In the fentanyl era, methadone clinics serve as vital lifelines for individuals battling opioid addiction, yet their efficacy and risks are under heightened scrutiny. A collective effort involving community resources, government strategies, self-management techniques, and family support is imperative to navigate this landscape. By exploring these interconnected elements, we can better understand how methadone clinics are both aiding and potentially exacerbating the challenges of opioid addiction in the face of fentanyl’s heightened dangers.
The Role of Methadone Clinics in the Fentanyl Era: How They Help and Potential Drawbacks
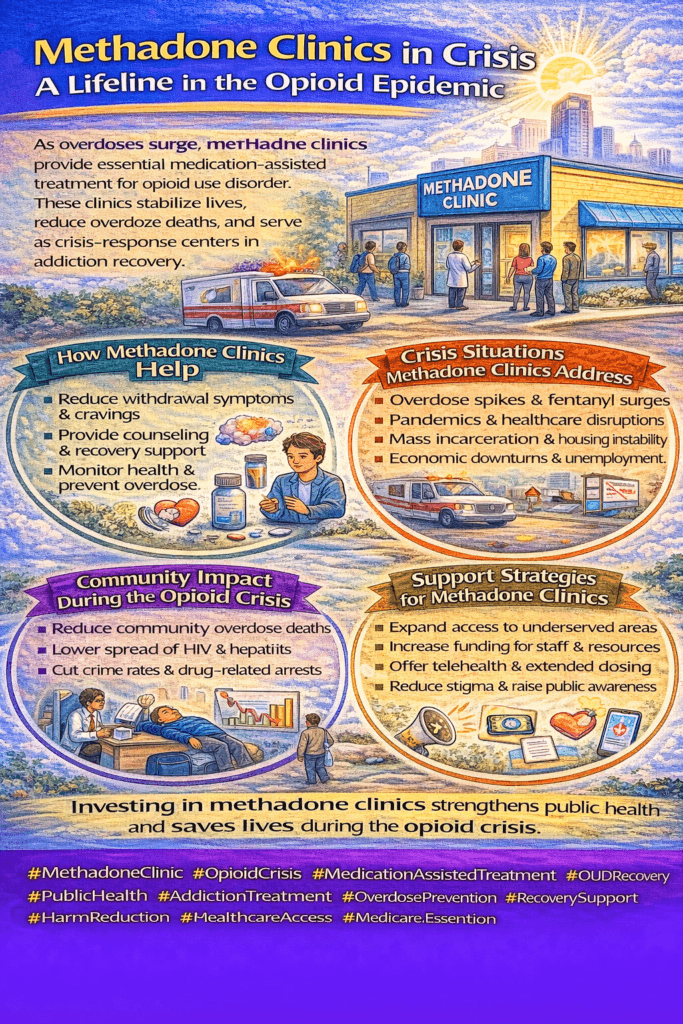
In the face of the opioid crisis, particularly as fentanyl use rises, methadone clinics play an indispensable role in supporting those struggling with opioid addiction. Here’s a look at how these clinics contribute to recovery and the challenges they face.
How Methadone Clinics Help
- Medication-Assisted Treatment (MAT): Methadone clinics provide methadone, a well-established medication that reduces opioid cravings and withdrawal symptoms. This allows individuals to stabilize their lives, manage daily responsibilities, and fully engage in their recovery journey.
- Reduction of Illicit Opioid Use: Research shows that methadone treatment effectively reduces the need for illicit opioids, including powerful substances like fentanyl. By offering a regulated and safer alternative, clinics help mitigate the risks associated with unregulated drug use.
- Supervised Administration: Many clinics administer methadone doses under medical supervision, ensuring patients receive the correct amount while reducing the risk of diversion or misuse. This structure enhances patient safety and builds trust in the recovery process.
- Comprehensive Care: Methadone clinics often go beyond medication, providing essential services such as counseling, medical support, and social resources. This holistic approach helps individuals address broader issues related to their addiction, such as mental health concerns and socioeconomic challenges.
