Opioid Use Disorder (OUD) in older adults is a growing concern, driven by chronic pain, multiple prescriptions, age-related changes, and social isolation. Prevention requires a comprehensive approach: self-management through safe medication use, health check-ups, and non-opioid pain care; family support through open communication, prescription monitoring, and healthy routines; and community resources such as wellness programs, caregiver education, and counseling to keep older adults safe and supported.
The Silent Epidemic: Understanding the Rise of Opioid Use Disorder in Older Adults
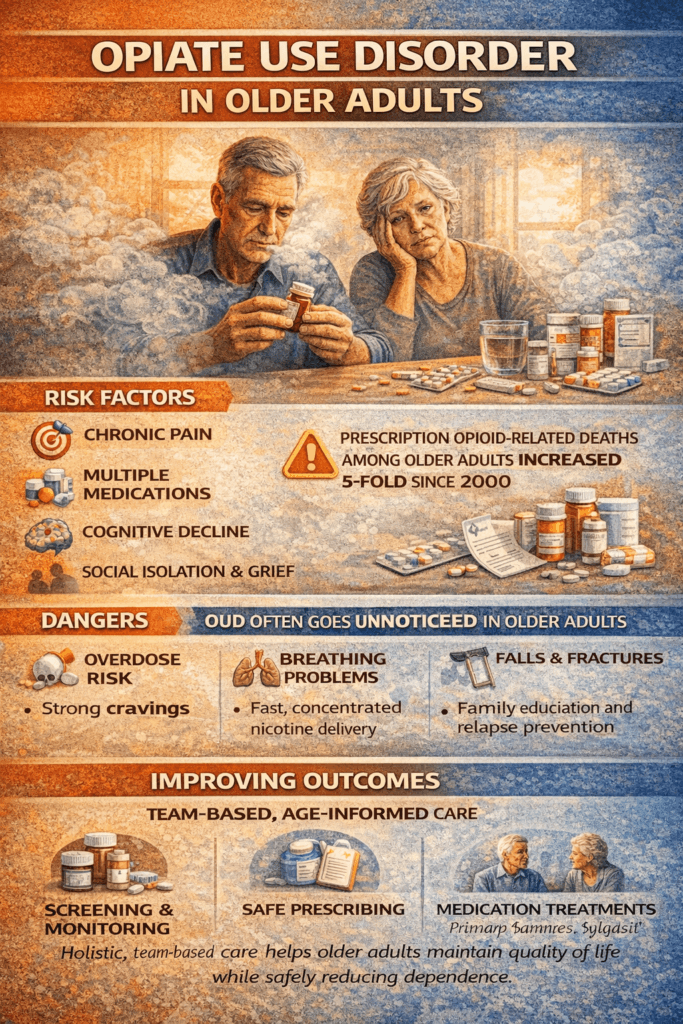
Opioid Use Disorder (OUD) is often associated with younger populations, but recent trends show a troubling rise among older adults. This shift is driven by a unique combination of medical, social, and biological factors that make older adults especially vulnerable. Understanding these influences is key to prevention, early detection, and effective treatment.
1. Chronic Pain and Prescription Opioids
Chronic pain conditions such as arthritis, neuropathy, or back problems are more common in older age. To manage this pain, many older adults are prescribed opioids. While these medications can provide relief, long-term use often leads to tolerance and dependence. The risk escalates when higher doses are prescribed or when opioids are combined with other sedatives.
2. Polypharmacy and Drug Interactions
Older adults are more likely to take multiple medications (polypharmacy). Mixing opioids with sedatives, benzodiazepines, or even alcohol can magnify their effects, raising the risk of dependence and overdose. Accidental misuse becomes more likely as medication regimens grow more complex.
3. Physiological Changes with Aging
With age, the body processes medications differently. Reduced kidney and liver function can cause opioids to remain in the system longer, increasing sensitivity and risk of overdose. Cognitive decline adds another layer of vulnerability, making it harder for some individuals to manage dosing instructions properly.
4. Mental Health and Social Factors
Depression, isolation, and grief are common challenges in later life. Retirement, loss of loved ones, or social disconnection can make older adults more likely to turn to substances, including opioids, as a coping mechanism.
5. Historical Prescription Practices
Many older adults were prescribed opioids during a time when long-term use was encouraged, and risks were downplayed. This historical exposure has contributed to prolonged use and higher rates of OUD in today’s older population.
6. Underdiagnosis and Stigma
OUD in older adults is often underdiagnosed because its symptoms—fatigue, memory issues, or falls—can be mistaken for normal aging. Stigma also prevents many from seeking help, allowing misuse to progress unchecked.
In summary, the rise of OUD among older adults is not the result of a single cause but a complex web of chronic pain management, medication interactions, physiological vulnerability, mental health challenges, and overlooked substance use. Addressing this issue requires age-specific interventions: careful prescribing, better screening, and integrated support that treats both the physical and emotional needs of older adults. By recognizing and responding to these risks, healthcare systems and families can better protect older adults from this silent epidemic.
Empowering Older Adults: Self-Management Strategies to Prevent Opioid Use Disorder
Opioid Use Disorder (OUD) among older adults is an emerging concern. Factors such as chronic pain, multiple prescriptions, and age-related health changes make this population especially vulnerable. However, prevention is possible. By adopting self-management strategies tailored to their unique needs, older adults can reduce risks and maintain independence while effectively managing pain.
1. Medication Awareness and Management
A proactive approach to medication is one of the strongest safeguards against OUD. Older adults should maintain an up-to-date medication list and review it regularly with healthcare providers. Opioids must be taken exactly as prescribed, without increasing doses independently. Combining opioids with alcohol, benzodiazepines, or other sedatives should be avoided unless approved by a clinician. Tools like pill organizers or digital reminders can help prevent missed or duplicate doses.
2. Non-Opioid Pain Management
Opioids are not the only solution for chronic pain. Physical therapy, gentle exercise, stretching, and mobility programs can ease discomfort and improve function. Alternatives such as topical treatments, NSAIDs, or acetaminophen may be safer options when appropriate. Mind-body practices—like meditation, yoga, tai chi, or cognitive behavioral therapy (CBT)—offer additional relief by addressing both pain and stress.
3. Regular Health Monitoring
Consistent medical follow-up is essential. Routine check-ups help track pain, mobility, and emotional well-being. Screening for sleep issues, depression, or anxiety can identify early contributors to opioid misuse. Recognizing early warning signs—such as cravings, dose escalation, or withdrawal symptoms—allows for timely intervention.
4. Education and Awareness
Knowledge is a powerful prevention tool. Understanding the risks of long-term opioid use, as well as the dangers of dependence and overdose, can guide safer decisions. Safe storage and proper disposal of unused medications also protect loved ones and reduce misuse risks.
5. Social and Emotional Support
Isolation and grief can increase vulnerability. Maintaining strong connections with family, friends, and community groups provides emotional stability. Peer support groups and counseling can reduce loneliness and help process difficult emotions. Open communication with caregivers about pain, medication side effects, and concerns fosters trust and early problem-solving.
6. Healthy Lifestyle Habits
Healthy routines can lessen reliance on opioids. Adequate sleep, balanced nutrition, and regular physical activity support overall well-being. Avoiding tobacco, excessive alcohol, and illicit substances further reduces risk. Minor lifestyle adjustments can significantly improve both mood and pain management.
7. Develop an Action Plan
Preparation is key. Older adults should have a plan for managing flare-ups, cravings, or accidental overuse, including when to contact healthcare providers. If naloxone is prescribed, both patients and caregivers should know how to use it in an emergency.
In summary, older adults face unique risks for OUD, but prevention is within reach. By practicing medication awareness, exploring non-opioid pain management, staying engaged with healthcare, building strong support networks, and maintaining healthy habits, older adults can safeguard themselves against misuse. An individualized action plan further ensures safety. These strategies highlight the power of awareness, prevention, and proactive engagement with healthcare providers—helping older adults live healthier, safer lives.
How Families Can Help Older Adults Prevent Opioid Use Disorder
Opioid Use Disorder (OUD) is an increasing concern among older adults due to chronic pain, multiple medications, and age-related health changes. Families play a vital role in prevention by offering structure, guidance, and emotional connection. With the right strategies, caregivers and loved ones can reduce risks while promoting healthier, safer aging.
1. Monitoring and Assistance with Medications
Families can help older adults stay safe by supporting medication management. This may include setting up pill boxes, reminders, or charts to avoid missed or double doses. Loved ones should also encourage adherence to prescribed amounts and watch for signs of misuse, such as taking higher doses without approval. Safe storage and proper disposal of unused opioids are essential steps to prevent accidental or intentional misuse.
2. Education and Awareness
Knowledge empowers both families and older adults. Families should learn about the risks, side effects, and safe use of opioids. Having open conversations about the importance of following medical guidance and exploring non-opioid alternatives helps reduce dependence while improving pain management options.
3. Emotional and Social Support
Isolation, grief, and depression often make older adults more vulnerable to substance misuse. Families can counteract this by offering companionship, frequent check-ins, and emotional support. Encouraging participation in community groups, hobbies, or peer support programs provides meaningful social connections and healthy coping outlets.
4. Advocacy in Healthcare
Family members can be strong advocates in medical settings. Attending appointments, asking questions about pain management, and discussing non-opioid alternatives help ensure safe prescribing. By actively engaging in care discussions, families support informed decision-making and reduce the risk of long-term opioid dependence.
5. Encouraging Healthy Lifestyle Habits
Daily routines can make a big difference. Families can support older adults in maintaining regular exercise, balanced nutrition, and consistent sleep—all of which naturally improve mood and reduce pain. Discouraging alcohol, tobacco, or other substances further lowers the risk of OUD.
6. Crisis Preparedness
Families should be prepared for emergencies. This includes keeping healthcare providers’ contact information accessible and ensuring naloxone is available if prescribed. Recognizing early warning signs such as escalating doses, withdrawal symptoms, or sudden behavioral changes allows for prompt intervention and prevention of overdose.
In summary, families are on the front line of protecting older adults from OUD. By offering structured medication management, emotional connection, ongoing education, and active healthcare advocacy, loved ones can make a profound difference. Supporting healthy routines and being prepared for crises ensures that older adults not only stay safe but also thrive with dignity and resilience.
Strengthening Communities: Resources to Help Older Adults Prevent Opioid Use Disorder
Opioid Use Disorder (OUD) among older adults is a growing concern, shaped by chronic pain, multiple medications, and the challenges of aging. While families and healthcare providers play a critical role, community resources are equally important in reducing risks and supporting safe, healthy aging. By building strong networks of care, education, and prevention, communities can help older adults avoid the pitfalls of opioid misuse.
1. Access to Healthcare Services
Regular access to medical care is essential. Communities can strengthen prevention efforts by ensuring older adults have connections to primary care providers, pain specialists, and geriatric experts. Expanding telehealth services can bridge barriers for those with mobility or transportation challenges, ensuring consistent monitoring of pain and medications.
2. Medication Disposal and Safety Programs
Unused medications can pose significant risks if not properly handled. Community take-back programs and pharmacy-based disposal sites provide safe ways to eliminate leftover opioids. Public education on safe storage also helps reduce accidental ingestion or diversion.
3. Non-Opioid Pain Management Programs
Communities can promote healthier alternatives for pain management by offering access to physical therapy, exercise classes, and rehabilitation programs. Workshops in mindfulness, yoga, or tai chi provide both physical and emotional benefits. Where available, complementary therapies like acupuncture or massage can further expand non-opioid options.
4. Support Groups and Peer Networks
Social isolation can increase vulnerability to opioid misuse. Senior centers, recovery groups, and social clubs help older adults build supportive relationships. Peer programs explicitly designed for those managing chronic pain or substance use risk offer an added layer of connection and understanding.
5. Educational Workshops
Community-based education is a powerful prevention tool. Hosting workshops on safe opioid use, addiction risks, and non-opioid pain strategies raises awareness among older adults. Training sessions for caregivers and family members can also ensure early recognition of misuse or dependence.
6. Emergency Preparedness
Readiness saves lives. Communities should expand access to naloxone through pharmacies, health departments, and community programs. Training older adults, caregivers, and peers in overdose recognition and response ensures timely action in emergencies. Local EMS and public health outreach further strengthen community safety nets.
7. Policy and Advocacy Support
Sustainable prevention requires systemic change. Advocating for age-appropriate OUD prevention programs and securing funding for senior-focused addiction services can expand access to care. Public health campaigns targeted at older adults raise awareness about opioid risks and safer alternatives.
In summary, preventing OUD among older adults requires more than individual action—it depends on strong community systems. By improving healthcare access, supporting safe medication practices, promoting non-opioid therapies, fostering social networks, providing education, and preparing for emergencies, communities can reduce risks and protect older adults. Coordinated efforts not only safeguard health but also create more resilient, connected communities where older adults can thrive.
Frequently Asked Questions
Here are some common questions:
Question: Provide a conversation script to discuss potential OUD with older adults in their medical care.
Answer: A gentle, respectful, and educational conversation script you can use to discuss potential OUD risks with older adults during medical care:
Conversation Script: Discussing OUD Risk with Older Adults
Clinician:
“Hi [Name], I wanted to take a few minutes to talk about the medications you’re taking for pain. Many people your age are prescribed opioids, and while they can help with pain, they can also have risks if not managed carefully.”
Patient:
“What kind of risks?”
Clinician:
“Some risks include dependence or addiction, which is called opioid use disorder, as well as side effects like sleepiness, constipation, or confusion. Because our bodies change as we age, opioids can stay in your system longer and increase these risks.”
Patient:
“I’ve been taking them for a while. Does that mean I’m addicted?”
Clinician:
“Not necessarily. Many people take opioids safely for pain. But it’s important to be aware of the warning signs, like needing higher doses for the same pain relief, feeling like you can’t function without the medication, or taking it in ways other than prescribed.”
Patient:
“What can I do to avoid that?”
Clinician:
*”There are several strategies we can use together:
- Take your medications exactly as prescribed.
- Keep track of your doses and any side effects.
- Explore non-opioid options for pain, like physical therapy, gentle exercise, or topical treatments.
- Stay connected socially and engage in activities you enjoy, as isolation can increase risk.
- Let us know if you feel cravings, withdrawal, or if the medication isn’t helping as it should.”*
Patient:
“That sounds manageable. But what if I slip up?”
Clinician:
“If that happens, don’t be afraid to tell us. There’s support available, including counseling, peer programs, and, if necessary, medication-assisted treatment. The goal is to manage your pain safely while keeping you healthy and independent.”
Clinician (closing):
“We’ll work together to make sure your pain is managed safely. Do you have any questions or concerns about your medications right now?”
Tips for Effectiveness:
Reinforce that early intervention is protective, not punitive.
Use simple, clear language; avoid medical jargon.
Be nonjudgmental and empathetic to reduce stigma.
Emphasize partnership and shared decision-making.
Question: Provide a conversation script to discuss potential OUD with older family members in their medical care.
Answer: A respectful, clear conversation script for talking to older family members about potential opioid use disorder (OUD) in their medical care:
Family Conversation Script: Addressing OUD Risk with Older Adults
Family Member:
“Grandma/Grandpa, I wanted to check in about your medications for pain. Are you okay talking about that?”
Older Adult:
“Sure, what about it?”
Family Member:
“I know you’ve been taking [name of medication] for your pain. These medications can help, but they also have some risks, especially for older adults, like dependence or something called opioid use disorder. That means the body can get used to them, and it might be harder to manage if the dose isn’t monitored.”
Older Adult:
“Does that mean I’m addicted?”
Family Member:
“Not at all. Lots of people take these medications safely. We want to make sure you stay healthy and avoid problems before they happen. There are signs to watch for, like needing more medicine to get the same relief, feeling like you can’t go without it, or taking it differently than prescribed.”
Older Adult:
“So what should I do?”
Family Member:
*”Some helpful steps include:
- Taking your medications exactly as prescribed.
- Keeping track of doses and side effects.
- Ask your doctor about non-opioid options for pain, like physical therapy or topical treatments.
- Staying socially connected and active.
- Letting us or your doctor know if anything feels off or if you’re worried about the medications.”*
Older Adult:
“I see. I’ll try to keep that in mind.”
Family Member:
“We’re here to help you manage your pain safely. We can even go to appointments together if you want, to ask your doctor any questions. Our goal is to make sure you stay comfortable and healthy without unnecessary risks.”
Tips for Effectiveness:
Encourage open communication with healthcare providers.
Stay calm and nonjudgmental; avoid implying blame.
Use simple, clear language appropriate for older adults.
Emphasize support and teamwork—that the conversation is about safety, not control.
Question: Provide a self-management toolkit about avoiding OUD in the older population with health conditions.
Answer: A self-management toolkit designed specifically for older adults with health conditions to help prevent opioid use disorder (OUD). It’s structured for practical use, combining education, strategies, and resources.
Self-Management Toolkit: Preventing Opioid Use Disorder in Older Adults
1. Understand Your Medications
- Keep a medication list: Track all prescriptions, over-the-counter drugs, and supplements.
- Follow prescriptions exactly: Never change the dose or schedule without consulting your healthcare provider.
- Know side effects: Be aware of sedation, constipation, confusion, or dizziness.
- Avoid mixing substances: Alcohol, sedatives, or recreational drugs can increase risk.
2. Pain Management Alternatives
- Non-opioid medications: Acetaminophen, NSAIDs, or topical analgesics as recommended by your doctor.
- Physical therapy & gentle exercise: Walking, swimming, stretching, or strength training.
- Mind-body approaches: Meditation, yoga, tai chi, or cognitive behavioral therapy for pain and stress.
- Complementary therapies: Massage, acupuncture, or heat/cold therapy where appropriate.
3. Healthy Lifestyle Practices
- Nutrition: Eat a balanced diet rich in fruits, vegetables, and whole grains.
- Sleep: Aim for 7–8 hours per night; manage insomnia without sedatives if possible.
- Exercise: Stay active daily to reduce pain, improve mood, and maintain independence.
- Avoid risky substances: Limit alcohol, tobacco, or other drugs.
4. Monitoring and Tracking
- Use pill organizers or apps to manage doses.
- Track pain levels and side effects in a journal to discuss with your healthcare provider.
- Watch for warning signs: Increased dose needs, cravings, or using medication differently than prescribed.
5. Social and Emotional Support
- Stay connected: Engage with family, friends, or community groups to reduce isolation.
- Seek counseling or peer support if experiencing depression, grief, or stress.
- Discuss concerns openly with family or caregivers about medication use.
6. Communication with Healthcare Providers
- Attend regular appointments and review your medications.
- Ask about non-opioid options for pain.
- Inform your provider about all other medications and health conditions.
- Plan for safe tapering if opioid use is prolonged or no longer necessary.
7. Emergency Preparedness
- Know the signs of overdose: Extreme sleepiness, slowed breathing, or unresponsiveness.
- Have a plan: Keep emergency contacts handy.
- Naloxone: Ask your healthcare provider if you should have access to naloxone for emergencies.
8. Resources
- SAMHSA Helpline: 1-800-662-4357 (for information and support)
- National Institute on Aging: https://www.nia.nih.gov
- Local senior centers: Often provide support groups, exercise classes, and counseling.
- Community pain management programs: Check hospitals or clinics for workshops and classes.
Tip: Keep this toolkit handy and review it regularly with your healthcare provider or family members to stay proactive in preventing OUD.
Conclusion
OUD in older adults is a complex issue shaped by medical, psychological, and social factors, but it can be prevented through coordinated strategies. By combining self-management practices that encourage safe and mindful medication use, family support systems that promote accountability and emotional care, and community resources that provide education and accessible alternatives, older adults can be protected from the risks of opioid misuse. A proactive, collaborative approach ensures healthier aging and reduces the burden of OUD in this vulnerable population.
Video: The Surprising Science Behind Seniors And Opioid Addiction