Many mental health clinics struggle to treat adults with opioid use disorder (OUD) due to their inability to conduct dual diagnosis evaluations, hindered by regulatory barriers, limited training, and insufficient resources. Government intervention and community strategies, such as increased funding, enhanced training, and integrated care models, are essential to overcoming these challenges. By fostering collaboration and providing necessary resources, mental health clinics can better address both mental health and substance use disorders, improving overall treatment outcomes.
Why Many Mental Health Clinics Avoid Treating Addiction
Despite the growing need for comprehensive addiction treatment, many outpatient mental health clinics do not offer opioid addiction medications like buprenorphine. This reluctance stems from a complex interplay of regulatory, logistical, financial, and cultural factors. Understanding these barriers is crucial for addressing the gap in care for individuals struggling with opioid use disorder (OUD).
Regulatory Barriers
1. Certification Requirements
Prescribing opioid addiction medications necessitates special certification and training under the Drug Addiction Treatment Act of 2000 (DATA 2000). Many clinics lack providers with this certification, limiting their capacity to offer these essential treatments.
Lack of Training and Expertise
2. Insufficient Training
Mental health professionals often lack the training and experience needed to manage opioid addiction treatment effectively. This includes knowledge of medication-assisted treatment (MAT) and the skills to monitor patients appropriately throughout their recovery journey.
Funding and Reimbursement Issues
3. Financial Disincentives
Offering MAT can be financially burdensome, as insurance companies and Medicaid/Medicare reimbursement rates often do not cover the full cost of these services. This can discourage clinics from providing opioid addiction medications.
Integration Challenges
4. Workflow Coordination
Integrating MAT into existing mental health services requires significant coordination and workflow adjustments, which can be particularly challenging for clinics operating with limited resources and staff.
Stigma and Misconceptions
5. Cultural Attitudes
There remains a stigma surrounding the use of medications for opioid addiction within the medical community. Some providers may believe that MAT merely substitutes one addiction for another or may feel that treating addiction falls outside their scope of practice.
Resource Limitations
6. Prioritization of Services
Many outpatient mental health clinics function with constrained resources and may prioritize other mental health treatments that do not require additional certifications, training, or financial investment.
Regulatory and Licensing Issues
7. State Variability
State regulations governing the provision of MAT can vary widely, with some imposing additional barriers or paperwork that complicate the ability to offer these treatments within mental health settings.
Focus on Traditional Mental Health Services
8. Narrow Treatment Focus
Many mental health clinics primarily concentrate on traditional services such as counseling, therapy, and psychiatric care. This narrow focus can hinder their capacity or willingness to expand into the realm of addiction medicine.
Addressing these barriers requires a multi-faceted approach, including policy changes, increased funding, and education and training programs for healthcare providers. Additionally, efforts to reduce stigma and promote understanding of addiction treatment are essential. By tackling these challenges, outpatient mental health clinics can become better equipped and more willing to offer comprehensive care that includes opioid addiction medications, ultimately improving outcomes for individuals with opioid use disorder.
The Importance of Integrated Treatment for Co-Occurring Opioid Addiction and Mental Illness
A significant percentage of adults with opioid addiction also struggle with mental illness. According to the National Institute on Drug Abuse (NIDA), approximately 30-50% of individuals with opioid use disorder (OUD) have a co-occurring mental health disorder. Similarly, the Substance Abuse and Mental Health Services Administration (SAMHSA) reports that nearly 40% of adults with a substance use disorder (SUD) also have a mental health disorder, with this overlap being especially pronounced in those with opioid addiction. These high rates underscore the necessity of integrated treatment approaches that address both opioid addiction and mental health issues simultaneously.
Understanding Dual Diagnosis
Dual Diagnosis Defined
Dual diagnosis refers to the concurrent assessment and treatment of mental health and substance use disorders. Despite its importance, dual diagnosis is often inadequately integrated into mental health evaluations, facing several challenges and barriers.
Barriers to Integrated Treatment
- Lack of Training and Expertise
Many mental health professionals lack specialized training in substance use disorders. Conversely, addiction specialists may not have training in mental health disorders, creating a gap in comprehensive assessment and treatment. - Siloed Treatment Systems
Historically, mental health and addiction treatment systems have functioned separately, leading to fragmented care. This separation makes it difficult to address both issues concurrently, resulting in suboptimal outcomes. - Stigma and Misunderstanding
The stigma surrounding substance use disorders persists, leading some mental health professionals to underestimate or overlook the complexities of addiction. This can result in inadequate screening and treatment for substance use issues. - Resource Limitations
Many mental health clinics operate with limited resources and often prioritize traditional mental health services. This focus can hinder their ability to provide comprehensive dual-diagnosis care. - Regulatory and Licensing Issues
Different regulations for mental health and addiction treatment can create barriers to integrated care. Providers may face additional administrative burdens when offering dual diagnosis services. - Insurance and Reimbursement Challenges
Inconsistent insurance coverage for integrated care can disincentivize providers from offering comprehensive evaluations. Many plans do not adequately cover dual diagnosis treatment, further complicating access. - Lack of Standardized Screening Tools
While tools for screening co-occurring disorders exist, they are not consistently used across mental health settings, and standardized practices for dual diagnosis are not universally implemented. - Cultural and Systemic Factors
Some treatment settings may focus primarily on one disorder at a time, often prioritizing either mental health issues or substance use disorders over the other.
Steps Toward Improved Integration
To enhance the integration of dual diagnosis into mental health evaluations, several actionable steps can be taken:
- Increase Training and Education
Provide comprehensive training for mental health professionals on assessing and treating substance use disorders to bridge the knowledge gap. - Promote Integrated Care Models
Encourage the development of models that concurrently address mental health and substance use disorders, fostering a more holistic approach. - Enhance Screening Practices
Implement standardized screening tools for dual diagnosis in all mental health settings to ensure comprehensive assessments. - Address Stigma
Actively work to reduce the stigma associated with substance use disorders within the mental health profession, promoting a more accepting environment for integrated care. - Improve Funding and Reimbursement
To incentivize providers, advocate for better insurance coverage and reimbursement policies for dual diagnosis treatment. - Foster Collaboration
Encourage collaboration between mental health and addiction treatment providers to ensure coordinated and holistic care.
Addressing the barriers to integrated treatment for individuals with co-occurring mental health and substance use disorders is essential for improving outcomes. By taking steps to enhance training, promote integrated care models, and reduce stigma, the healthcare system can better identify and treat individuals struggling with both opioid addiction and mental illness, ultimately leading to more effective and compassionate care.
Enhancing the Capacity of Outpatient Mental Health Clinics to Treat Opioid Use Disorder
The opioid crisis continues to impact communities across the country, highlighting the urgent need for effective treatment options. Outpatient mental health clinics play a crucial role in addressing opioid use disorder (OUD), yet many struggle to provide comprehensive care. To increase their capacity, governments can implement several targeted actions that enhance resources, training, and support.
1. Provide Funding and Financial Incentives
- Grants and Subsidies: Offering grants and subsidies to mental health clinics can help cover the costs of training, certification, and the necessary infrastructure to treat OUD. This financial support can ease the burden on clinics looking to expand their services.
- Increased Reimbursement Rates: Raising reimbursement rates for OUD treatment services ensures that clinics can sustainably offer these critical services without jeopardizing their financial stability.
2. Enhance Training and Certification
- Training Programs: It is essential to develop and fund comprehensive training programs for mental health professionals focused on OUD treatment, including medication-assisted treatment (MAT). This training equips clinicians with the knowledge and skills to manage OUD effectively.
- Certification Support: Simplifying the process for clinicians to obtain necessary certifications, such as prescribing buprenorphine and covering the associated costs, can encourage more providers to offer MAT.
3. Integrate Care Models
- Integrated Care Grants: Funding for integrated care models that combine mental health and addiction treatment services can foster a more holistic approach to care. These models enhance coordination among providers and improve patient outcomes.
- Support for Collaborative Care: Encouraging collaborative care models that integrate primary care, mental health, and addiction specialists ensures comprehensive support for individuals with OUD.
4. Regulatory and Policy Changes
- Ease Regulatory Burdens: Streamlining regulatory requirements for mental health clinics to offer MAT and other OUD treatments reduces administrative hurdles and facilitates service delivery.
- Mandate Dual Diagnosis Screening: Requiring mental health clinics to routinely screen for substance use disorders and provide or refer for appropriate treatment ensures that patients receive comprehensive evaluations.
5. Increase Access to Medications
- Medication Access Programs: Funding initiatives to increase access to MAT, including covering medication costs for uninsured or underinsured patients, address a significant barrier to treatment.
- Pharmacy Collaboration: Encouraging partnerships between clinics and pharmacies ensures easy access to medications for OUD and facilitates timely treatment initiation.
6. Public Awareness Campaigns
- Education Initiatives: Launching public awareness campaigns to educate communities about the benefits of integrated mental health and OUD treatment can foster greater understanding and acceptance of these services.
- Reduce Stigma: Efforts to reduce the stigma associated with OUD treatment can encourage more individuals to seek help and support, ultimately improving public health outcomes.
7. Support Research and Data Collection
- Funding Research: Investing in research to identify best practices for integrating OUD treatment into mental health clinics helps to establish effective treatment models.
- Data Sharing: Promoting the sharing of data and best practices among clinics enhances learning and improves treatment outcomes.
8. Community Partnerships
- Collaborate with Local Organizations: Partnering with community organizations can provide comprehensive support services, including housing, employment, and social services for individuals in treatment.