Potential Drawbacks and Challenges
- Risk of Dependency: While methadone is a vital part of MAT, it is also an opioid and can lead to physical dependence. Some individuals may require methadone for an extended period, and tapering off can be difficult. Transitioning to an opioid-free life may require additional support, counseling, and sometimes long-term planning.
- Stigma and Discrimination: Methadone treatment can carry a stigma, often stemming from misunderstandings about MAT and addiction. This societal stigma can lead to discrimination, causing some individuals to avoid seeking help or feel alienated in their recovery journey.
- Safety Concerns: Methadone requires careful dosing and management due to its narrow therapeutic window, meaning the difference between a therapeutic dose and an overdose is small. Especially during the fentanyl era, the risks increase if methadone is misused or combined with other substances. Clinics must ensure safe administration practices and educate patients on potential risks.
- Limited Access: Methadone clinics are not available everywhere, with significant access gaps in rural and underserved communities. This geographic barrier means many individuals cannot access this life-saving treatment, which is essential in areas deeply affected by the opioid crisis.
Methadone clinics are vital in combating opioid addiction, including the challenges posed by the widespread presence of fentanyl. However, it is equally important to address the potential harms and barriers, such as dependency, stigma, safety concerns, and access limitations. By improving education, expanding access, and tackling stigma, communities can strengthen the impact of methadone clinics and promote a path toward recovery that is accessible, safe, and respectful for all who seek help.
Community Strategies for Increasing Access to Methadone Clinics in the Fentanyl Era
In the fight against opioid addiction, especially during the ongoing fentanyl crisis, methadone clinics offer a vital lifeline. However, increasing access to these clinics and ensuring effective support requires a coordinated, community-centered approach. Here are several impactful strategies communities can implement to expand access and better manage opioid addiction.
1. Increase Awareness and Education
One of the most significant barriers to methadone treatment is stigma and misinformation. Community organizations can tackle this by conducting outreach campaigns that educate the public on the proven benefits of methadone for opioid addiction. These campaigns can dispel myths, explain how methadone works, and show how it helps individuals stabilize their lives.
2. Expand Funding and Support
Sustainable funding is critical for methadone clinics. Communities can work together to advocate for government grants, seek private donations, and build collaborations with healthcare organizations. Increased financial support enables clinics to expand services, improve accessibility, and reach more needy people.
3. Reduce Barriers to Access
Logistical challenges like transportation, work schedules, and childcare needs can prevent people from accessing methadone treatment. Solutions like transportation vouchers, flexible clinic hours, and on-site childcare can make clinics more accessible. Removing these practical barriers helps individuals prioritize their treatment.
4. Build Community Partnerships
Forging partnerships between methadone clinics and other local organizations — including primary care clinics, mental health services, and social services — provides a comprehensive support network. This approach ensures that individuals have access to all necessary services, from mental health care to housing support, increasing the chances of long-term recovery.
5. Establish Peer Support Programs
Integrating peer support into methadone clinics offers valuable guidance from individuals who have firsthand experience with recovery. Peer mentors provide emotional support, reduce stigma, and inspire others to engage actively in their recovery journeys. Many people find it reassuring to connect with others who understand their challenges.
6. Expand Telemedicine Services
Telemedicine is a powerful tool to increase methadone access in rural or underserved areas. Telemedicine allows for remote consultations, counseling, and medication management, making it easier for those without nearby clinics to receive consistent care. This solution is particularly effective for people with limited mobility or facing transportation challenges.
7. Community-Based Harm Reduction Initiatives
Supporting harm reduction efforts, such as naloxone distribution, syringe exchange services, and safe injection sites, can prevent overdoses and reduce the spread of infectious diseases. By integrating harm reduction services, communities can keep individuals safer while offering methadone as a pathway to stability and recovery.
8. Advocacy and Policy Change
Advocacy is crucial to expanding methadone access. Communities can push for policy changes that support methadone clinic growth, secure insurance coverage, and reduce regulatory hurdles. By promoting evidence-based policies, community leaders and members can help build a treatment framework that is accessible, equitable, and focused on long-term recovery.
By embracing these strategies, communities can make methadone clinics more accessible and create a support system that effectively addresses opioid addiction, even amid the fentanyl crisis. With education, practical resources, and collaboration, we can build communities that not only support recovery but also actively work to prevent further addiction and overdose tragedies.
