Dopamine plays a central role in addiction by shaping motivation, reward, and learning within the brain. Rather than simply producing pleasure, dopamine teaches the brain what to seek and repeat. In addition, substances and compulsive behaviors overstimulate this system, causing the brain to prioritize short-term rewards over long-term well-being. Over time, this leads to cravings, tolerance, emotional blunting, and loss of control. Understanding dopamine helps reframe addiction as a brain-based condition and highlights why recovery requires more than willpower—it requires restoring balance to the reward system through intentional, sustained support.
The Science of Dopamine in Addiction: How the Brain’s Reward System Gets Hijacked
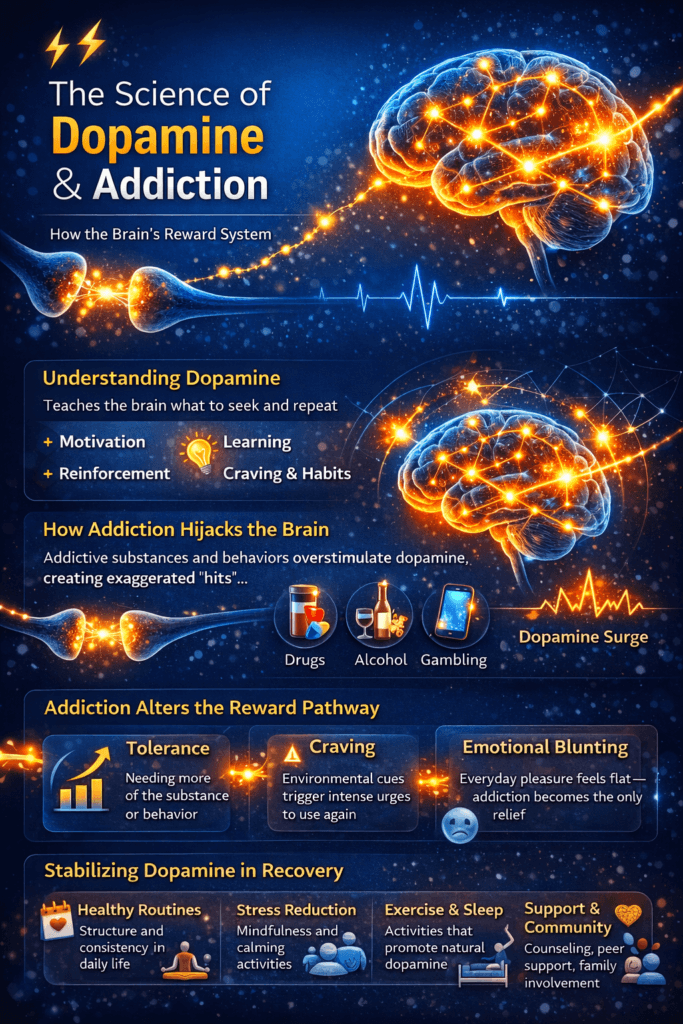
Dopamine is often misunderstood as the brain’s “pleasure chemical,” but its real role in addiction is far more complex—and far more powerful. Dopamine is a neurotransmitter involved in motivation, learning, and reinforcement. Rather than simply making us feel good, dopamine teaches the brain what is worth repeating. It marks experiences as important and drives us to seek them again.
Under normal conditions, dopamine is released during survival-promoting activities such as eating, social bonding, achieving goals, or learning something new. This release strengthens neural pathways, helping the brain remember behaviors that support well-being. In this way, dopamine acts as a teacher, reinforcing habits that keep us alive and connected.
Addictive substances and behaviors disrupt this system. Drugs like opioids, stimulants, alcohol, and even behaviors such as gambling or excessive digital use can trigger dopamine releases far beyond natural levels. These exaggerated surges signal to the brain that the substance or behavior is extremely valuable—more valuable than food, relationships, or long-term goals. Over time, the brain prioritizes seeking the addictive stimulus above almost everything else.
With repeated exposure, the brain adapts. Dopamine receptors become less sensitive, meaning the person needs more of the substance or behavior to achieve the same effect. This process, known as tolerance, is why addiction escalates. At the same time, baseline dopamine levels can drop, leaving individuals feeling flat, unmotivated, or depressed when not using. Everyday pleasures lose their impact, reinforcing reliance on the addictive behavior just to feel “normal.”
Dopamine also plays a key role in craving and relapse. Environmental cues—such as places, people, emotions, or stress—can trigger dopamine release even before the substance is used. This anticipatory dopamine spike drives intense cravings, often long after physical withdrawal has ended. This explains why relapse is not a failure of willpower, but a learned brain response.
Understanding the science of dopamine reframes addiction as a brain-based condition rather than a moral weakness. Recovery involves more than stopping use; it requires retraining the brain’s reward system. Over time, healthy activities such as exercise, therapy, meaningful relationships, purpose-driven goals, and, when appropriate, medication can help restore dopamine balance. With consistency and support, the brain can heal—and motivation, joy, and resilience can return.
Self-Management Strategies to Regulate Dopamine in Addiction Recovery
Regulating dopamine is a central part of addiction recovery. After prolonged substance use or compulsive behaviors, the brain’s reward system becomes dysregulated—swinging between intense cravings and emotional flatness. Self-management strategies help stabilize dopamine signaling over time, allowing the brain to relearn to balance motivation and pleasure without relying on addictive stimuli.
One of the most effective ways to regulate dopamine naturally is through a structured routine. Consistent daily schedules for waking, eating, working, exercising, and sleeping provide predictable rewards to the brain. Dopamine thrives on anticipation and completion of tasks, so even small, achievable goals—such as making the bed or taking a short walk—help rebuild healthy reward pathways and restore motivation.
Physical activity plays a powerful role in dopamine regulation. Regular exercise increases dopamine receptor availability and supports overall neurotransmitter balance. Moderate, consistent movement—like walking, strength training, yoga, or cycling—is more effective than extreme workouts. Over time, exercise helps reduce cravings, improves mood, and restores the brain’s ability to experience reward from non-drug sources.
Mindfulness and stress-management practices are equally important. Chronic stress drives dopamine dysregulation and increases relapse risk. Techniques such as deep breathing, meditation, grounding exercises, and progressive muscle relaxation calm the nervous system and reduce impulsive dopamine-seeking behaviors. Mindfulness also strengthens awareness of cravings, allowing individuals to respond thoughtfully rather than react automatically.
Sleep is a foundational but often overlooked regulator of dopamine. Poor sleep disrupts dopamine signaling, worsens impulse control, and amplifies emotional distress. Establishing healthy sleep hygiene—consistent bedtimes, limiting screen exposure at night, and avoiding stimulants late in the day—helps normalize dopamine rhythms and supports emotional resilience.
Nutrition also influences dopamine balance. Diets rich in protein, whole grains, fruits, vegetables, and healthy fats provide the building blocks for neurotransmitter production. Staying hydrated and avoiding excessive sugar and ultra-processed foods prevents rapid dopamine spikes and crashes that can mimic addictive patterns.
Finally, reducing artificial dopamine triggers is key. Limiting exposure to substances, excessive social media, gambling, or other high-stimulation behaviors gives the brain space to recalibrate. Replacing these with meaningful activities—connection, creativity, learning, service, and purpose-driven goals—gradually retrains the reward system.
Self-management does not “fix” dopamine overnight, but consistency matters more than intensity. With time, patience, and supportive habits, the brain can regain balance. Regulated dopamine leads to clearer thinking, improved mood, stronger self-control, and a recovery that feels sustainable rather than forced.
Family Support Strategies to Regulate Dopamine in Addiction Recovery
Family plays a powerful role in regulating dopamine during addiction recovery. Because addiction reshapes the brain’s reward system, the environment surrounding a person in recovery can either stabilize or destabilize dopamine signaling. Supportive family strategies help reduce stress, reinforce healthy rewards, and create consistency that allows the brain to heal.
One of the most important family strategies is creating a predictable, low-chaos environment. Consistent routines around meals, sleep, work, and family time provide structure that supports dopamine regulation. When expectations are clear and daily rhythms are stable, the brain experiences fewer stress-driven dopamine spikes that can trigger cravings or impulsive behavior.
Healthy communication is another key factor. Families that use calm, nonjudgmental language help reduce shame and emotional volatility—both of which disrupt dopamine balance. Encouraging open conversations, active listening, and validation helps the individual feel safe and supported. Feeling understood and accepted activates natural reward pathways tied to connection and belonging, reducing the need for artificial dopamine sources.
Families can also support dopamine regulation by reinforcing progress rather than perfection. Small wins—such as attending appointments, practicing coping skills, or maintaining routines—should be acknowledged. Positive reinforcement strengthens healthy dopamine pathways and builds motivation. Criticism or constant monitoring, on the other hand, can increase stress and drive relapse-related behaviors.
Shared healthy activities are another powerful tool. Family walks, exercise, cooking meals together, hobbies, or creative projects provide natural dopamine through connection and a sense of accomplishment. These experiences help retrain the brain to associate reward with relationships and meaningful engagement rather than substances or compulsive behaviors.
Setting clear, consistent boundaries is equally important. Boundaries reduce chaos and protect both the family and the person in recovery from patterns that destabilize dopamine levels, such as enabling or emotional overinvolvement. Boundaries should be communicated calmly and consistently enforced, reinforcing accountability rather than punishment.
Finally, families benefit from caring for their own emotional health. Family stress, burnout, and unresolved conflict can unintentionally dysregulate dopamine in the household. Support groups, family therapy, education about addiction, and self-care help families remain grounded and emotionally regulated. A regulated family system supports a regulated brain.
When families focus on stability, encouragement, connection, and healthy boundaries, they become a powerful source of healing. Over time, these supportive environments help normalize dopamine signaling, reduce the risk of relapse, and foster long-term recovery grounded in trust, resilience, and shared growth.
Community Resource Strategies to Regulate Dopamine in Addiction Recovery
Community resources play a critical role in regulating dopamine during addiction recovery. Because addiction alters the brain’s reward and motivation systems, recovery is strengthened when individuals are surrounded by environments that promote stability, connection, and healthy reinforcement. Community-based supports help replace artificial dopamine spikes with consistent, meaningful sources of reward.
One of the most impactful community strategies is access to peer support groups. Mutual-support meetings, recovery communities, and peer-led programs provide connection, shared understanding, and accountability. Social belonging naturally stimulates dopamine in a balanced way, reinforcing motivation without the extremes seen in addictive behaviors. Seeing others’ progress in recovery also activates hope and goal-oriented dopamine pathways.
Structured community programs further support dopamine regulation. Outpatient treatment, recovery coaching, vocational training, and educational programs provide routine, purpose, and achievable milestones. These predictable achievements retrain the brain to associate dopamine release with effort, growth, and completion rather than instant gratification. Consistency within these programs reduces stress-driven dopamine dysregulation and relapse risk.
Physical and recreational community resources are equally important. Access to gyms, walking groups, sports leagues, yoga classes, art workshops, or volunteer opportunities offers healthy stimulation and social engagement. These activities promote gradual dopamine release through movement, creativity, and contribution—key components in restoring reward sensitivity.
Community-based mental health and medical services also help stabilize dopamine. Counseling, medication-assisted treatment, and integrated primary care address co-occurring conditions such as depression, anxiety, or chronic pain that can disrupt dopamine balance. When these underlying issues are treated, cravings and impulsive dopamine-seeking behaviors often decrease.
Faith-based organizations, service groups, and volunteer networks can offer additional layers of meaning and connection. Purpose-driven activities activate dopamine through service and identity rather than consumption. Feeling valued and useful within a community strengthens intrinsic motivation and emotional regulation.
Finally, recovery-friendly communities that reduce stigma play a powerful role. Safe housing programs, recovery-friendly workplaces, sober living environments, and community education initiatives lower chronic stress and shame—two major disruptors of dopamine balance. When individuals feel accepted rather than judged, the brain is better able to heal.
Community resources do more than support abstinence; they help retrain the brain’s reward system. Through connection, structure, purpose, and access to care, communities provide steady, sustainable dopamine regulation—laying the foundation for long-term recovery, resilience, and a meaningful life beyond addiction.
Frequently Asked Questions
Here are some common questions:
1. What is dopamine, and why is it important in addiction?
Dopamine is a neurotransmitter involved in motivation, learning, reward, and habit formation. In addition, dopamine becomes dysregulated because substances or compulsive behaviors produce unnaturally strong dopamine signals, teaching the brain to prioritize those behaviors over healthy, long-term goals.
2. Is dopamine the same as pleasure?
No. Dopamine is not the brain’s pleasure chemical—it is the motivation and learning chemical. It signals what is important and worth repeating. Pleasure involves other neurotransmitters, while dopamine drives craving, anticipation, and reinforcement.
3. How do drugs affect dopamine differently than natural rewards?
Natural rewards such as food, connection, or achievement elicit moderate, regulated dopamine release. Drugs and addictive behaviors cause rapid, intense dopamine spikes that overwhelm the system, making the brain falsely label them as extremely valuable.
4. Why do people with addiction lose interest in normal activities?
Repeated dopamine overstimulation reduces receptor sensitivity and lowers baseline dopamine levels. As a result, everyday pleasures feel dull or unrewarding, pushing individuals to rely on the addictive substance or behavior just to feel normal.
5. What role does dopamine play in cravings and relapse?
Dopamine is heavily involved in craving. Environmental cues—stress, places, people, emotions—can trigger dopamine release before use occurs, driving powerful urges even after long periods of abstinence.
6. Can dopamine levels return to normal after addiction?
Yes. The brain can heal, but it takes time. With sustained recovery, healthy routines, reduced stimulation, therapy, and support, dopamine signaling and receptor sensitivity can gradually improve.
7. Does willpower control dopamine-driven behavior?
Not entirely. Dopamine-driven cravings are learned brain responses, not moral failures. While effort matters, recovery is most effective when it includes structure, support, and strategies that retrain the brain’s reward system.
8. How do medications help regulate dopamine in addiction?
Some medications stabilize brain chemistry, reduce cravings, or block dopamine surges from substances. These treatments help protect recovery while the brain gradually rebalances its reward pathways.
9. Can behavioral addictions affect dopamine the same way drugs do?
Yes. Gambling, gaming, social media, and other high-stimulation behaviors can strongly activate dopamine pathways, leading to similar craving, tolerance, and compulsive patterns seen in substance addiction.
10. Why is understanding dopamine important for recovery?
Understanding dopamine reduces stigma and shame. It helps people recognize addiction as a brain-based condition and highlights why recovery requires patience, consistency, and supportive environments—not just stopping use.
Conclusion
Regulating dopamine in addiction recovery is a gradual process that works best when self-management, family support, and community resources function together. Healthy routines, exercise, stress management, sleep, and nutrition help individuals rebuild internal dopamine balance. Supportive families create stability, reduce stress, reinforce progress, and foster connection—key drivers of natural reward. Community resources provide structure, purpose, a sense of belonging, and access to care, replacing artificial dopamine spikes with meaningful engagement. When these layers align, the brain’s reward system can heal, cravings diminish, and recovery becomes not only possible, but sustainable and life-giving.
Video: