Opioid addiction, driven by the highly addictive nature of opioids, is marked by symptoms like physical dependence, tolerance, and behavioral changes. Risk factors for developing opioid use disorder (OUD) include genetic predisposition, mental health issues, and prior substance abuse. Addressing opioid addiction requires self-management strategies, such as proper medication use and healthy coping mechanisms, strong family support, including education and communication, and community resources like public education, alternative pain management options, and safe medication practices. These combined efforts are essential in preventing and managing opioid addiction.
Why Opioids Are Highly Addictive: Understanding the Key Factors
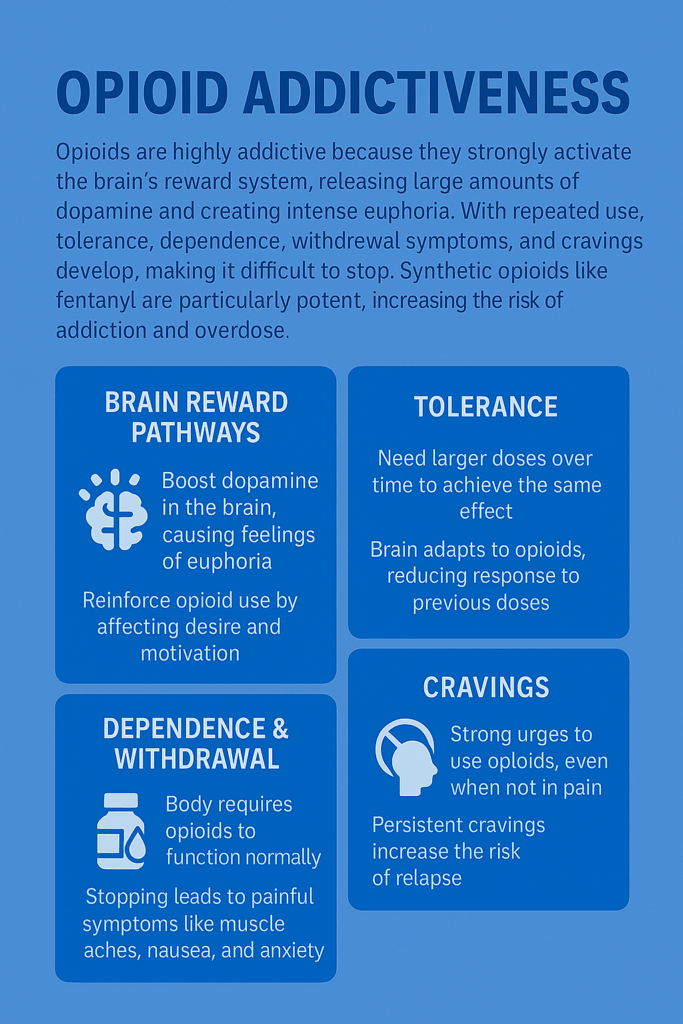
Opioids are among the most addictive substances due to their profound effects on the brain’s reward and pleasure systems. Understanding why opioids are so compelling and dangerous can shed light on the mechanisms behind opioid addiction. Here are the primary reasons:
1. Powerful Reward System Activation
Opioids strongly activate the brain’s reward system by triggering the release of dopamine, a neurotransmitter associated with pleasure and satisfaction. This surge in dopamine creates an intense feeling of euphoria, reinforcing the desire to use the drug repeatedly. The brain quickly associates opioids with pleasure, making it difficult to resist using them again.
2. Binding to Opioid Receptors
Opioids bind to mu-opioid receptors in the brain and spinal cord, leading to pain relief and a sense of well-being. While this helps manage pain, chronic activation of these receptors changes the brain’s chemistry. Over time, it becomes difficult for individuals to feel pleasure from everyday activities without the drug.
3. Tolerance Development
With continued opioid use, the body builds tolerance, meaning higher doses are required to achieve the same effect. This escalating need for more opioids increases the risk of addiction as individuals chase the euphoric feeling, leading them to consume dangerous amounts.
4. Dependence and Withdrawal
Physical dependence develops with prolonged opioid use, where the brain adapts to the drug’s presence. If use is reduced or stopped, withdrawal symptoms—such as nausea, anxiety, and muscle pain—occur. These symptoms are often so uncomfortable that individuals continue using opioids to avoid them, further perpetuating addiction.
5. Neuroplasticity Changes
Chronic opioid use causes lasting changes in brain structure and function, especially in regions responsible for decision-making, impulse control, and reward. These neuroplasticity changes make it harder to regulate drug-seeking behaviors and contribute to compulsive opioid use.
6. Emotional and Psychological Factors
Opioids can provide significant relief from emotional distress, anxiety, and stress, making them appealing as a coping mechanism. This emotional relief reinforces continued use, especially in individuals dealing with underlying mental health conditions, making it more challenging to quit.
7. Social and Environmental Influences
The availability of opioids and social factors such as peer pressure, stress, or trauma can also contribute to addiction. In environments where opioids are easily accessible or used as a social norm, the likelihood of developing an addiction increases.
8. Genetic and Individual Differences
Some individuals have a genetic predisposition to addiction, meaning their genetic makeup makes them more vulnerable to the addictive properties of opioids. These individual differences play a role in determining who may be more at risk for developing an opioid addiction.
The combination of biological, psychological, and environmental factors makes opioids incredibly addictive. Their ability to quickly create a sense of euphoria, coupled with tolerance, dependence, and lasting changes to brain chemistry, makes them challenging to use safely. Awareness of these risks is essential for preventing opioid misuse and addressing addiction effectively.
Understanding the Differences Between Opioid Dependence, Addiction, and Abuse
Opioids, while effective for managing pain, can lead to a range of issues if misused or used over long periods. It’s essential to understand the distinctions between opioid dependence, addiction, and abuse, as these terms describe different levels of interaction with the drug. Misunderstanding them can lead to confusion about treatment needs and risks. Here’s a breakdown of the key differences:
Opioid Dependence
Opioid dependence occurs when your body becomes physically reliant on the drug. After prolonged opioid use, the body adapts, leading to tolerance, meaning you may need more of the drug to feel the same effects. When you stop using opioids suddenly, you might experience withdrawal symptoms such as sweating, nausea, or anxiety. This physical reliance is not the same as addiction—it’s a natural response to continued use, even if opioids are used for legitimate medical reasons like pain relief.
However, dependence is a critical stage to be aware of because it signals the body’s growing reliance on opioids to function normally. Many people who take opioids for chronic pain management can become dependent but do not necessarily become addicted.
Opioid Addiction
Addiction, on the other hand, is much more complex. It’s a chronic brain disease characterized by compulsive opioid use despite the negative consequences it brings to one’s health, relationships, or career. Addiction involves both physical dependence and a psychological craving for the drug. It’s this compulsive need to continue using opioids, even when they’re not needed for pain or are causing harm, that defines addiction.
Unlike dependence, addiction drastically impacts everyday life. Individuals often lose control over their drug use, experience intense cravings, and prioritize drug use over responsibilities or well-being. Recovery from opioid addiction usually requires comprehensive treatment, including medical and behavioral therapy.
Opioid Abuse
Opioid abuse is a term used when someone misuses opioids, but it doesn’t necessarily mean they’re addicted or dependent—yet. Abuse typically involves taking opioids in higher doses, for longer than prescribed, or using them recreationally to achieve a high. Though opioid abuse may not immediately lead to addiction or dependence, it significantly raises the risks for both.
People engaging in opioid abuse might not have the compulsive behavior seen in addiction, but are still putting themselves at risk for serious health issues, including overdose. Recognizing opioid abuse early can help prevent the escalation of a full-blown addiction.
The Bottom Line
- Opioid Dependence: Physical reliance on opioids, often due to long-term medical use.
- Opioid Addiction: A chronic disease with both physical and psychological components leading to uncontrollable drug use.
- Opioid Abuse: Misuse of opioids that increases the risk of dependence and addiction, but doesn’t necessarily involve them.
Understanding these distinctions is critical in identifying the proper treatment approach and avoiding the dangerous consequences of opioid misuse. Whether it’s physical dependence, early-stage abuse, or full addiction, early intervention can make a significant difference in recovery outcomes.
Recognizing the Signs and Symptoms of Opioid Addiction
Opioid addiction can manifest in various ways, affecting an individual’s physical health, behavior, mental state, and social life. Understanding the key indicators can help identify when opioid use has progressed into addiction, a condition that often requires professional treatment. Here are some of the most common signs and symptoms:
Physical Symptoms
- Tolerance: Individuals may require increasingly larger doses of opioids to achieve the same effect, a hallmark of developing physical dependence.
- Withdrawal Symptoms: When opioid use is stopped or reduced, uncomfortable symptoms like nausea, vomiting, muscle aches, insomnia, and irritability occur.
- Changes in Sleep Patterns: Sleep disturbances, such as excessive drowsiness or insomnia, are associated with opioid use.
- Constipation: Persistent gastrointestinal issues, including constipation, are a known side effect of opioid use.
- Pupillary Changes: Constricted pupils (miosis) are a classic sign of opioid use, though dilated pupils can occur in some situations.
Behavioral Symptoms
- Increased Use: Taking opioids more frequently or in more significant amounts than initially intended, often beyond medical necessity.
- Neglecting Responsibilities: Failing to meet obligations at work, school, or home due to opioid use.
- Loss of Interest: Losing interest in hobbies or activities once enjoyed as drug use becomes the main focus.
- Secretive Behavior: Hiding drug use or lying about how often or how much is being consumed.
- Cravings: An intense and persistent desire to use opioids, even when not necessary for pain management.
Psychological Symptoms
- Mood Swings: Extreme mood changes, ranging from euphoria to agitation, often triggered by drug use or withdrawal.
- Anxiety and Depression: Many individuals struggling with opioid addiction report increased anxiety or bouts of depression.
- Cognitive Impairment: Difficulty concentrating, memory problems, or impaired judgment are common as opioids affect brain function.
Social and Interpersonal Symptoms
- Social Withdrawal: Individuals may start isolating themselves from friends and family to focus on drug use.
- Relationship Issues: Increased conflicts and strain in personal relationships due to erratic behavior, neglect, or dishonesty about drug use.
- Financial Problems: Opioid addiction often leads to spending large amounts of money on obtaining drugs, which can result in economic instability.
Health-Related Symptoms
- Frequent Illness: Recurrent infections, including those related to injection drug use, may occur, along with other health issues.
- Overdose Risk: Signs of overdose include difficulty breathing, loss of consciousness, or bluish skin (cyanosis), which are life-threatening and require immediate medical attention.
Signs of Physical Dependence
- Need for Medical Help: Individuals may require medical assistance to manage withdrawal symptoms or health complications caused by opioid use.
- Inability to Cut Down: Despite a desire to quit or cut back, many find it difficult to control or reduce their opioid consumption.
Recognizing the signs and symptoms of opioid addiction is crucial for early intervention. The physical, behavioral, psychological, and social effects of opioid addiction often indicate a more profound issue requiring comprehensive treatment. If you or someone you know is exhibiting these symptoms, it’s essential to seek professional help to address the addiction effectively and avoid further harm.
Understanding the Risk Factors for Opioid Dependency and Opioid Use Disorder (OUD)
Individuals at risk for opioid dependency and opioid use disorder (OUD) often share a combination of genetic, psychological, social, and environmental characteristics. Recognizing these key risk factors is essential for preventing opioid misuse and identifying those most vulnerable. Here are the major risk factors:
1. Genetic Predisposition
- Family History: A family history of substance abuse or mental health disorders significantly increases the likelihood of developing opioid dependency.
- Genetic Markers: Certain genetic variations influence how individuals metabolize opioids and may make them more susceptible to addiction.
2. Psychological Factors
- Mental Health Disorders: People with mental health conditions like depression, anxiety, or trauma are at higher risk of opioid misuse, often using opioids as a form of self-medication.
- Emotional Regulation: Difficulty managing emotions or coping with stress can lead individuals to rely on opioids as a way to relieve emotional discomfort.
3. Previous Substance Use
- History of Substance Abuse: Individuals who have abused other substances, including alcohol or illicit drugs, are at a greater risk of developing opioid dependency.
- Prior Prescription Drug Use: Previous use or misuse of prescription opioids can increase the risk of dependency, especially if opioids were used for extended periods or at high doses.
4. Social and Environmental Factors
- Peer Influence: Socializing with peers who misuse opioids or other substances can normalize and encourage opioid use.
- Stressful Life Events: Traumatic experiences, abuse, or significant life stressors, such as financial hardship or personal loss, can make individuals more vulnerable to opioid misuse.
- Socioeconomic Status: Individuals living in poverty or without access to healthcare and social support are at a higher risk of developing OUD due to limited resources for managing health and emotional stress.
5. Medical and Behavioral Factors
- Chronic Pain: Long-term opioid prescriptions for chronic pain can lead to dependence, especially if patients develop tolerance or begin to misuse their medications.
- High-Dose Prescription: Being prescribed high doses of opioids, particularly extended-release forms, raises the likelihood of dependence or misuse.
6. Cognitive and Behavioral Traits
- Impulsivity: Individuals who display impulsive behavior or frequently engage in risky activities are more likely to misuse opioids and other substances.
- Poor Coping Skills: The inability to effectively handle stress or emotional challenges may increase the likelihood of turning to opioids for relief.
7. Lack of Protective Factors
- Support Systems: Individuals without strong social support networks or positive role models are more vulnerable to opioid misuse.
- Protective Skills: Lacking effective strategies to resist peer pressure or manage stress further increases the risk of developing dependency.
Understanding these risk factors is crucial for identifying at-risk individuals and developing strategies to prevent opioid dependency and opioid use disorder. By recognizing the interplay of genetic, psychological, social, and environmental influences, healthcare providers, families, and communities can better support those vulnerable to opioid misuse and work toward more effective intervention and prevention efforts.
Self-Management Strategies to Prevent Opioid Dependency and Opioid Use Disorder (OUD)
Preventing opioid dependency and opioid use disorder (OUD) begins with proactive, informed decision-making. By incorporating self-management strategies, individuals can take charge of their health and pain management in ways that reduce the risk of opioid misuse. Here are key strategies for avoiding opioid dependency:
1. Educate Yourself
- Understanding Risks: Become informed about the potential risks of opioid use, including addiction and side effects, to make well-considered decisions about their use.
- Medication Awareness: Know the purpose, dosage, and potential alternatives to opioids, and discuss these options with your healthcare provider to find the best fit for your situation.
2. Follow Prescriptions Carefully
- Adhere to Dosage: Use opioids strictly as prescribed, without exceeding the recommended dosage or frequency.
- Consult Healthcare Providers: Regularly review the effectiveness of your opioid treatment with your healthcare provider to determine if continued use is necessary or if adjustments should be made.
3. Explore Alternative Pain Management
- Non-Opioid Medications: Consider non-opioid pain relievers, such as acetaminophen or ibuprofen, which may be effective for your condition.
- Therapeutic Options: Consider alternative pain management strategies, such as physical therapy, acupuncture, massage therapy, or chiropractic care.
4. Develop Healthy Coping Mechanisms
- Stress Management: Practice techniques like mindfulness, meditation, or yoga to manage stress, which can exacerbate pain and lead to opioid misuse.
- Emotional Support: Engage in therapy or counseling to address emotional or psychological challenges that may contribute to opioid dependency.
5. Avoid Misuse and Diversion
- Proper Storage: Keep opioids stored in a secure place, out of reach of others, to prevent unauthorized use.
- Disposal: Safely dispose of unused or expired opioids through drug take-back programs or approved methods to avoid potential misuse.
6. Monitor and Address Early Signs of Dependency
- Self-Assessment: Regularly check in with yourself to identify any patterns of increased opioid use, cravings, or dependency.
- Seek Help Early: If you notice any signs of dependency, seek professional help immediately to prevent the situation from escalating.
7. Build a Support Network
- Social Support: Engage with family and friends who can help you manage pain and stay accountable for following your treatment plan.
- Support Groups: Consider joining support groups for individuals managing chronic pain or recovering from addiction for additional community and resources.
8. Maintain a Healthy Lifestyle
- Balanced Diet and Exercise: A healthy diet and regular physical activity can improve overall well-being and reduce pain.
- Adequate Sleep: Prioritize getting sufficient rest and quality sleep, which can significantly manage pain and enhance overall health.
9. Regular Medical Check-Ups
- Monitor Health: Stay in contact with healthcare providers for regular check-ups and to ensure your pain management plan remains adequate.
- Adjust Treatments: Be open to adjusting your treatment plan based on ongoing health assessments and professional advice.
By implementing these self-management strategies, individuals can significantly reduce their risk of opioid dependency and OUD. These approaches encourage responsible medication use, healthy coping mechanisms, and a proactive mindset toward overall health and well-being.
The Crucial Role of Family Support in Preventing Opioid Dependency and Opioid Use Disorder (OUD)
Family support is a critical factor in preventing opioid dependency and opioid use disorder (OUD). When families come together to create a supportive, informed, and proactive environment, they can significantly reduce the risk of opioid misuse among their loved ones. Here are effective strategies that families can implement to support individuals at risk:
1. Educate and Inform
- Understanding Risks: Families should educate themselves about the dangers of opioid use, including the signs of dependency and addiction. This knowledge helps them identify potential issues early.
- Medication Awareness: Learn about safe opioid use, proper dosing, and the importance of disposing of unused medications to prevent misuse within the household.
2. Promote Safe Medication Practices
- Adherence to Prescriptions: Encourage strict adherence to prescribed dosages and schedules. Never alter medication regimens without consulting a healthcare provider, as improper use increases the risk of dependency.
- Secure Storage: Store opioids in a safe and secure location, out of reach of children and other family members, to reduce the potential for accidental misuse.
3. Support Healthy Alternatives
- Encourage Alternatives: Help explore and promote alternative pain management methods such as physical therapy, counseling, or non-opioid medications that can provide relief without the risks associated with opioids.
- Healthy Lifestyle: Encourage a healthy lifestyle, emphasizing regular physical activity, balanced nutrition, and stress-reducing practices, all of which can contribute to pain management and emotional well-being.
4. Foster Open Communication
- Discuss Concerns: Maintain open, nonjudgmental conversations about opioid use and any concerns regarding its potential impact. This helps family members feel comfortable discussing their experiences and seeking help.
- Encourage Seeking Help: If you notice any signs of opioid misuse or dependency, encourage your loved one to seek professional help early before the issue worsens.
5. Create a Supportive Environment
- Emotional Support: Offer consistent emotional support and understanding, particularly for those managing chronic pain or a medical condition that requires opioids. This emotional connection can reduce the likelihood of misuse.
- Monitor Behavior: Keep a watchful eye on any behavioral changes that may indicate opioid dependency, such as increased secrecy or mood swings, and provide compassionate support if concerns arise.
6. Promote Access to Resources
- Professional Help: Help find healthcare professionals, pain management experts, or addiction specialists who can guide and treat those at risk.
- Support Groups: Encourage participation in support groups where individuals managing chronic pain or those in recovery can find community resources.
7. Address Underlying Issues
- Mental Health Support: Recognize and address underlying mental health conditions such as anxiety, depression, or trauma that could contribute to opioid misuse. Access to proper mental health care is critical.
- Coping Skills: Help family members develop healthy coping mechanisms to deal with stress and emotional pain, reducing the likelihood of turning to opioids as an escape.
8. Set Boundaries and Expectations
- Clear Guidelines: Establish clear rules and expectations regarding medication use, emphasizing the importance of following medical advice and maintaining healthy behaviors.
- Accountability: Encourage personal responsibility and accountability in managing opioid prescriptions, reinforcing the importance of adherence to treatment plans.
9. Be Prepared for Emergencies
- Emergency Plans: Have a well-defined plan in place for responding to signs of overdose or severe opioid misuse. Know when and how to seek emergency medical help.
- Naloxone Access: Consider keeping naloxone, an opioid overdose reversal medication, in the home and ensure family members know how to use it if necessary.
By implementing these strategies, families can play a proactive and supportive role in preventing opioid dependency and OUD. Education, open communication, emotional support, and access to resources are vital to creating a safer, healthier environment for at-risk individuals. Through these efforts, families can help reduce the risk of opioid misuse and foster long-term well-being.
Community Resource Strategies to Prevent Opioid Dependency and Opioid Use Disorder (OUD)
Communities play a vital role in preventing opioid dependency and opioid use disorder (OUD) by providing education, resources, and support to individuals at risk. Communities can create a safer, healthier environment by implementing comprehensive prevention and intervention strategies. Here are key strategies that focus on prevention, education, and support:
1. Public Education and Awareness
- Educational Campaigns: Launch wide-reaching community educational campaigns to raise awareness about the risks of opioid use, encourage safe medication practices, and inform people about the signs of addiction.
- School Programs: Implement drug prevention programs in schools that teach students about the dangers of opioid misuse while promoting healthy coping mechanisms and lifestyles.
2. Access to Alternatives
- Pain Management Clinics: Develop and promote clinics specializing in alternative pain management techniques, such as physical therapy, acupuncture, and non-opioid medications, to reduce reliance on opioids.
- Mental Health Services: Ensure accessible mental health services are available for those dealing with stress, trauma, or emotional issues, as these factors often contribute to opioid misuse.
3. Community-Based Support Programs
- Support Groups: Establish support groups for individuals and families affected by opioid use. These groups provide a safe space for sharing experiences, offering peer support, and connecting people to local resources.
- Hotlines and Counseling: Offer 24/7 helplines and counseling services to provide immediate advice and support for those struggling with opioid-related challenges.
4. Access to Treatment and Recovery Services
- Substance Use Disorder Treatment: Expand access to addiction treatment services, including medication-assisted treatment (MAT) and behavioral therapies, to help individuals recover from opioid dependency.
- Rehabilitation Programs: Provide accessible community-based rehabilitation programs that offer holistic recovery options for those seeking long-term recovery from opioid misuse.
5. Safe Medication Practices
- Prescription Drug Monitoring Programs: Promote and implement state and local prescription drug monitoring systems to track opioid prescriptions and help prevent misuse.
- Drug Take-Back Programs: Organize drug take-back events and establish permanent drop-off locations for the safe disposal of unused or expired medications, reducing the risk of misuse.
6. Training and Capacity Building
- Training for Professionals: Provide specialized training for healthcare providers, educators, and community leaders to help them recognize and address opioid misuse and dependency professionally.
- Community Workshops: Offer workshops and seminars on safe medication use, opioid addiction prevention, and available community resources to empower individuals and families.
7. Policy and Advocacy
- Support Legislation: Advocate for policies and legislation that focus on opioid misuse prevention, expanding access to treatment services, and enhancing community health resources.
- Funding and Resources: Secure funding to support community programs and initiatives aimed at preventing opioid dependency and improving access to treatment and recovery services.
8. Strengthen Community Networks
- Partnerships: Foster collaborative partnerships among healthcare providers, law enforcement, local government, and community organizations to address opioid-related issues.
- Community Engagement: Actively involve community members in developing, planning, and implementing strategies to prevent opioid misuse and offer support to those affected.
9. Promote Healthy Lifestyles
- Community Activities: Organize community events that promote physical activity, mental well-being, and social engagement as healthy alternatives to opioid use.
- Youth Programs: Create youth-focused initiatives that offer mentorship, recreational opportunities, and skills development to reduce risk factors for opioid misuse among young people.
By adopting these community resource strategies, communities can create a supportive environment that not only prevents opioid dependency but also helps individuals manage pain and seek recovery in a safe and supportive way. Collaborative efforts involving education, access to alternatives, and strong community support are essential to building resilience against opioid misuse.
Frequently Asked Questions
Here are some common questions:
Do prescription opioids carry the same addiction risk as illicit opioids?
Yes. Prescription opioids affect the brain the same way as heroin or fentanyl. While dosing and purity may differ, the addictive potential is similar, especially with prolonged or non-medical use.
Why does mixing opioids with other drugs increase addiction and overdose risk?
Combining opioids with alcohol, benzodiazepines, or stimulants increases strain on the brain and body. These combinations raise overdose risk and can intensify addictive patterns.
Can opioids change the brain long term?
Yes. Chronic opioid use alters brain regions involved in reward, stress, and decision-making. Some changes improve with recovery, but vulnerability to relapse may persist.
Conclusion
The addictive nature of opioids, evident through symptoms like physical dependence and behavioral changes, presents significant challenges in managing opioid use disorder (OUD). Individuals at risk often face factors such as genetic predisposition, mental health issues, and past substance abuse. Effective management of opioid addiction necessitates a multifaceted approach, including self-management strategies to ensure proper medication use and stress management, strong family support through education and open dialogue, and comprehensive community resources strategies such as public awareness, alternative pain management, and safe medication practices. By integrating these approaches, we can more effectively prevent and address opioid addiction, fostering healthier outcomes for individuals and communities.
Video: The Opioid Cycle That Keeps Addicts Trapped #crisis #awareness