Government Strategies to Increase Access to Methadone Clinics in the Fentanyl Crisis
In the era of potent synthetic opioids like fentanyl, addressing opioid addiction has become more urgent than ever. Governments play a pivotal role in making methadone treatment more accessible, effective, and widespread. Here are key strategies that policymakers can implement to expand access to methadone clinics and support individuals battling opioid addiction.
1. Funding and Resource Allocation
Allocating adequate funding is essential for establishing and sustaining methadone clinics. This includes not only funding for clinic operations but also for training healthcare staff, developing infrastructure, and researching the best practices in addiction treatment. Government support can help clinics reach underserved areas, maintain high-quality services, and adapt to changing community needs.
2. Policy and Regulatory Support
Governments can streamline the establishment of methadone clinics by reducing bureaucratic barriers and ensuring compliance with evidence-based treatment standards. Policies that support easy licensing, quick accreditation, and flexible regulations make it easier to set up new clinics and reduce waiting times for patients seeking treatment.
3. Workforce Development
A skilled workforce is essential for the success of methadone clinics. Investing in addiction medicine training and creating incentives such as scholarships, loan forgiveness, and continuing education programs can help attract and retain healthcare providers specialized in addiction treatment. This strategy ensures that clinics have qualified staff to offer comprehensive care.
4. Integration with Healthcare Systems
Promoting collaboration between methadone clinics and other healthcare providers helps ensure that patients receive comprehensive, coordinated care. By integrating methadone clinics with primary care, mental health services, and social services, governments can help individuals manage addiction while also addressing co-occurring health issues, housing, and employment needs.
5. Telemedicine and Technology Expansion
In rural or underserved areas, telemedicine is a critical tool for expanding access to methadone treatment. Government support for telemedicine infrastructure, reimbursement for virtual visits, and regulatory frameworks that facilitate telehealth services can enable individuals in remote locations to receive timely and consistent care.
6. Data Collection and Monitoring
Data-driven policies improve treatment quality and outcomes. Governments can establish systems for collecting data on opioid use, treatment success rates, and patient satisfaction to refine addiction treatment programs continuously. Using standardized data collection tools and electronic health records, policymakers can make informed decisions to improve services.
7. Public Awareness Campaigns
Public awareness campaigns are essential to reduce the stigma associated with methadone treatment and opioid addiction. By promoting methadone’s effectiveness and educating communities, governments can encourage more individuals to seek treatment without fear of judgment. Campaigns can include media outreach, community events, and targeted messages for high-risk populations.
8. Collaboration with Stakeholders
Addressing opioid addiction requires a collaborative approach. Governments can bring together healthcare providers, community organizations, law enforcement, advocacy groups, and people affected by addiction to develop comprehensive strategies. Stakeholder meetings, task forces, and community input sessions help ensure that diverse perspectives are considered in policymaking.
By implementing these strategies, governments can make methadone treatment more accessible and effective, even amidst the challenges of the fentanyl crisis. Through funding, regulatory support, workforce development, and collaborative efforts, policymakers can ensure that individuals with opioid addiction receive the care they need to manage their addiction and reclaim their lives.
Self-Management Strategies for Methadone Treatment Success in the Fentanyl Era
In the current fentanyl crisis, self-management strategies are essential for individuals on methadone treatment for opioid addiction. Methadone treatment offers significant help in stabilizing opioid cravings and supporting recovery, but self-management practices can maximize its effectiveness. Here are key strategies for navigating methadone treatment successfully.
1. Medication Adherence
Sticking to the prescribed methadone dosage and following your treatment plan is vital. Methadone works best when taken consistently, as it helps keep opioid cravings and withdrawal symptoms under control. Remember to communicate with your healthcare provider if you have any issues with your dosage or side effects.
2. Education and Information
Educate yourself about how methadone works, including its benefits, potential side effects, and safety precautions. Being informed empowers you to actively participate in your treatment and make decisions that align with your recovery goals. Don’t hesitate to ask your healthcare provider questions.
