Common Traits in Addiction
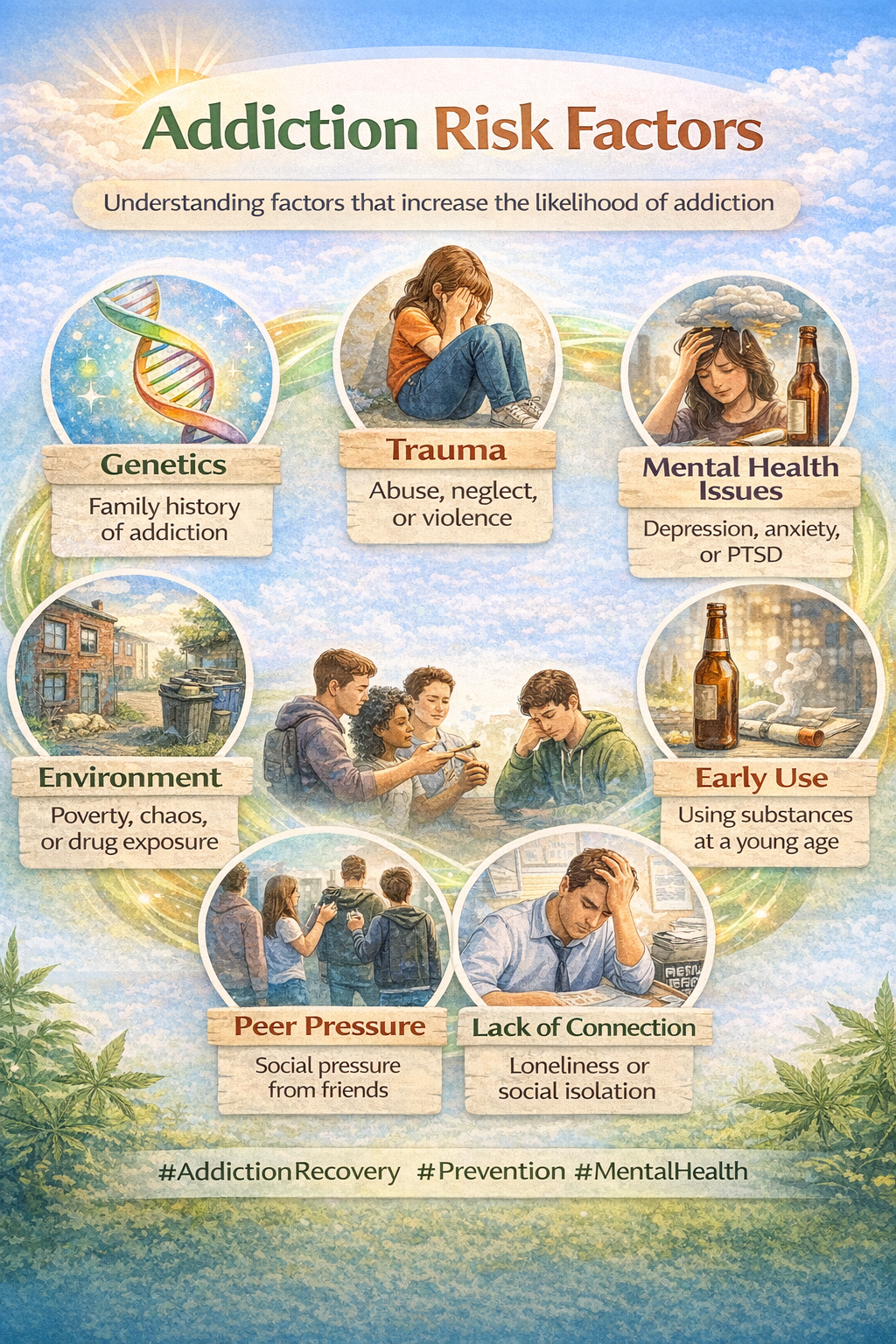
Addiction shows up in all sorts of forms, including alcohol, drugs, gambling, food, internet use, and much more. While every person’s experience is different, there are some key traits and patterns that a lot of people with addiction share, no matter the specifics. My goal here is to break down what people with addiction often … Read more