Mental health and drug use are deeply connected, often creating a cycle that’s hard to break. When someone is dealing with both, it can feel like one issue fuels the other, making recovery overwhelming. Many people are unsure about what’s really happening in the brain—how certain substances can trigger new symptoms, intensify existing disorders, or change the way someone thinks, feels, and behaves. That confusion is entirely understandable. Drug use can alter brain chemistry in ways that affect mood, stress responses, and emotional regulation, while mental health symptoms can make substances feel like a quick escape. In this article, the goal is to break down what science currently understands, highlight key warning signs to watch for, and offer clear guidance for anyone who wants a better grasp of how mental health disorders and drug use interact.
How Drug Use Connects to Mental Health Disorders
Drug use can throw the brain out of balance. Some drugs may cause symptoms like anxiety, depression, or even paranoia after just a few uses, while others might make existing mental health problems worse over time. The link between substance use and mental health disorders isn’t always obvious, but it’s definitely stronger than many people realize.
Statistics show that people who use drugs are also more likely to experience mental health issues. According to the National Institute on Drug Abuse, about half of those living with a mental illness will also face substance use problems at some point. I often hear people wonder whether the drugs caused the mental illness or if the person started using them to cope with tough feelings. Honestly, it can go both ways.
The brain’s reward system, stress response, and mood regulators all play a part here. Drugs change how these systems work, sometimes in permanent ways. This means even a short period of heavy use can have lasting effects, especially during the teenage years, when the brain is still developing. If you want specific stats or are curious about the science, the National Institute on Drug Abuse is a great resource worth checking out.
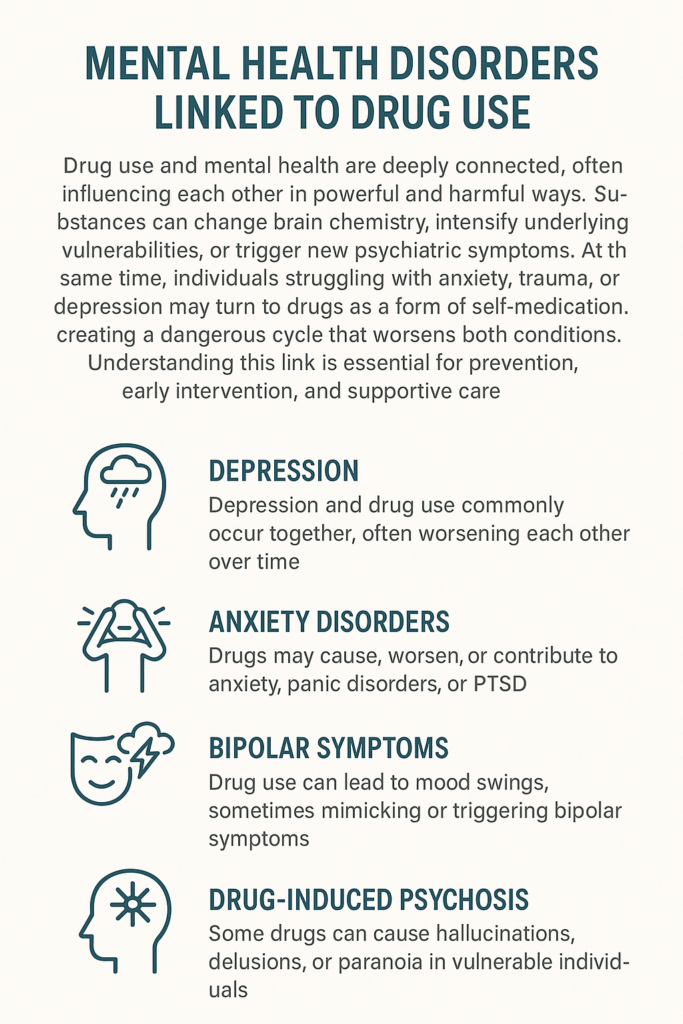
Common Mental Health Disorders Linked to Drug Use
You’ll see several mental health problems frequently tied to substance use. Some of these show up while using drugs, while others may pop up after quitting or cutting back. Here are a few disorders you’ll hear about most often:
- Anxiety Disorders: Drugs like stimulants (think cocaine or meth) can bring on panic attacks, severe anxiety, or ongoing worry—even after the high wears off.
- Depression: Alcohol, opioids, and some sedatives are strongly tied to dips in mood and lingering hopelessness. Sometimes it’s hard to tell if the depression came first or if the substance use tipped things over the edge.
- Psychosis: Substances like cannabis (especially high-potency strains), LSD, or amphetamines can cause hallucinations or delusions. These symptoms may fade as the drug wears off, but they can stick around—especially for people already at risk.
- Bipolar Disorder: For people living with bipolar disorder, drug or alcohol use might trigger more intense mood swings or episodes.
- Post-Traumatic Stress Disorder (PTSD): People with PTSD may turn to substances to dampen flashbacks or bad memories, often ending up stuck in a cycle of relief and rebound.
- Personality Disorders: Certain drugs may increase impulsivity and risk-taking, which can make personality disorders more obvious or severe.
Signs That Drug Use Is Affecting Mental Health
Spotting early warning signs can make a real difference. While everyone’s experience is different, here are some signals that drug use might be taking a toll on mental health:
- Sudden mood changes without an apparent reason
- Feeling anxious, agitated, or hopeless when not using
- Withdrawing from friends and activities that were once enjoyable
- Having trouble with sleep, whether it’s too little or too much
- Hallucinating or seeing things that aren’t really there
- Extreme paranoia or distrust for no apparent reason
- Thoughts about hurting yourself or others
Some changes are subtle. I’ve talked with people who didn’t realize their energy or attitude had changed until someone close to them mentioned it. Noticing these signs early and reaching out for support can really help to turn things around.
Why Drug Use and Mental Health Disorders Often Go Together
No single answer fits every situation, but there are explanations for why substance use and mental health disorders seem to show up side by side:
- Self-Medication: Many people use substances to numb challenging emotions, calm anxiety, or pick up a low mood. The quick relief can make drugs seem like a solution, but over time, they usually make mental health symptoms worse.
- Changes in Brain Chemistry: Drugs upset the brain’s chemical balance, which can trigger new mental health problems or amplify those that already existed.
- Shared Risk Factors: Genetics, stress, trauma, and environment can all raise the chance of dealing with both substance use and certain mental health disorders. If mental health problems run in your family, being around drugs can make things riskier.
- Developmental Timing: Using drugs early in life, while the brain and emotions are still developing, raises the risks for future mental health issues.
Ideas and research in this area keep moving forward, but these are the main threads I’ve seen in mental health discussions and in stories from people living it.
Challenges in Treatment and Recovery
Treating both mental health disorders and substance use at the same time brings special challenges. Here are some obstacles that can show up:
- It’s tough to figure out whether the mental health issue or the drug use came first, and knowing that can help pick the proper treatment.
- Some symptoms might be mistaken for one disorder when they’re actually caused by another, which can slow progress.
- Stigma still holds too many people back from getting help, especially if they worry about being judged for either the drug use or mental health symptoms.
- Finding clinics or therapists truly experienced in “dual diagnosis” (meaning both drug and mental health issues are present) is not always straightforward.
I recommend searching for programs or professionals who clearly have experience treating both substance use and mental health together. Methods such as cognitive-behavioral therapy, medication-assisted treatment, and peer support are often combined for better results. Many communities offer special groups or resources for “co-occurring” disorders, so checking around can be helpful if you’re exploring options.
Practical Steps for Supporting Yourself or Others
If you or someone you care about might be struggling with a mental health disorder connected to drug use, here’s what helps in my experience:
- Reach Out for Help: Start with a trusted doctor, counselor, or mental health hotline. Even a general checkup can steer you to the proper support.
- Share Your Experience: Talking about what’s going on, whether with friends, family, or an online support group, takes the weight off your shoulders and makes it easier to find answers.
- Be Open to Treatment: No single treatment works for everyone, but being open to talk therapy, medication, or group support can give a boost to recovery.
- Plan for Triggers: Knowing what situations, feelings, or places make symptoms worse can help prevent relapse or setbacks later on.
- Take It Step by Step: Small moves, like improving sleep, cutting back on use, or finding healthier coping strategies, lay a stronger foundation for long-term recovery.
The Substance Abuse and Mental Health Services Administration (SAMHSA) has plenty of resources if you’re searching for treatment centers, hotlines, or guides near you.
Everyday Examples and Real-Life Impact
Stories and real-life experiences can help put the facts in perspective. Here are some examples from chats I’ve had and stories I’ve followed:
- A college student tried Adderall to help with exams and had his first panic attack, leading to ongoing anxiety even after quitting.
- Someone with social anxiety started heavy drinking at parties to feel more comfortable, only to find that the depression and stress worsened afterward.
- A friend turned to cannabis to manage trauma nightmares, but noticed their motivation dropped, and mild paranoia kicked in on bad days.
Drug use and mental health often go together for many people, but the stories are unique. If you’ve noticed similar patterns, you’re far from alone, and support is definitely possible.
Frequently Asked Questions
Here are some common questions about mental health disorders and drug use:
Question: Can mental health disorders be cured if someone stops using drugs?
Answer: Sometimes, symptoms fade after stopping drug use, but a lot of people find that mental health disorders still need attention and care, too.
Question: Is it possible to treat both problems at once?
Answer: Yes, treating both substance use and the mental health disorder together usually works best. Integrated care is now being offered in more treatment centers.
Question: Where can I get help?
Answer: Reaching out to a healthcare provider or local mental health service is a significant step. Hotlines and online directories can help point you toward options nearby.
Taking the Next Step
Knowing how closely drug use and mental health connect makes it easier to make good choices and reach out for support sooner. If you or someone you care about is dealing with both, remember there’s no shame in checking in for help, and resources are available.
Learning about the warning signs, possible treatments, and the science linking them can help individuals, parents, and loved ones take action to improve well-being.
Video: Mental Health Disorders Linked to Drug Use