3. Adopt a Healthy Lifestyle
A balanced lifestyle that includes healthy eating, regular exercise, stress management, and sufficient sleep supports recovery. Activities like mindfulness, meditation, and physical exercise boost your physical health and improve mental resilience, helping you navigate daily stressors without relying on substances.
4. Avoid Triggers and High-Risk Situations
Understanding your triggers—such as specific places, people, or situations associated with past drug use—is essential for relapse prevention. Take proactive steps to avoid these triggers and develop coping strategies for moments when cravings arise.
5. Engage in Supportive Activities
Filling your time with positive, fulfilling activities can reinforce your commitment to recovery. This might include picking up a new hobby, volunteering, joining a support group, or spending time with supportive friends and family. These activities help shift your focus and offer meaningful connections.
6. Participate in Counseling and Therapy
Therapy can address the root causes of addiction, provide you with coping skills, and offer ongoing support. Whether in individual counseling, group therapy, or family therapy, regular sessions benefit emotional processing and long-term recovery.
7. Regular Monitoring and Self-Reflection
Tracking your treatment progress can reveal important insights. Regularly check in with yourself regarding your mood, any changes in symptoms, and your overall well-being. If you notice any challenges or setbacks, share them with your healthcare provider so your treatment plan can be adjusted accordingly.
8. Develop a Relapse Prevention Plan
Work with your provider to create a plan that addresses potential relapse situations. This plan should include strategies for managing cravings, dealing with stress, and knowing when and how to seek help. Having a solid plan gives you tools to rely on during difficult times.
9. Connect with Peer Support
Building a support network of peers on the journey to recovery can provide invaluable encouragement and accountability. Support groups can offer understanding and help you stay committed to your goals.
10. Attend Regular Check-ins
Staying in close communication with your healthcare team is essential for successful treatment. Regular appointments offer a chance to discuss progress, address any concerns, and make adjustments to your treatment plan as necessary. Don’t hesitate to reach out between appointments if challenges arise.
By implementing these self-management strategies, you can take an active role in your recovery, maximize the benefits of methadone treatment, and work toward a stable, fulfilling life. Managing opioid addiction, particularly in the fentanyl era, is challenging but achievable with the proper support, knowledge, and commitment. Every positive step strengthens your foundation for long-term recovery and overall well-being.
Family Support Strategies for Managing Opioid Addiction Through Methadone Treatment in the Fentanyl Era
Family support is a cornerstone of success for individuals undergoing methadone treatment for opioid addiction, especially during the fentanyl crisis. Opioid addiction can be a complex and challenging disease, and having the right support system can make a world of difference in a loved one’s recovery journey. Here are some family support strategies to help individuals navigate the challenges of opioid addiction and methadone treatment:
1. Education and Awareness
The first step in providing practical support is understanding the disease. Educate family members about opioid addiction, methadone treatment, and the specific challenges presented by the fentanyl epidemic. By learning about how methadone works to reduce cravings and withdrawal symptoms, family members can better understand the recovery process and the role they can play in supporting their loved ones.
2. Open Communication
Encourage open, honest communication within the family. Addiction can often create feelings of shame and isolation, so family members need to create a safe, non-judgmental space where the person undergoing treatment can express their feelings and experiences. Listening with empathy and without criticism helps build trust and strengthen recovery.
3. Participation in Treatment
Support the individual by becoming actively involved in their treatment journey. Attend counseling sessions, medication appointments, and support group meetings together. Participating in treatment as a family can provide emotional support and reinforce the importance of commitment to recovery. Family members can also help with practical needs, such as transportation or childcare, making it easier to attend appointments.
4. Setting Boundaries
Setting healthy, clear boundaries is crucial for both the person in recovery and the family. While it’s essential to offer support, enabling behaviors—such as financially supporting substance use or excusing missed appointments—can undermine recovery efforts. Establish boundaries that encourage accountability while showing care and commitment to recovery goals.
5. Empathy and Support
Offer empathy and emotional support. Let your loved one know you understand their struggles and care deeply about their recovery. Feelings of guilt and shame often accompany addiction, so validating their experiences can be incredibly reassuring. Remind them they are not alone and that recovery is a journey that takes time and patience.
