Panic disorder, marked by sudden, intense fear, can lead to addiction when individuals turn to substances like alcohol or benzodiazepines for quick relief. This self-medication increases the risk of dependency and complicates recovery. Preventing this requires self-management tools such as breathing techniques and journaling, supportive family environments, and access to community resources, including mental health services, school programs, and peer support. Together, these strategies build resilience and reduce the risk of addiction.
Breaking the Cycle: Understanding the Link Between Panic Disorder and Addiction
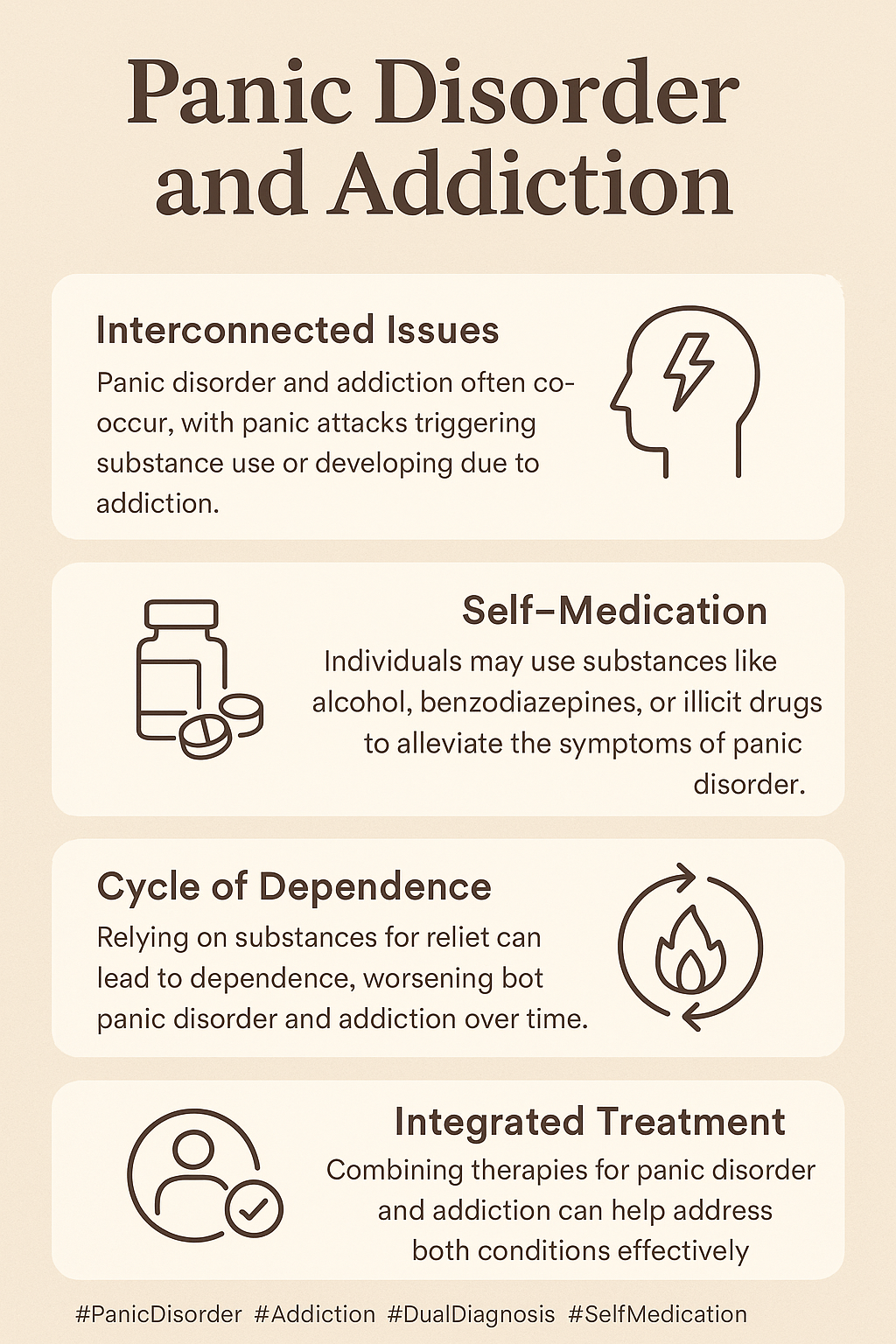
Panic disorder and addiction are often tangled in a complex, bidirectional relationship. While they may seem separate, they usually feed into one another through overlapping brain circuits, emotional responses, and environmental stressors. Here’s a clear breakdown of how these two conditions are connected — and what it takes to address both effectively.
🔄 1. The Self-Medication Cycle
When panic attacks become overwhelming, many individuals seek relief through substances like alcohol, benzodiazepines, or cannabis. While these may provide short-term calming effects, they can also set off a harmful cycle of dependence.
- Temporary relief quickly turns into psychological or physical dependence
- Tolerance builds, requiring larger doses to achieve the same calming effect
- Withdrawal symptoms can mimic or worsen panic, leading to further substance use
This cycle is often one of the earliest ways panic and addiction begin to reinforce each other.
🧠 2. Shared Neurological Pathways
The link between panic and addiction isn’t just behavioral — it’s rooted in brain biology. Both disorders involve dysregulation in:
- The amygdala, which processes fear and threat
- The prefrontal cortex, which governs judgment and impulse control
- Neurochemical systems, especially dopamine (reward) and GABA (calming)
Because these pathways are shared, people with panic disorder are often neurologically more susceptible to developing substance use disorders — and vice versa.
📊 3. Co-Occurrence and Risk Factors
Studies reveal a striking overlap: up to 20–40% of individuals with panic disorder also have a substance use disorder (SUD).
Key shared risk factors include:
- Genetics: A family history of either condition can increase vulnerability
- Trauma and adversity: Especially during childhood
- Chronic stress or untreated anxiety, which may trigger both disorders over time
🔁 4. The Reinforcement Loop
What starts as self-medication can spiral into a loop:
- Substance withdrawal increases anxiety sensitivity, making panic worse
- Panic episodes can heighten cravings, especially in high-stress or triggering environments
- Relapse risk increases when panic symptoms are not properly managed
This cycle makes it critical to treat both conditions together, rather than in isolation.
🧩 5. Treatment Challenges and Integrated Solutions
Some traditional panic treatments — like benzodiazepines — carry a high risk of dependence, making them a tricky option for someone with addiction risk.
Effective treatment requires:
- Integrated care, treating both disorders in tandem
- Cognitive Behavioral Therapy (CBT) that addresses both panic triggers and substance use patterns
- Non-addictive medications, such as SSRIs or beta-blockers
- Mindfulness, exercise, and lifestyle strategies to build healthier coping mechanisms
- Relapse prevention planning that factors in anxiety flare-ups
In summary, the connection between panic disorder and addiction is more than coincidental — it’s biological, emotional, and deeply intertwined. Without comprehensive treatment, one can easily worsen the other. But with early intervention, integrated care, and ongoing support, individuals can reclaim control and break the cycle.
💡 Tip: If you or someone you know is experiencing both panic and substance use concerns, seek out a provider who understands dual-diagnosis care — and remember, recovery is not only possible, it’s sustainable.
How to Prevent Panic Disorder from Leading to Addiction: 8 Proven Self-Management Strategies
Preventing panic disorder from progressing into an addiction disorder requires intentional strategies that foster resilience, reduce anxiety, and build healthier ways to cope. Many individuals experiencing panic attacks may turn to substances like alcohol or benzodiazepines for relief — but over time, this can lead to dependence or addiction. The good news? There are practical, evidence-based tools that help break this cycle before it starts.
🧘♀️ 1. Breathing and Grounding Techniques
Why it works: These techniques directly calm the nervous system and reduce the urgency that might drive someone to use substances for relief.
Examples:
- Box Breathing (inhale-hold-exhale-hold pattern)
- 5-4-3-2-1 Grounding using the five senses to reorient during anxiety
📓 2. Trigger Awareness and Journaling
Why it works: Becoming more aware of what sparks anxiety or cravings allows for earlier, more mindful intervention.
Tools:
- Log panic episodes (time, place, physical symptoms, thoughts)
- Track urges to use substances and what preceded them
🧠 3. Cognitive Restructuring
Why it works: Helps disrupt irrational thinking patterns that escalate panic and impulsive behavior.
Practice:
- Replace catastrophic thoughts (e.g., “I’m dying”) with reality-based affirmations (e.g., “This is anxiety. It will pass.”)
- Use calming mantras or logic-based reminders to ground yourself
💪 4. Healthy Coping Substitutes
Why it works: Non-addictive strategies provide similar emotional regulation benefits without harmful consequences.
Examples:
- Movement: gentle exercise, stretching, yoga
- Creative outlets: drawing, journaling, listening to calming music
- Physical grounding: cold water on the face (stimulates vagus nerve)
🗣 5. Social Connection and Support
Why it works: Isolation increases risk for both panic attacks and substance misuse. Emotional connection supports healing.
Suggestions:
- Join anxiety or recovery peer groups (in-person or virtual)
- Reach out to a trusted friend or support person to talk things through
📱 6. Digital Support Tools
Why it works: On-demand help from apps or hotlines offers real-time support during moments of distress.
Examples:
- Apps: MindShift, Insight Timer, QuitNow
- Hotlines: Crisis text lines or substance use helplines available 24/7
🛌 7. Prioritize Sleep, Nutrition, and Routine
Why it works: Sleep deprivation and poor nutrition heighten anxiety and reduce emotional regulation.
Tips:
- Stick to a consistent sleep schedule
- Limit caffeine and sugar intake
- Create calming routines (like stretching or herbal tea before bed)
📆 8. Set Micro-Goals
Why it works: Small, realistic goals promote self-efficacy and forward progress without overwhelming pressure.
Examples:
- “Today I’ll try a breathing exercise when I feel panic.”
- “This week I’ll attend one support group or therapy session.”
Panic disorder doesn’t have to lead to addiction — especially when armed with proactive, empowering tools. Building these skills gradually can strengthen your ability to manage anxiety, improve your emotional health, and reduce the need for external substances. The key is early awareness, consistent practice, and social support. Recovery is possible — and prevention is powerful.
How Family Support Can Prevent Panic Disorder from Leading to Addiction: 8 Essential Strategies
Family support is one of the most potent protective factors in preventing panic disorder from escalating into addiction. When families foster safety, emotional regulation, and open communication, they create a nurturing environment where anxiety can be managed without turning to substances. Here are eight key strategies families can use to support their loved ones effectively:
👂 1. Listen Without Judgment
Why it helps: Reduces shame and encourages openness, so your loved one feels safe sharing their anxiety without fear of dismissal.
What to do: Use validating statements like, “That sounds really overwhelming. I’m here with you.”
🛡 2. Create a Safe and Predictable Environment
Why it helps: Minimizes external stressors that trigger panic and reduces the risk of substance use.
Tips: Maintain consistent routines and limit exposure to conflict or overstimulation at home.
🧠 3. Learn About Panic and Addiction Together
Why it helps: Reduces stigma, increases empathy, and promotes collaborative problem-solving.
What to try: Attend psychoeducation workshops or watch short educational videos as a family.
🗣 4. Practice Calming Techniques as a Family
Why it helps: It models healthy coping and builds shared tools everyone can use in stressful moments.
Examples: Do a 5-minute breathing exercise together or take a walk after dinner as a family routine.
🔄 5. Monitor Without Controlling
Why it helps: Maintains trust while allowing early intervention if concerns arise.
Tips: Use gentle check-ins rather than interrogations, and watch for changes in sleep, mood, or social behavior.
🌱 6. Support Therapy and Non-Addictive Treatments
Why it helps: Ensures early professional help and reduces the temptation to self-medicate.
Action steps: Help find a trauma-informed or CBT therapist and support medication plans that avoid addictive substances.
🧩 7. Encourage Healthy Coping Activities
Why it helps: Builds emotional resilience and provides positive outlets for stress.
Ideas: Encourage creative activities such as art or music, and support participation in peer support or youth programs.
💬 8. Use a Supportive Conversation Framework
Why it helps: Keeps communication open and non-threatening, strengthening your relationship.
Sample script: “I’ve noticed you’ve seemed anxious lately. I want to make sure you know you can talk to me about anything—without judgment.”
In summary, families play a vital role in breaking the cycle that can turn panic disorder into addiction. By listening compassionately, creating safe environments, learning together, and supporting healthy coping, families can help their loved ones navigate anxiety without resorting to harmful substances. Open dialogue and early intervention are key — and with the proper support, recovery is possible.
Community Resource Strategies to Prevent Panic Disorder from Progressing to Addiction
Community resources are vital in preventing panic disorder from evolving into addiction by offering early support, reducing isolation, and encouraging healthy coping alternatives. When communities proactively create accessible and integrated services, individuals struggling with anxiety have better chances of recovery without turning to substances. Here are key strategies communities can adopt:
🧠 1. Integrated Mental Health and Substance Use Services
Why it matters: Early, accessible care can address panic symptoms before individuals resort to substance use.
Examples: Community mental health centers with dual-diagnosis programs; walk-in anxiety clinics; mobile crisis teams.
🧑🏫 2. School-Based Education and Support
Why it matters: Young people are especially vulnerable, and schools can identify and support early anxiety symptoms.
Examples: Counselors trained in trauma and panic disorders; peer-led groups or wellness clubs; mental health literacy workshops for students and families.
🤝 3. Peer Recovery and Support Groups
Why it matters: Connection and shared experience reduce the urge to self-medicate.
Examples: Local NAMI chapters; SMART Recovery or peer-led anxiety groups; recovery community centers offering anxiety-informed support.
📲 4. Digital and Helpline Services
Why it matters: Immediate support during panic episodes can prevent substance use as a coping mechanism.
Examples: Crisis Text Line (Text HOME to 741741); mental health apps promoted through libraries, schools, or clinics.
🧘 5. Affordable Wellness and Coping Resources
Why it matters: Providing accessible alternatives helps individuals healthily soothe anxiety.
Examples: Community yoga or mindfulness classes; art and music therapy programs; nature-based activities like walking groups or community gardens.
🧭 6. Awareness Campaigns and Trainings
Why it matters: Reducing stigma and increasing knowledge promote early intervention.
Examples: Mental health first aid training for parents, teachers, and community members; public events during Mental Health or Recovery Awareness months; flyers and posters in clinics and libraries highlighting links between panic and substance use.
In summary, communities that build robust, compassionate, and accessible resources can make a real difference in preventing the progression from panic disorder to addiction. Early intervention, education, peer support, and wellness programs together create a safety net that empowers individuals to manage anxiety effectively and avoid harmful coping strategies.
Frequently Asked Questions
Here are some common questions:
Question: Provide a self-management worksheet to prevent panic disorder from leading to addiction.
Answer: Self-Management Worksheet: Preventing Panic from Leading to Addiction
Name: _________________________
Date: _________________________
1. Today’s Emotional Check-In
☐ Calm ☐ Anxious ☐ Overwhelmed ☐ Triggered ☐ Other: ___________
2. What Triggered My Anxiety or Panic Today?
3. What Did I Do in Response? (Healthy or Unhealthy)
4. What Strategy Can I Use Instead?
☐ Breathing (Box or Diaphragmatic)
☐ Grounding Exercise (5-4-3-2-1)
☐ Talk to Someone I Trust
☐ Journaling
☐ Go for a Walk or Exercise
☐ Creative Activity (Music, Drawing, etc.)
☐ Use a Calming App (Name: _______________)
5. What Would Help Me Right Now?
6. Positive Thought or Affirmation for the Day
7. One Small Goal for Tomorrow:
Resources
Local school counselor or pediatrician
Partnership to End Addiction (https://drugfree.org)
Question: Provide a family conversation guide to prevent panic disorder from leading to addiction.
Answer: Family Conversation Guide: Preventing Panic-Driven Substance Use
Purpose: Help families create safe, open conversations that address panic symptoms and prevent unhealthy coping, like substance use.
🟢 Step 1: Set a Safe Tone
Say:
“I want to talk with you about how you’ve been feeling—not to fix you or control anything, just to support you.”
Tips:
- Choose a calm, private time (not during a conflict).
- Be mindful of body language—open posture, soft tone, eye contact.
🔍 Step 2: Ask About Their Experience
Say:
“When you feel overwhelmed or panicked, what’s that like for you?”
“What do you usually do when those feelings come up?”
Listen for:
- Descriptions of physical symptoms (racing heart, chest pain)
- Coping behaviors (avoidance, isolation, risky choices)
🧭 Step 3: Explore Coping Options Together
Say:
“It makes sense you’d want to feel better fast. Would you be open to trying some calming tools together—like breathing or grounding techniques?”
Offer choices:
- Breathing apps
- Creative outlets
- Talking to a therapist
🧱 Step 4: Address Substance Use Risks Gently
Say:
“Some people try using substances to calm their anxiety. I get why that might seem like it works. But it often makes things worse in the long run. Have you heard of that?”
Normalize without shame:
“It’s common to want relief quickly. There are safer ways we can try together.”
🛠 Step 5: Reaffirm Support
Say:
“You’re not alone. Panic doesn’t mean you’re weak. We can figure this out together—without needing to go down a dangerous path.”
Follow up:
- Help schedule a therapy appointment
- Practice tools together weekly
- Check in regularly with warmth and curiosity
🔁 Bonus Tips for Families
Celebrate progress, not perfection.
Revisit conversations over time—it’s not one-and-done.
Focus on feelings, not behaviors.
Question: Provide a community resource directory template to help organize or promote these supports locally for panic disorder, without leading to addiction.
Answer: Community Resource Directory: Support for Panic Disorder & Prevention of Addiction
🧠 Purpose:
To connect individuals with panic disorder and their families to local, accessible, and evidence-based resources that promote recovery, reduce isolation, and prevent substance misuse.
📝 Section 1: Emergency & Crisis Services
| Service Name | Description | Phone Number | Website/Address | Notes |
|---|---|---|---|---|
| Crisis Hotline | 24/7 support for panic attacks, suicidality | 988 or local line | www.988lifeline.org | Free and confidential |
| Mobile Crisis Unit | On-site mental health crisis support | [Local #] | [Address if relevant] | Available: [Days/Hours] |
| Urgent Care Mental Health | Walk-in panic disorder care | [Clinic Name] | [Clinic Address/Website] | Accepts uninsured/patients in crisis |
🧠 Section 2: Mental Health Services
| Provider/Clinic Name | Services Offered | Phone/Email | Website/Address | Sliding Scale? | Accepts Insurance? | Notes |
|---|---|---|---|---|---|---|
| [Therapist Group] | CBT, DBT, Exposure Therapy | [Contact Info] | [URL] | Yes/No | Yes/No | Specializes in anxiety |
| [Community Mental Health] | Counseling, psychiatry | Walk-in accepted |
🫂 Section 3: Peer & Support Groups
| Group Name | Type (Online/In-person) | Meeting Info | Contact | Notes |
|---|---|---|---|---|
| Panic Disorder Support Circle | In-person | Mondays 6-7PM @ [Location] | [Email/Phone] | Free, peer-led |
| Anxiety Anonymous | Online & In-Person | See website | [URL] | Modeled after 12-step recovery |
| NAMI Local Chapter | Peer Family Support | Monthly Zoom | www.nami.org/local | For loved ones & families |
🧰 Section 4: Holistic & Wellness Resources
| Program/Center Name | Services Offered | Cost | Address/Website | Notes |
|---|---|---|---|---|
| [Yoga Studio] | Trauma-informed yoga | $ / Sliding scale | Breathwork for anxiety | |
| [Mindfulness Center] | Meditation, grounding workshops | Free intro session | [Website] | Panic-specific sessions |
| [Nature Group] | Group walks, outdoor therapy | Free | [Park or Meetup Info] | Promotes social connection |
🏠 Section 5: Social Determinants of Health
| May need a referral letter | Name/Org | Description | Contact | Notes |
|---|---|---|---|---|
| Housing Assistance | [Local Housing Org] | Short-term support | Panic often worsens in housing instability | |
| Transportation Aid | [Transit or Ride Program] | For therapy/medical visits | Free with appointment | |
| Financial Help | [Relief Org] | Utilities, rent, food | May need referral letter |
🔁 Section 6: Addiction Prevention & Harm Reduction
| Resource Name | Service Type | Contact | Notes |
|---|---|---|---|
| Behavioral Health Navigator | Resource linkage & follow-up | [Phone/Email] | Helps prevent substance use from escalating |
| Harm Reduction Center | Fentanyl test strips, naloxone | [Address/Hotline] | Open to anxiety medication misuse cases |
| Education Workshops | Local health dept | “Safe Coping Skills” classes | Promotes alternatives to self-medication |
✅ Checklist for Community Organizers
Add QR code linking to digital directory
Regularly update the directory every 6 months
Include culturally and linguistically diverse resources
Distribute printed and digital copies in clinics, libraries, and faith centers
Host quarterly workshops or meetups to promote resource awareness
Conclusion
The link between panic disorder and addiction highlights the urgent need for early intervention and comprehensive support. By promoting self-management strategies like mindfulness and coping skill development, individuals can better manage anxiety without turning to substances. Families play a vital role by fostering trust, emotional safety, and connection, which serve as protective factors against addiction. Community resources—ranging from mental health services to peer-led support and school-based initiatives—provide essential outreach and guidance. When these elements work together, they form a strong, multi-layered approach that not only addresses panic disorder but also helps prevent the onset of substance use disorders.
Video: Why Panic Attacks Make Addiction Worse