Primary care physicians (PCPs) are increasingly involved in prescribing addiction treatment, offering greater accessibility and continuity of care while integrating addiction management into general health services. Despite these advantages, challenges such as limited specialized training, time constraints, and the potential for inadequate treatment exist. Ethical dilemmas, including competence issues, patient autonomy, confidentiality, and resource allocation, further complicate the landscape. Community resource strategies such as collaborative care models, robust referral networks, and patient navigation services are crucial for addressing these complexities. These strategies enhance PCPs’ effectiveness in delivering comprehensive addiction treatment by leveraging community support and healthcare resources.
The Essential Role of Primary Care Physicians in Addiction Medicine
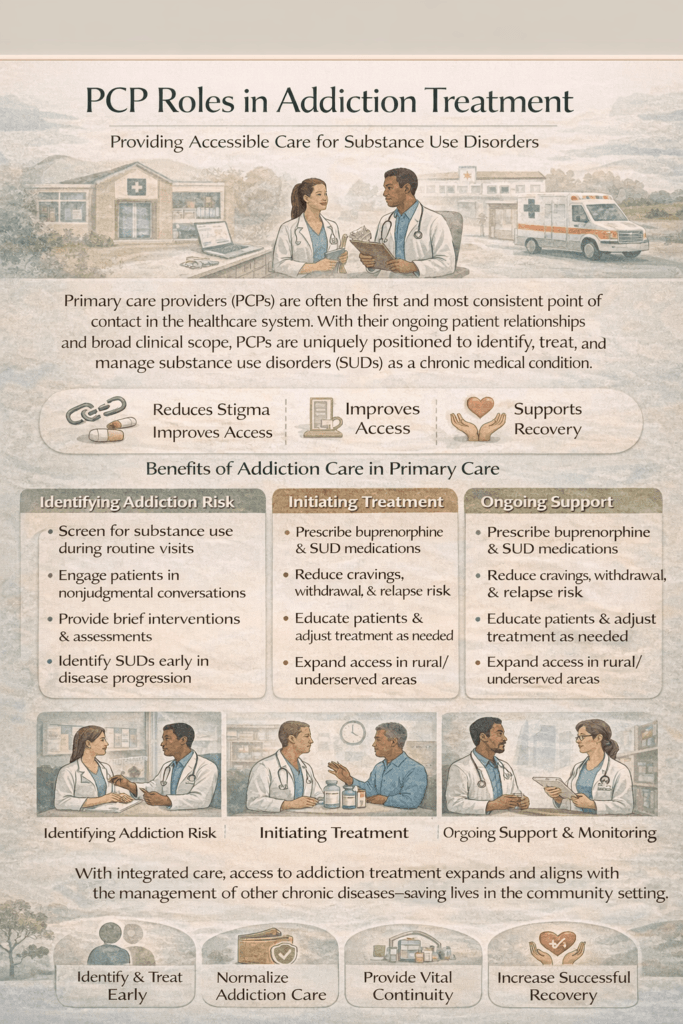
Primary care physicians (PCPs) play a pivotal role in the management and treatment of addiction. Their involvement is crucial for several reasons:
1. Accessibility
- Role: PCPs are often the first healthcare professionals individuals encounter when seeking medical care.
- Impact: Their widespread availability allows them to identify and address addiction issues early, making them a critical touchpoint in the continuum of care.
2. Continuity of Care
- Role: PCPs maintain long-term relationships with their patients, providing consistent care over time.
- Impact: This ongoing relationship enables PCPs to monitor progress, adjust treatment plans as necessary, and offer sustained support.
3. Holistic Approach
- Role: PCPs address various health needs, including mental, physical, and social aspects of their patients’ lives.
- Impact: Managing addiction requires a comprehensive approach that considers all facets of a person’s health, and PCPs are uniquely positioned to provide this integrated care.
4. Integration with General Health Care
- Role: Incorporating addiction treatment into general health care settings helps normalize addiction treatment.
- Impact: This approach reduces stigma, encourages more individuals to seek help, and facilitates the management of co-occurring conditions, which are common among those with addiction.
5. Training and Certification
- Role: Many PCPs receive specialized training in addiction medicine and can become certified to prescribe medications such as buprenorphine for opioid use disorder.
- Impact: This training expands the availability of effective treatment options and enhances the healthcare system’s capacity to address addiction.
6. Resource Constraints
- Role: There is a notable shortage of specialized addiction treatment providers.
- Impact: By allowing PCPs to prescribe addiction treatment, the healthcare system can better bridge the gap and increase the overall capacity to treat addiction.
7. Early Intervention
- Role: PCPs are well-positioned to identify risky substance use behaviors and intervene before addiction becomes severe.
- Impact: Early intervention can prevent the escalation of addiction, reducing the risk of more serious health issues and complications.
8. Comprehensive Care Plans
- Role: PCPs can develop and implement comprehensive care plans that include medication-assisted treatment (MAT), counseling, and other support services.
- Impact: A well-rounded approach to addiction management improves treatment outcomes and supports long-term recovery.
By utilizing the unique position of PCPs within the healthcare system, we can more effectively address the widespread issue of addiction. PCPs play a crucial role in improving access to addiction treatment, managing co-occurring health conditions, and providing continuous support, ultimately enhancing outcomes for individuals and their communities.
Disadvantages of Primary Care Physicians Prescribing Addiction Treatment
While primary care physicians (PCPs) can significantly impact addiction treatment, several challenges and disadvantages need to be addressed:
1. Limited Specialized Training
- Challenge: Many PCPs may not have extensive training in addiction medicine.
- Impact: This gap in specialized knowledge can affect the quality of care provided, as addiction treatment often requires expertise beyond general medical education.
2. Time Constraints
- Challenge: PCPs typically have limited time for each patient visit.
- Impact: The complexity and time-consuming nature of addiction treatment may be challenging to manage within the constraints of a standard primary care appointment.
3. Resource Limitations
- Challenge: PCPs may lack access to necessary resources, such as addiction specialists, behavioral health services, and community support.
- Impact: Limited resources can hinder the effectiveness of addiction treatment and support, affecting patient outcomes.
4. Stigma and Bias
- Challenge: PCPs, like other healthcare providers, may have stigmatizing attitudes or biases towards individuals with addiction.
- Impact: Such biases can impact the quality of care and may deter patients from seeking or continuing treatment.
5. Monitoring and Follow-Up
- Challenge: Effective addiction treatment requires regular monitoring and follow-up.
- Impact: PCPs may struggle to provide the necessary oversight in a busy primary care setting, potentially affecting treatment continuity and effectiveness.
6. Complex Cases
- Challenge: Patients with severe or complex addiction issues may need specialized care beyond what PCPs can offer.
- Impact: These cases may require the expertise of addiction specialists to be managed effectively.
7. Risk of Inadequate Treatment
- Challenge: PCPs might under-treat or over-treat addiction, especially if they are not well-versed in the latest guidelines and practices.
- Impact: Inadequate or inappropriate treatment can lead to suboptimal outcomes and affect patient recovery.
8. Coordination of Care
- Challenge: Addiction treatment often involves coordination with mental health professionals, social workers, and other specialists.
- Impact: PCPs may struggle to coordinate, leading to fragmented care and reduced treatment effectiveness.
9. Legal and Regulatory Barriers
- Challenge: Legal and regulatory issues can complicate the prescribing of specific addiction treatments, such as medication-assisted treatment (MAT) for opioid use disorder.
- Impact: These barriers can limit the ability of PCPs to provide comprehensive addiction treatment.
10. Burnout
- Challenge: Managing addiction treatment can be emotionally and professionally demanding.
- Impact: PCPs, already facing high levels of stress and burnout, may find the additional responsibilities of addiction treatment exacerbating their stress levels.
Addressing these disadvantages involves a multifaceted approach, including enhanced training for PCPs, better integration of addiction services within primary care, and improved support systems. By tackling these challenges, we can optimize the role of PCPs in addiction treatment and improve outcomes for individuals with substance use disorders.
Ethical Dilemmas in Primary Care Physicians’ Prescribing Addiction Treatment
Primary care physicians (PCPs) face several ethical dilemmas when prescribing addiction treatment. Addressing these dilemmas requires careful consideration to ensure ethical and practical patient care:
1. Competence and Training
- Dilemma: Ensuring PCPs have the necessary training and competence to provide effective addiction treatment.
- Ethical Concern: There is a moral obligation to provide high-quality care. Insufficient training may result in suboptimal treatment outcomes, potentially harming patients who rely on their PCPs for addiction management.
2. Patient Autonomy and Informed Consent
- Dilemma: Balancing the need for appropriate addiction treatment while respecting patient autonomy and ensuring informed consent.
- Ethical Concern: To make autonomous decisions, patients must be informed about their treatment options, including risks and benefits. Ensuring that patients understand their treatment plans, especially in the context of addiction, can be challenging.
3. Confidentiality and Stigma
- Dilemma: Maintaining patient confidentiality while minimizing stigma and discrimination.
- Ethical Concern: Addiction is highly stigmatized, and breaches of confidentiality can lead to significant personal and social repercussions for patients. PCPs must ensure that patient information is kept confidential while coordinating care.
4. Resource Allocation and Access to Care
- Dilemma: Ensuring fair and equitable access to addiction treatment, particularly in resource-limited settings.
- Ethical Concern: Due to limited resources, PCPs may face challenges in providing equitable care, raising moral concerns about justice and fairness in access to treatment.
5. Conflict of Interest
- Dilemma: Managing potential conflicts of interest, such as relationships with pharmaceutical companies.
- Ethical Concern: PCPs may face ethical dilemmas if they are influenced by pharmaceutical companies’ prescribing practices, which could potentially compromise patient care.
6. Patient-Provider Relationship
- Dilemma: Navigating the complexities of the patient-provider relationship when treating addiction.
- Ethical Concern: Addiction treatment can strain the patient-provider relationship, particularly with trust issues or non-adherence to treatment plans. PCPs must balance empathy and support with the need to set boundaries and manage expectations.
7. Dual Loyalty
- Dilemma: Balancing responsibilities to the patient with broader public health concerns.
- Ethical Concern: PCPs may encounter situations where individual patient needs conflict with public health goals, such as controlling the spread of infectious diseases associated with drug use.
8. Scope of Practice
- Dilemma: Determining the appropriate scope of practice for PCPs in addiction treatment.
- Ethical Concern: PCPs must recognize the limits of their expertise and know when to refer patients to specialists to ensure they receive the best possible care.
9. Non-Maleficence and Beneficence
- Dilemma: Ensuring that treatment decisions do not cause harm and are in the patient’s best interest.
- Ethical Concern: Balancing the potential benefits of addiction treatment with the risks of side effects, withdrawal, or other adverse outcomes requires careful consideration.
10. Social and Economic Determinants of Health
- Dilemma: Addressing the broader social and economic factors contributing to addiction.
- Ethical Concern: PCPs must consider how social determinants of health, such as poverty, lack of housing, and unemployment, impact addiction and treatment outcomes. Addressing these factors ethically requires a holistic approach.
Navigating these ethical dilemmas involves ongoing education, reflection, and adherence to moral principles in medical practice. Collaboration with addiction specialists, mental health professionals, and ethical committees can help PCPs manage these challenges effectively, ensuring the provision of high-quality and equitable addiction treatment.
Community Resource Strategies to Support PCPs in Addiction Treatment
Community resource strategies are crucial for enhancing the effectiveness and reach of addiction treatment prescribed by primary care physicians (PCPs). These strategies focus on integrating local resources, services, and support systems to provide comprehensive care for individuals with substance use disorders. Here are some key strategies:
1. Collaborative Care Models
- Strategy: Implement integrated care models that involve collaboration between PCPs, addiction specialists, mental health professionals, and social workers.
- Benefit: Ensures comprehensive care by addressing addiction’s medical and psychosocial aspects, leading to more effective treatment outcomes.
2. Referral Networks
- Strategy: Develop and maintain strong referral networks with local addiction treatment centers, behavioral health clinics, and support groups.
- Benefit: It provides patients with access to specialized care and additional support services when needed, facilitating a smoother treatment process.
3. Telemedicine Services
- Strategy: Utilize telemedicine to connect patients with addiction specialists and support services, especially in underserved or rural areas.
- Benefit: Increases access to care, allows regular follow-up, and provides ongoing monitoring without frequent in-person visits.
4. Community Outreach and Education
- Strategy: Conduct community outreach programs to raise awareness about addiction, reduce stigma, and educate the public about available treatment options.
- Benefit: Encourages individuals to seek help early and supports community engagement in addressing addiction issues.
5. Patient Navigation Services
- Strategy: Employ patient navigators or case managers to assist patients in accessing treatment, navigating the healthcare system, and connecting with community resources.
- Benefit: Helps patients overcome barriers to care and ensures they receive comprehensive support throughout their treatment journey.
6. Support Groups and Peer Support
- Strategy: Promote and facilitate access to peer support groups, such as Alcoholics Anonymous (AA), Narcotics Anonymous (NA), and other community-based support networks.
- Benefit: Provides ongoing emotional and social support, crucial for maintaining recovery and preventing relapse.
7. Education and Training for PCPs
- Strategy: Offer continuing education and training programs for PCPs on addiction treatment, including medication-assisted treatment (MAT) and behavioral therapies.
- Benefit: Enhances PCPs’ skills and confidence in managing addiction treatment, thereby improving the quality of patient care.
8. Partnerships with Law Enforcement and Social Services
- Strategy: Establish partnerships with local law enforcement, social services, and public health agencies to create a coordinated response to addiction.
- Benefit: Provides a holistic approach to addressing addiction, including prevention, treatment, and recovery support, integrating multiple community sectors.
9. Funding and Grants
- Strategy: Secure funding and grants to support addiction treatment programs, community outreach, and resource development.
- Benefit: Ensures the sustainability and expansion of addiction treatment services, improving access and quality of care.
10. Data Sharing and Monitoring
- Strategy: Develop systems for data sharing and monitoring patient outcomes across different providers and agencies.
- Benefit: Improves care coordination, tracks treatment effectiveness, and identifies areas for improvement in addiction treatment services.
11. Holistic and Culturally Sensitive Approaches
- Strategy: Implement holistic and culturally sensitive treatment approaches that consider patients’ unique needs and backgrounds.
- Benefit: Enhances patient engagement and treatment adherence by providing personalized, respectful care.
12. Community-Based Recovery Programs
- Strategy: Support community-based recovery programs that offer vocational training, housing assistance, and other services to support long-term recovery.
- Benefit: Addresses broader social determinants of health that impact addiction and recovery, promoting sustained recovery and reintegration into society.
By leveraging these community resource strategies, PCPs can offer more effective and comprehensive addiction treatment, improve patient outcomes, and foster a supportive environment for recovery.
Frequently Asked Questions
Here are some common questions:
Why are primary care providers important in addiction treatment?
Primary care providers are often the first point of contact for patients with substance use disorders and provide ongoing, trusted relationships that support early identification, treatment initiation, and long-term follow-up.
Can PCPs treat addiction effectively without specialty referral?
Yes. PCPs can safely and effectively manage many substance use disorders, especially opioid and alcohol use disorders, using evidence-based medications and integrated care models.
What addiction medications can PCPs prescribe?
PCPs can prescribe buprenorphine for opioid use disorder and medications for alcohol use disorder, such as naltrexone, acamprosate, and disulfiram, depending on patient needs and training.
How does addiction treatment fit into routine primary care visits?
Addiction care can be integrated through screening, brief interventions, medication management, chronic disease monitoring, and coordination with behavioral health and community resources.
Do PCPs need special training to treat addiction?
While additional training improves confidence and quality of care, many addiction treatments fall within the standard primary care scope. Ongoing education and clinical support enhance implementation.
How does primary care reduce stigma in addiction treatment?
Treating addiction alongside diabetes, hypertension, and depression normalizes substance use disorder as a medical condition and reduces shame associated with seeking care.
What role do PCPs play during high-risk transitions of care?
PCPs help prevent relapse and overdose by initiating medications, ensuring follow-up after hospital discharge or incarceration, and maintaining continuity of care.
Can PCPs manage co-occurring conditions in patients with addiction?
Yes. PCPs are well-positioned to address chronic pain, mental health disorders, infectious diseases, and other medical conditions commonly associated with substance use disorder.
What barriers prevent PCPs from providing addiction care?
Common barriers include limited time, lack of training, regulatory complexity, reimbursement challenges, and insufficient behavioral health integration.
How can healthcare systems support PCPs in addiction treatment?
Support includes expanding training, simplifying regulations, embedding behavioral health, improving reimbursement, and integrating addiction treatment into routine primary care workflows.
Conclusion
The involvement of primary care physicians in prescribing addiction treatment offers significant advantages, such as increased accessibility and continuity of care. Still, it also presents notable challenges, including limited specialized training and potential ethical dilemmas. Addressing these issues requires careful consideration of this approach’s disadvantages and moral concerns. Implementing community resource strategies, such as collaborative care models and robust referral networks, is essential to support PCPs in this role. By leveraging these strategies, the healthcare system can enhance the effectiveness of addiction treatment, providing comprehensive and integrated care that addresses the diverse needs of patients struggling with addiction.
Video: Your Doctor Can Actually Treat Addiction #AddictionTreatment #PrimaryCare