6. Self-Care for Family Members
Supporting someone through addiction can be emotionally taxing, so it’s crucial for family members to prioritize their own mental and emotional health. Encourage family members to make time for self-care, whether by joining support groups, seeking professional counseling, or simply engaging in stress-reducing activities such as exercise or meditation. When family members care for themselves, they are better equipped to support their loved ones.
7. Crisis Intervention Planning
Addiction recovery is rarely a straight path, and setbacks may occur. Develop a crisis intervention plan with the individual and other family members to address potential challenges, such as relapses or emotional crises. A plan ensures everyone is on the same page and knows how to respond effectively in difficult situations.
8. Education on Harm Reduction
Harm reduction strategies can save lives in moments of crisis. Educate family members about tools like naloxone (an opioid overdose reversal medication), and train them on how to administer it if needed. Carrying naloxone can be a critical step in preventing a fatal overdose, especially given the prevalence of fentanyl in the opioid supply.
9. Celebrating Milestones and Progress
Recovery is a long journey, but celebrating small wins can help maintain motivation. Acknowledge milestones like staying sober for a week, completing a therapy session, or engaging in healthy coping behaviors. These celebrations show appreciation for the effort put into recovery and help build the individual’s confidence in their ability to continue.
10. Seeking Professional Support
Encourage family members to seek professional support as well. Addiction affects the entire family, and counseling or family therapy can provide the tools needed to address interpersonal issues and strengthen relationships. Support groups, such as Al-Anon or Nar-Anon, can also offer a safe environment for family members to share their experiences and receive encouragement from others in similar situations.
By implementing these strategies, families can be instrumental in helping individuals manage opioid addiction through methadone treatment. The fentanyl era presents unique challenges, but with the right education, open communication, and a commitment to recovery, families can provide the support needed to navigate these challenges. A strong family network can foster hope, resilience, and long-term recovery, making all the difference in the journey toward well-being.
Frequently Asked Questions
Here are some common questions:
What is a methadone clinic?
A methadone clinic is a licensed medical facility that provides methadone treatment for individuals with opioid use disorder, along with counseling and recovery support services.
Why are methadone clinics important during the opioid crisis?
They provide life-saving medication that reduces withdrawal, cravings, and overdose risk, serving as a frontline response to rising opioid-related deaths.
How does methadone help people in crisis?
Methadone stabilizes brain chemistry affected by opioid addiction, allowing individuals to function normally without illicit opioid use.
Do methadone clinics only provide medication?
No. They also offer medical monitoring, mental health counseling, peer support, case management, and referrals to housing and employment services.
How do methadone clinics reduce overdose deaths?
By replacing unpredictable street opioids with medically supervised dosing, clinics dramatically lower the risk of fatal overdose.
Are methadone clinics part of public health crisis response?
Yes. They reduce infectious disease transmission, emergency room visits, and criminal justice involvement, easing community-level healthcare strain.
What happens if a community faces a disaster or healthcare disruption?
Clinics adapt with take-home doses, telehealth counseling, and flexible scheduling to maintain continuous access to treatment.
Is methadone treatment long-term?
It can be. Duration is individualized based on patient stability, recovery progress, and medical guidance.
Do methadone clinics help people enter long-term recovery?
Yes. They often serve as the first consistent point of care, connecting patients to broader recovery and social support services.
Are methadone clinics replacing one addiction with another?
No. Methadone is a medically controlled treatment that stabilizes brain function and supports recovery rather than producing intoxication.
Conclusion
Methadone clinics represent a critical component of the response to opioid addiction in the fentanyl era, offering both promise and peril. While these clinics provide essential medication-assisted treatment, their effectiveness depends on the support and collaboration of various stakeholders. Community resources, government strategies, self-management techniques, and family support play pivotal roles in maximizing the benefits of methadone treatment while mitigating its potential harms. By fostering a holistic approach that integrates these elements, we can better address the complex challenges posed by opioid addiction in the face of fentanyl’s lethal presence, ultimately offering hope and healing to individuals and communities affected by this devastating crisis.
Video: