music
- Journaling
- Deep breathing
✔️ Avoid screens at least 1 hour before bed
✔️ Offer to wind down together (no-pressure connection)
📝 “Each night we encourage them to try at least one calming activity before bed.”
💬 3. Offer Gentle Emotional Support
- ✅ Validate their struggle: “I know this is frustrating. You’re doing great.”
- ✅ Avoid pressure: Don’t say “Just go to sleep” or “You’ll be fine.”
- ✅ Reassure: “Your sleep will return—it’s part of healing.”
📝 Use kind words that reduce shame and anxiety.
⏰ 4. Promote Consistent Routines
✔️ Wake-up time: ______________ AM
✔️ Bedtime goal: ______________ PM
✔️ Morning sunlight or short walk
✔️ Limit naps to <30 minutes or avoid completely
📝 “We try to keep consistent wake/sleep times, even after a rough night.”
⚠️ 5. Avoid Enabling or Destructive Habits
🚫 Don’t suggest alcohol, marijuana, or old sleeping pills
🚫 Don’t let them isolate all day—invite them to connect
🚫 Don’t take it personally if they’re irritable
📝 “We support recovery habits over short-term sleep fixes.”
📚 6. Stay Informed & Connected
✔️ Attend a family support group (Al-Anon, SMART Recovery Family & Friends)
✔️ Talk to a counselor about family sleep challenges
✔️ Learn about addiction, withdrawal, and sleep together
📝 “We remind ourselves this is part of recovery, not a failure.”
🌱 7. Support Your Own Well-being
- Get your own rest and quiet time
- Take breaks when needed
- Talk to others who understand
- Practice your own relaxation (walk, music, faith, journaling)
💡 “You can’t pour from an empty cup. Your calm presence matters.”
🧭 Family Nighttime Plan (Optional Fill-in)
| Time | Family Routine | Who’s Involved? |
|---|---|---|
| 7:00 PM | Dim lights, quiet activities | Whole family |
| 8:00 PM | No screens / calming activity | Support person + them |
| 9:00 PM | Gentle check-in + winding down | Partner/Sibling |
| 10:00 PM | Sleep environment set up | Everyone |
💬 Encouraging Words to Say:
“Bad nights happen, but you’re still moving forward.”
“You don’t have to do this alone.”
“We’re proud of you for getting through today.”
“Sleep is hard right now, but your body is working to heal.”
Question: Provide a community sleep support planner for detox.
Answer: The Community Sleep Support Planner is designed for individuals going through detoxification and recovery who are struggling with insomnia. This tool helps organize and track community-based strategies that support healthy sleep, structure, and emotional regulation.
Let me know if you’d like this in a fillable or printable PDF with calming visuals and icons.
💤 Community Sleep Support Planner
Stabilize your sleep through structure, support, and healing routines
🌤️ SECTION 1: My Sleep Challenges
Which sleep problems do you currently experience?
☐ Trouble falling asleep
☐ Waking up during the night
☐ Vivid dreams or nightmares
☐ Early waking
☐ Sleep anxiety
☐ Cravings at night
☐ Fatigue during the day
How long have these issues been going on?
📝 __________________________________________________
What time do you usually:
- Go to bed? ______
- Wake up? ______
- Feel most tired? ______
🛏️ SECTION 2: My Community-Based Sleep Resources
🔄 1. Recovery Programs
| Program Name | Type (NA, SMART, etc.) | Time | Sleep Benefit | Joined? (Y/N) |
|---|---|---|---|---|
🧘 2. Wellness & Mindfulness Activities
| Activity / Class | Where/When | Type (Yoga, Meditation, etc.) | Tried Before? (Y/N) | Plan to Join? |
|---|---|---|---|---|
🏠 3. Sober Living / Structured Housing (if needed)
| Housing Program | Daily Routines Offered | Evening Quiet Hours? | Helps With Sleep? |
|---|---|---|---|
📱 4. Nighttime Support (Peer or Crisis Lines)
| Resource Name | Contact Info | When to Use |
|---|---|---|
| SAMHSA Helpline | 1-800-662-HELP | Any time during detox |
| Crisis Text Line | Text HOME to 741741 | When anxious or alone |
| Local Warm Line |
📚 5. Quiet, Structured Daytime Options
| Resource or Location | Hours | Type (Library, Center, Volunteer, etc.) | Helps Sleep? |
|---|---|---|---|
📅 SECTION 3: Weekly Sleep Support Schedule
| Day | Community Resource | Time | Purpose (Routine, Relaxation, Peer Support) |
|---|---|---|---|
| Monday | |||
| Tuesday | |||
| Wednesday | |||
| Thursday | |||
| Friday | |||
| Saturday | |||
| Sunday |
💬 SECTION 4: Sleep Reflection & Progress Notes
1. What community resource helped you sleep the most this week?
📝 _________________________________________________________
2. What made it harder to sleep, and how did you respond?
📝 _________________________________________________________
3. One small sleep-supporting action to try next week:
🟩 _________________________________________________________
“Even when sleep is hard, I am healing. I am not alone. I have support.”
Conclusion
Sleep disturbances during detoxification arise from complex changes in brain pathways that regulate key neurotransmitters, making restful sleep difficult. Addressing these challenges through self-management techniques, strong family support, and access to community resources is essential for improving sleep quality and supporting long-term recovery. By combining biological understanding with social and emotional support, individuals undergoing detox can better navigate sleep issues and reduce the risk of relapse.
Video: How Sleep Affects Opioid Detoxification