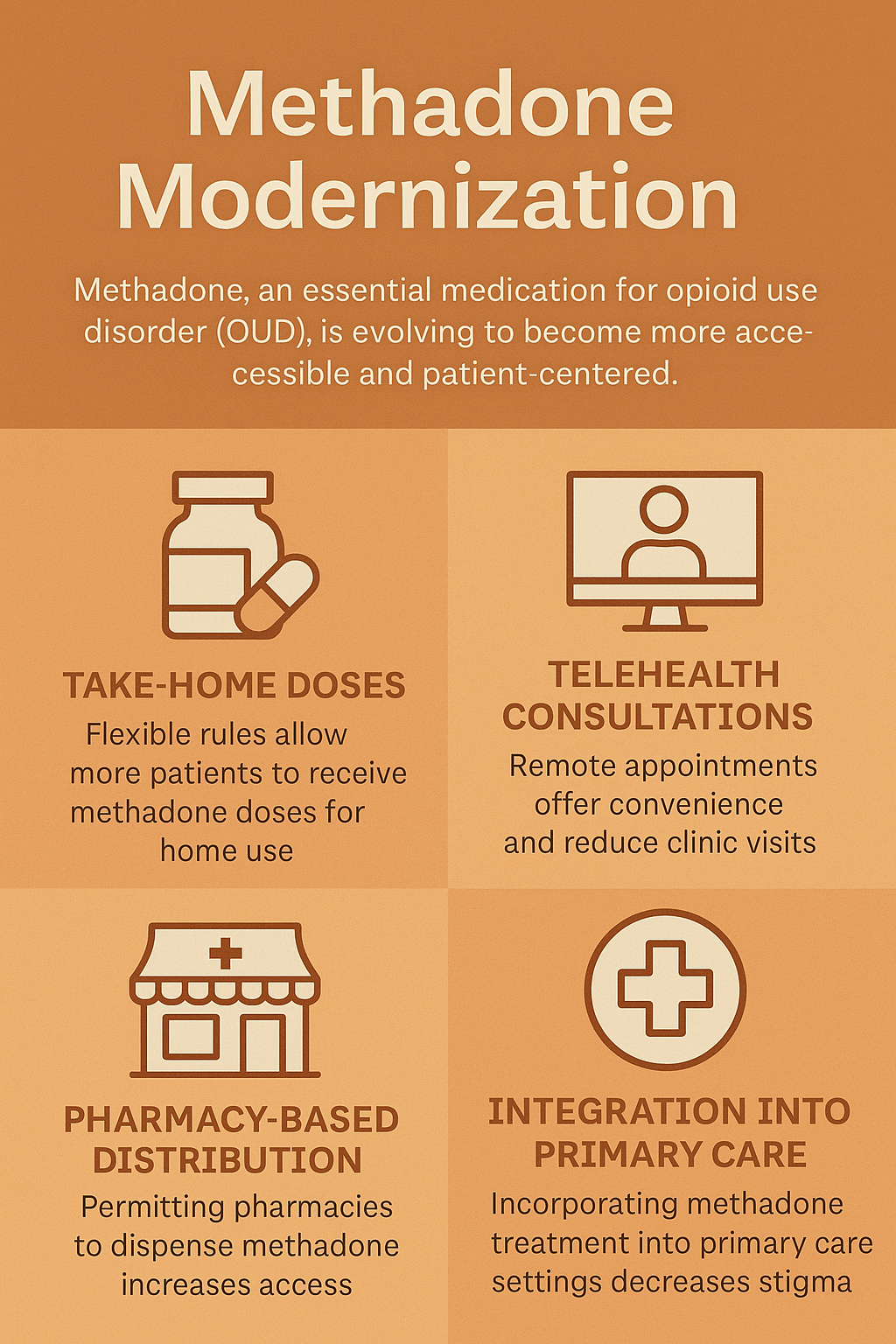
Methadone modernization is a transformative approach to opioid use disorder (OUD) treatment that aims to expand access, improve flexibility, and integrate care into more community-based and patient-centered settings. By allowing take-home dosing, pharmacy-based distribution, and care outside of traditional opioid treatment programs (OTPs), this model empowers individuals with more autonomy and dignity in recovery. However, it also brings disadvantages and ethical dilemmas, including concerns about diversion, uneven quality of care, and potential over-commercialization. To succeed, methadone modernization must be paired with strong self-management practices, engaged family support, and community resource strategies—such as peer recovery networks, mobile clinics, and primary care integration—to ensure safety, equity, and sustained recovery for all.
Methadone Modernization: Bringing Opioid Treatment into the 21st Century
Methadone Modernization refers to ongoing efforts to reform how methadone—a gold-standard medication for opioid use disorder (OUD)—is regulated, prescribed, and accessed in the United States. These efforts aim to expand access, reduce stigma, and bring treatment practices in line with current medical and public health standards, especially as the landscape of substance use disorder (SUD) treatment continues to evolve.
🔍 Key Elements of Methadone Modernization
1. Decentralizing Access
Traditionally, methadone can only be dispensed through federally certified opioid treatment programs (OTPs)—a system that is highly regulated and often stigmatized. Modernization efforts promote:
- Office-based prescribing by qualified healthcare providers
- Integration into primary care clinics, community pharmacies, and mobile treatment units
- Expanded availability in rural and underserved communities
2. Flexible Take-Home Dosing
During the COVID-19 pandemic, federal regulations were temporarily relaxed to allow more patients to take methadone home. Modernization supports:
- Permanent policy reforms for flexible, individualized take-home dosing
- Increased trust in patient stability and self-management
- Reduced daily travel demands for patients, particularly those who work or care for others
3. Reducing Stigma and Discrimination
Modernization efforts aim to reshape public and clinical perceptions of methadone, emphasizing its legitimacy as a routine medical treatment rather than a last resort or court-mandated measure. This involves:
- Training healthcare providers on evidence-based addiction treatment
- Public education to normalize methadone as part of standard care
4. Updating Safety and Monitoring Tools
Modernization also calls for better tools and infrastructure to support safe, effective methadone use, including:
- Integrated data systems
- Digital health tools for patient monitoring
- Standardized metrics for outcomes and quality assurance
⚖️ The Shifting Regulatory Space in SUD Treatment
🏛️ 1. Policy Reforms
Key federal agencies such as SAMHSA and the DEA are reviewing outdated regulations and considering updates to meet current public health needs better.
- Bipartisan support is growing for modernization.
- Reforms are driven by the need to address rising overdose rates and gaps in treatment
📉 2. Public Health Focus
The regulatory mindset is shifting from criminal-justice-based control toward a health-centered approach that views addiction as a chronic, manageable medical condition.
- Focus on harm reduction, treatment equity, and integration into broader healthcare
🧠 3. Expanded Roles for Healthcare Providers
Modernization includes expanding the scope of who can provide methadone care:
- Primary care providers, nurse practitioners, and pharmacists are being encouraged to play active roles
- Requires updated training, streamlined certification pathways, and legal protections
🧾 Summary: Why Methadone Modernization Matters
| Traditional System | Modernized Approach |
|---|---|
| Daily clinic visits required | Flexible, take-home dosing based on stability |
| Only certified OTPs can dispense | Office-based, pharmacy, and telehealth access |
| Heavily regulated and stigmatized | Normalized as part of mainstream addiction care |
| Limited access in rural or underserved areas | Expansion to primary care and community settings |
The Ethics of Methadone Modernization: Balancing Access, Safety, and Equity
The modernization of methadone treatment offers a hopeful path forward in the fight against opioid addiction by increasing access, reducing stigma, and streamlining care. However, this shift also presents complex ethical dilemmas that require careful consideration from clinicians, policymakers, and communities. As methadone becomes more accessible through pharmacies and primary care, the system must weigh critical concerns around safety, equity, continuity of care, and patient autonomy.
⚖️ Ethical Dilemmas of Methadone Modernization
1. 🧪 Balancing Access with Safety
Dilemma: How do we expand methadone access without increasing risks of misuse, diversion, or overdose?
- More take-home doses and decentralized dispensing reduce barriers—but could endanger safety without proper safeguards.
- Patient empowerment must be balanced with the realities of methadone’s potency.
2. 🏥 Ensuring Quality and Continuity of Care
Dilemma: Can primary care or pharmacy-based providers match the support offered by specialized opioid treatment programs (OTPs)?
- Without addiction-specific training, care quality may suffer.
- There’s a moral obligation to ensure that all patients receive adequate monitoring and support, regardless of setting.
3. ⚖️ Health Equity and Disparities
Dilemma: Will modernization bridge or widen access gaps across communities?
- Marginalized populations could be left behind if reforms favor well-resourced areas.
- Cultural competence and equity must be central to implementation efforts.
4. 🔓 Autonomy vs. Provider Oversight
Dilemma: Should patients fully control their treatment, or should providers maintain limits for safety?
- Overly paternalistic restrictions can undermine patient dignity.
- But unrestricted access early in treatment might increase relapse risk.
5. 🔄 Changing the Role of Methadone Clinics
Dilemma: What happens to traditional OTPs and their staff in a decentralized model?
- Clinics may face job losses or funding cuts.
- Ethical modernization includes workforce transition planning and sustaining essential services.
6. 🧾 Commercialization and Profit Motives
Dilemma: Could pharmacy-based treatment prioritize profit over care?
- Without strong regulation, for-profit systems might underemphasize counseling or patient relationships.
- Training, accountability, and oversight are critical in non-clinical settings.
🧠 Summary Table of Key Ethical Tensions
| Ethical Issue | Central Question |
|---|---|
| Safety vs. Access | Can we expand availability without increasing harm? |
| Care Quality vs. Convenience | Will patients get the support they need outside OTPs? |
| Equity vs. Inequality | Are we widening or closing treatment gaps across populations? |
| Autonomy vs. Oversight | How much control should patients have over their treatment? |
| Innovation vs. Tradition | What is the fate of OTPs and their staff? |
| Profit vs. Patient-Centered Care | Will modernization protect patient interests in all settings? |
In summary, as we embrace methadone modernization, we must uphold both innovation and ethics. A truly modern system empowers recovery without sacrificing safety, fairness, or the therapeutic relationships at its core. Thoughtful policies, inclusive planning, and community voices are key to striking this balance.
Empowering Recovery: How Methadone Modernization Supports Self-Management and Autonomy
Methadone modernization—by increasing access, flexibility, and integration into community settings—creates new opportunities for individuals in recovery to take greater ownership over their treatment and long-term stability. It empowers patients to apply practical self-management strategies that support autonomy, resilience, and engagement in recovery.
🧠 Self-Management Strategies Enabled by Methadone Modernization
1. ✅ Daily Routine Planning with Take-Home Dosing
Modernization allows for more flexible take-home methadone schedules, reducing the need for daily clinic visits.
Strategy:
- Create and maintain a structured daily routine around medication, meals, work, and self-care.
- Use reminders (phone alarms, calendars) to stay on schedule with dosing.
- Incorporate morning or evening rituals around dosing for consistency.
📍 Benefit: Builds routine and accountability, reduces disruption to work and family life.
2. 📊 Symptom and Mood Tracking
With less direct supervision, patients can monitor their own progress and share updates with care teams.
Strategy:
- Use a journal or app to log cravings, mood, energy levels, sleep, and triggers.
- Track how methadone dosage correlates with stability or challenges.
📍 Benefit: Encourages self-awareness and timely self-advocacy if dose adjustments or counseling are needed.
3. 🧘 Mindfulness and Stress-Reduction Practices
Increased autonomy can bring more pressure. Integrating stress-reduction supports emotional resilience.
Strategy:
- Practice breathing exercises, grounding techniques, or guided meditations daily.
- Attend peer-led mindfulness or trauma-informed yoga sessions.
📍 Benefit: Enhances emotional regulation, reduces relapse risk, and supports mental wellness.
4. 💬 Peer Accountability and Support Networks
Modernization often includes integrating peer recovery into non-clinical settings such as pharmacies or telehealth.
Strategy:
- Join a recovery group (online or in person) for shared experiences and motivation.
- Set regular check-ins with a peer mentor or recovery coach.
📍 Benefit: Builds community and maintains motivation outside clinic walls.
5. 🧾 Health and Wellness Goal Setting
With fewer logistical barriers (e.g., daily clinic travel), patients can set personal wellness goals.
Strategy:
- Create SMART goals (Specific, Measurable, Achievable, Relevant, Time-bound) related to health, relationships, or employment.
- Track weekly progress and celebrate milestones.
📍 Benefit: Encourages purpose and direction in recovery beyond medication.
6. 🧠 Crisis Planning and Trigger Management
Modernized care emphasizes personalized relapse prevention, empowering people to take the lead.
Strategy:
- Develop and update a written recovery plan that includes triggers, coping tools, and emergency contacts.
- Review it monthly with a counselor or peer.
📍 Benefit: Prepares patients to respond constructively to stress and setbacks.
🔄 Summary Table: Self-Management Benefits of Methadone Modernization
| Strategy | Enabled by Modernization | Supports |
|---|---|---|
| Routine and dose planning | Flexible take-home schedules | Independence, structure |
| Mood and symptom tracking | Less frequent clinic visits | Self-awareness, dose management |
| Stress reduction tools | Reduced time burden enables wellness | Emotional regulation, relapse prevention |
| Peer and community connection | Integration into pharmacies/telehealth | Belonging, accountability |
| Goal setting | More time and flexibility | Personal growth, motivation |
| Crisis planning | Focus on individualized care | Safety, proactive recovery management |
How Methadone Modernization Empowers Families to Support Recovery
Methadone modernization offers families new and practical ways to support their loved ones by reducing treatment barriers, normalizing care, and enabling greater involvement beyond traditional clinic settings. These changes encourage families to take more active, informed, and compassionate roles, helping to foster stability and strengthen recovery at home.
💡 6 Family Support Strategies Enabled by Modernized Methadone Care
🏠 1. Support Home-Based Routine
Strategy: Help build a daily structure around medication, meals, rest, and responsibilities.
- Use calendars or phone reminders.
- Create a calm, substance-free home.
- Respect autonomy and celebrate recovery goals.
📍 Benefit: Encourages trust, consistency, and treatment engagement.
📚 2. Learn and Advocate for Access
Strategy: Stay informed about new care models—like pharmacy pick-ups or telehealth—and help navigate them.
- Attend family education sessions.
- Support stigma-free treatment choices.
📍 Benefit: Empowers families to advocate and reduce stigma.
💬 3. Communicate and Plan Together
Strategy: Join your loved one in treatment planning and relapse prevention.
- Attend telehealth check-ins or family sessions.
- Help update crisis and coping plans.
📍 Benefit: Builds openness, shared responsibility, and emotional support.
🚗 4. Reduce Logistical Barriers
Strategy: Offer support with scheduling, tech use, or transportation.
- Provide rides or help with telehealth tools.
📍 Benefit: Prevents missed appointments and reinforces reliability.
💡 5. Promote Healthy Coping at Home
Strategy: Join in healthy habits like walking, meal prep, or mindfulness.
- Watch for stress and offer nonjudgmental support.
📍 Benefit: Encourages emotional stability and bonding.
🧠 6. Reduce Stigma and Build Dignity
Strategy: Normalize methadone treatment in conversation and community.
- Challenge outdated views.
- Use people-first language (e.g., “person in recovery”).
📍 Benefit: Builds a recovery-friendly, respectful environment.
📋 Summary: Family Empowerment Through Modernization
| Family Strategy | Enabled by | Key Benefit |
|---|---|---|
| Home routine support | Take-home dosing flexibility | Routine and autonomy |
| Learn and advocate | Pharmacy & primary care integration | Choice and access |
| Communicate and co-plan | Decentralized & telehealth care | Stronger relationships |
| Help with logistics | Reduced clinic dependency | Fewer barriers to care |
| Encourage wellness at home | Flexible scheduling | Health, bonding, stress management |
| Reduce stigma | Expanded public understanding of MAT | Acceptance and dignity |
Methadone Modernization: Expanding Community-Based Strategies for Opioid Recovery
Methadone modernization opens the door for more inclusive, flexible, and widespread community-based strategies to support recovery from opioid use disorder (OUD). By shifting methadone treatment beyond tightly regulated clinics and into community settings, these strategies can broaden access, reduce stigma, and offer more comprehensive care in people’s everyday environments.
🏘️ Community Resource Strategies Enabled by Methadone Modernization
1. 🏥 Pharmacy-Based Methadone Dispensing
Strategy: Equip local pharmacies to dispense methadone, reducing dependence on specialized clinics.
- Offers convenience and normalization within everyday health settings.
- Builds relationships between patients and local pharmacists.
- May reduce stigma by integrating care into routine health stops.
📍 Impact: Increases access in rural and underserved areas and reduces transportation barriers.
2. 🧑⚕️ Primary Care Integration
Strategy: Train and authorize primary care providers (PCPs) to prescribe and manage methadone treatment.
- Patients can receive addiction care alongside other health services.
- Supports continuity of care, especially for those with co-occurring medical conditions.
📍 Impact: Makes methadone part of holistic community-based care and helps engage people earlier in treatment.
3. 🚐 Mobile Methadone Clinics
Strategy: Deploy mobile units to provide methadone and related services in hard-to-reach areas.
- Brings care to homeless encampments, rural towns, and underserved urban areas.
- Can offer other services like counseling, HIV/HCV testing, or harm reduction tools.
📍 Impact: Lowers barriers for those with unstable housing or limited mobility.
4. 🧑🤝🧑 Peer Recovery Support Networks
Strategy: Expand peer-led programs through recovery community organizations (RCOs), shelters, or outreach hubs.
- Peer coaches can help with methadone adherence, navigating pharmacy models, and relapse prevention.
- Create emotional support systems beyond clinical walls.
📍 Impact: Encourages engagement and trust, especially for people with prior negative treatment experiences.
5. 🏠 Recovery Housing and Transportation Support
Strategy: Pair methadone access with safe housing and transit options.
- Local nonprofits or health departments can partner to fund recovery homes near expanded methadone services.
- Provide transportation vouchers or a mobile app for scheduling pharmacy trips.
📍 Impact: Enhances treatment adherence and stability.
6. 🧾 Legal and Reentry Services
Strategy: Integrate methadone access into community-based reentry programs for justice-involved individuals.
- Provide bridge prescriptions or direct referral to pharmacy-based programs post-release.
- Offer legal navigation services alongside recovery support.
📍 Impact: Reduces risk of relapse and overdose after incarceration.
7. 🧘 Community Wellness Programs
Strategy: Encourage collaboration between methadone providers and local wellness centers or nonprofits.
- Offer access to therapy, mindfulness, group fitness, nutrition support, and skill-building.
- Help shift recovery from a medicalized experience to a community-embedded lifestyle.
📍 Impact: Supports long-term recovery and reduces isolation.
📋 Summary Table: Community Strategies from Methadone Modernization
| Strategy | Setting | Benefit |
|---|---|---|
| Pharmacy-based dispensing | Pharmacies, retail clinics | Normalizes care, improves convenience and access |
| Primary care integration | Health centers, clinics | Provides holistic care, reduces stigma |
| Mobile clinics | Streets, rural areas | Reaches marginalized and hard-to-access populations |
| Peer support programs | RCOs, shelters, libraries | Builds trust, offers guidance and lived experience |
| Recovery housing + transport | Nonprofits, city programs | Improves stability and adherence |
| Reentry and legal services | Justice and health orgs | Supports justice-involved individuals’ recovery |
| Community wellness partnerships | Parks, YMCAs, rec centers | Encourages healthy routines and social integration |
Frequently Asked Questions
Here are some common questions:
Question: Provide a self-management worksheet tailored to methadone patients or a planner template for daily routine and wellness tracking.
Answer: Self-management worksheet and daily wellness planner tailored for people in methadone treatment. It’s designed to support structure, medication adherence, and holistic recovery (physical, emotional, social). You can use this as a printable PDF, a digital fillable file, or even adapt it into a workbook format.
📘 Methadone Treatment Daily Wellness Planner
Supporting Your Recovery, One Day at a Time
🗓️ Today’s Date: ___________
💊 Medication Tracker
| Medication | Time | Taken (✔) | Notes |
|---|---|---|---|
| Methadone | ____ | ☐ | |
| Other (e.g., vitamins, psych meds) | ____ | ☐ |
🧠 Morning Check-In (Mental & Emotional Health)
- Mood (circle): 😊 🙂 😐 😟 😢 😠
- Energy level (1–10): _____
- One word to describe how I feel: ______________
- My intention for today: ___________________________________
🏃 Physical Wellness Goals
- ☐ 10+ minutes of movement (walk, stretch, etc.)
- ☐ Healthy meal(s)
- ☐ Hydration (goal: ___ cups)
- ☐ Sleep plan tonight: ___________________________
🧘 Recovery Activities
| Activity | Time | Completed (✔) |
|---|---|---|
| Support group / peer call | ____ | ☐ |
| Journaling or reflection | ____ | ☐ |
| Therapy / Counseling | ____ | ☐ |
| Harm reduction plan review | ____ | ☐ |
👥 Social Support / Contacts Today
- Did I talk to or check in with someone supportive today?
☐ Yes ☐ No
If yes, who? _____________________________
If not, who can I reach out to? ________________________
📚 Appointments or Tasks
| Task/Appointment | Time | Done (✔) |
|---|---|---|
📝 Evening Reflection
- What went well today? _____________________________________
- What was difficult? ________________________________________
- Did I stick to my medication and wellness plan? ☐ Yes ☐ No
If not, why: ______________________________________________ - What can I do differently tomorrow? _________________________
🔒 Affirmation of the Day
“I am committed to my recovery and deserve health, peace, and purpose.”
Question: Provide a family discussion guide tailored to methadone modernization and recovery.
Answer: Family Discussion Guide tailored to support loved ones receiving methadone as part of a modernized recovery approach. It’s designed to build trust, reduce stigma, and create open, practical conversations at home. This guide supports families through changes such as take-home dosing, pharmacy-based access, and more patient-centered care.
💬 Family Discussion Guide: Supporting Recovery with Methadone Modernization
🧭 Purpose of This Guide
This guide helps families have open, non-judgmental conversations with loved ones in treatment using modernized methadone access. It offers key questions, conversation starters, and respectful boundaries to encourage healing, understanding, and partnership.
🏠 Section 1: Understanding Methadone in Modern Recovery
Talking Points:
- Methadone is a life-saving, evidence-based medication used to manage opioid use disorder (OUD).
- Modern approaches now allow for take-home doses, pharmacy access, and care outside traditional clinics.
- Recovery is not just about stopping drugs—it’s about building a stable, hopeful life with support.
Questions to Ask:
- “What does methadone help you manage each day?”
- “How does having more flexibility (like take-home dosing or using a pharmacy) help your recovery?”
- “Are there things we can do to support your routine at home?”
🧩 Section 2: Creating a Supportive Home Environment
Supportive Actions:
- Set up a safe, judgment-free space to take medication.
- Respect your loved one’s privacy and independence.
- Be flexible about household routines as they adjust to treatment changes.
Conversation Starters:
- “Would a daily check-in or reminder help, or do you prefer managing it independently?”
- “Is there anything we should know to support you if you feel triggered or overwhelmed?”
- “Are there times when you’d rather have space or silence instead of conversation?”
📆 Section 3: Navigating Schedules, Stress, and Triggers
Support Tips:
- Encourage self-care, sleep, and wellness activities like walks, cooking, or support groups.
- Identify and reduce home-based triggers (e.g., stress, conflict, substance use by others).
- Help plan appointments or transportation if needed—but only if requested.
Ask Gently:
- “Would you like help planning your week, or are you comfortable doing that solo?”
- “Do you want to talk when you’re having a rough day, or do you prefer space?”
- “What coping strategies work best for you when things feel hard?”
🧠 Section 4: Reducing Stigma and Building Trust
Language to Use:
✅ “Medication for recovery.”
✅ “You’re in treatment.”
✅ “You’re taking care of your health.”
🚫 Avoid: “Still using” / “Addict” / “Just replacing one drug with another.”
Conversation Reminders:
- Avoid comparing recovery timelines.
- Don’t ask for proof of “progress.” Trust the process and focus on connection.
- Celebrate small wins—stability, showing up, managing emotions.
🛠️ Section 5: Crisis or Relapse Preparedness
Steps to Discuss in Advance:
- Who to call or notify if there’s a mental health or overdose emergency.
- Where medication is stored and how to respect boundaries around it.
- A calm strategy for handling setbacks or missed doses.
Sample Dialogue:
- “Can we talk about what you’d like us to do if you ever feel unsafe or overwhelmed?”
- “What signs should we look out for that might mean you need extra support?”
📘 Resources for Families
Include these with your guide or post on a family board:
- 📞 SAMHSA National Helpline: 1-800-662-HELP (24/7)
- 🌐 Partnership to End Addiction (drugfree.org)
- 👥 Al-Anon or Nar-Anon: Peer support for families
- 📍 Local peer recovery centers, family counseling, and mobile outreach units
✅ Final Tip: Be a Support, Not a Supervisor
Your loved one’s recovery belongs to them. Your role is to be present, informed, encouraging, and nonjudgmental. Methadone modernization gives them more freedom—your trust and understanding help them use it wisely.
Question: Provide a community action guide, a grant proposal outline, or a local resource directory format.
Answer: Three ready-to-use templates depending on your goal: a Community Action Guide, a Grant Proposal Outline, and a Local Resource Directory Format — all tailored for initiatives related to methadone modernization and community-based recovery support.
✅ 1. Community Action Guide Template
Title: Empowering Recovery: Community Strategies for Methadone Access and Support
I. Introduction
- Purpose of the guide
- Why methadone modernization matters
- Who this guide is for (community leaders, health workers, advocates)
II. Understanding Methadone Modernization
- Key policy updates (e.g., take-home doses, pharmacy dispensing)
- Benefits to individuals and communities
III. Identify Local Needs
- Assess transportation, stigma, and provider access
- Engage stakeholders (residents, providers, peer support groups)
IV. Develop Community Strategies
| Strategy | Description | Community Partners | Action Steps |
|---|---|---|---|
| Pharmacy Access | Engage local pharmacies | Pharmacy boards, DOH | Meet, train, pilot |
| Mobile Clinics | Outreach in underserved areas | Nonprofits, EMS | Plan routes, staff |
| Peer Networks | Train peer coaches | RCOs, shelters | Recruit, certify |
V. Advocacy & Policy Engagement
- Contacting local/state policymakers
- Hosting forums or town halls
- Sharing lived experience stories
VI. Evaluation & Sustainability
- Tracking access and outcomes
- Building long-term funding partnerships
💰 2. Grant Proposal Outline
Title: Expanding Community-Based Methadone Access through Peer Support and Integrated Services
I. Executive Summary
- Brief statement of problem
- Summary of solution
- Funding requested
II. Statement of Need
- Local OUD statistics
- Treatment access gaps
- Relevance of methadone modernization
III. Project Description
- Goals and objectives
- Activities: mobile clinic, peer training, pharmacy partnerships
- Timeline
- Target population
IV. Organizational Background
- Mission
- Relevant experience
- Key staff and partners
V. Evaluation Plan
- What metrics will you track (e.g., retention, overdose prevention)?
- Tools and methods
VI. Budget & Justification
- Staff, training, supplies, transportation
- Any in-kind or matching support
VII. Sustainability
- Future funding strategies
- Community partnerships
VIII. Appendices
- Letters of support
- Organizational chart
- IRS nonprofit letter (if applicable)
📇 3. Local Resource Directory Format
Title: Community Recovery Resource Directory: Methadone & Beyond
| Yoga, nutrition, and social events | Organization | Contact | Services Offered | Eligibility | Notes |
|---|---|---|---|---|---|
| Methadone Dispensing | CVS Pharmacy | 555-123-4567 | Daily and take-home doses | Adults with OUD diagnosis | Call ahead |
| Primary Care Providers | City Health Clinic | cityhealth.org | MAT, physical care, referrals | Uninsured welcome | Sliding scale |
| Peer Recovery Support | RiseUp RCO | 555-987-6543 | Peer coaching, groups | All stages of recovery | LGBTQ+ friendly |
| Recovery Housing | New Start Home | newstart.org | Sober housing + methadone support | Must be 30+ days sober | Application required |
| Legal Help | Justice & Health Project | 555-555-5555 | Reentry planning, expungement | Formerly incarcerated | Walk-ins Tues/Fri |
| Wellness Programs | YMCA Recovery Fitness | localymca.org | Yoga, nutrition, social events | Open to recovery community | Low-cost membership |
Conclusion
Methadone modernization represents a critical step toward making opioid use disorder treatment more accessible, flexible, and person-centered. While it offers significant benefits—such as increased autonomy and reduced stigma—it also presents challenges, including safety concerns, ethical dilemmas around care oversight, and the need for equitable implementation. Success depends on empowering individuals through self-management strategies, engaging families as active recovery partners, and mobilizing community resources to provide consistent, supportive care. When thoughtfully implemented, methadone modernization can help transform recovery into a more inclusive and sustainable journey.
Video: 4 HUGE Changes in Methadone Treatment You Need to Know About