- Peer Support Programs: Funding and promoting peer support programs within mental health clinics offers additional emotional and practical support for individuals with OUD.
9. Expand Telehealth Services
- Telehealth Funding: Funding to expand telehealth services for OUD treatment can improve accessibility, especially in underserved areas where traditional services may be limited.
- Policy Support: Implementing policies that support and reimburse telehealth services for MAT and counseling ensures that remote care options are viable and sustainable.
By taking these proactive measures, governments can significantly increase the capacity of outpatient mental health clinics to treat individuals with opioid use disorder effectively. This not only leads to better health outcomes for patients but also contributes to the broader effort to reduce overdose rates and combat the opioid crisis. Investing in these initiatives will foster a more resilient and responsive mental health system, ultimately benefiting communities nationwide.
Community Strategies to Boost Mental Health Clinics’ Capacity for Treating Opioid Use Disorder
Opioid use disorder (OUD) remains a significant challenge in many communities, necessitating a robust response from mental health outpatient clinics. Community resource strategies can enhance these clinics’ capacity to treat OUD and provide comprehensive care effectively. Here are several actionable strategies communities can implement.
1. Develop Local Training Programs
- Workshops and Seminars: Organizing training sessions for healthcare providers on the latest practices in OUD treatment, including medication-assisted treatment (MAT), ensures that providers are equipped with current knowledge and skills.
- Continuing Education: Partnering with local universities and medical schools to offer continuing education credits for addiction treatment courses encourages ongoing professional development among healthcare providers.
2. Foster Collaborative Networks
- Interagency Collaboration: Creating networks that bring together mental health providers, addiction specialists, primary care doctors, and other stakeholders enables the sharing of resources and best practices, fostering a more integrated approach to care.
- Referral Systems: Developing streamlined referral pathways between mental health clinics and addiction treatment centers ensures that individuals receive comprehensive, coordinated care.
3. Enhance Peer Support Services
- Peer Recovery Coaches: Training and employing individuals with lived experience of addiction as peer recovery coaches within outpatient clinics can provide invaluable support and mentorship to those in treatment.
- Support Groups: Establishing peer-led support groups within the community offers additional avenues for individuals to connect, share experiences, and find encouragement during their recovery journey.
4. Promote Integrated Care Models
- Co-Located Services: Encouraging the co-location of mental health and addiction services within the same facility allows for seamless care integration, improving patient experiences and outcomes.
- Case Management: Implementing case management services can help coordinate care across providers, ensuring that all aspects of a patient’s treatment are addressed holistically.
5. Increase Access to MAT
- Local Pharmacies: Partnering with local pharmacies ensures access to MAT medications and promotes collaborative care between pharmacies and clinics.
- Mobile Clinics: Utilizing mobile health units to provide MAT and other addiction services in underserved areas can significantly increase access to care for those who need it most.
6. Public Awareness and Education Campaigns
- Community Outreach: Conducting outreach programs to educate the community about OUD, available treatments, and the importance of integrated care raises awareness and encourages individuals to seek help.
- Anti-Stigma Campaigns: Launching campaigns to reduce the stigma associated with addiction and mental health treatment can foster a more supportive community environment for those struggling with OUD.
7. Support Funding and Grant Applications
- Grant Writing Assistance: Offering assistance to clinics and community organizations in applying for grants and funding can help expand OUD treatment services and resources.
- Local Funding Initiatives: Advocating for local government and philanthropic funding to expand mental health and addiction services ensures sustained support for these vital programs.
8. Leverage Technology and Telehealth
- Telehealth Platforms: Promoting telehealth for OUD treatment makes it easier for individuals to access care, particularly in remote or underserved areas.
- Digital Tools: Developing and distributing apps and online resources that provide information, support, and treatment options for OUD can empower individuals to take charge of their recovery journey.
9. Build Community Coalitions
- Task Forces: Forming community task forces that include healthcare providers, law enforcement, educators, and community leaders creates a comprehensive approach to addressing the opioid crisis.
- Resource Sharing: Creating platforms for sharing resources, data, and successful strategies among community organizations and clinics enhances collaboration and effectiveness.
10. Improve Social Support Services
- Housing and Employment: Developing programs that provide stable housing and employment support for individuals in recovery addresses critical social determinants of health that influence recovery outcomes.
- Family Support Programs: Providing counseling and support services for families affected by OUD fosters a supportive environment that promotes recovery for individuals and their families.
By implementing these community resource strategies, local stakeholders can significantly enhance the capacity of mental health outpatient clinics to treat opioid use disorder effectively. This collaborative effort not only improves outcomes for individuals struggling with addiction but also fosters a healthier, more resilient community overall. Together, we can address the opioid crisis and support those on the path to recovery.
Community resource strategies.
Community resource strategies can play a vital role in increasing the capacity of mental health outpatient clinics to treat opioid use disorder (OUD). Here are several methods that communities can implement:
- Develop Local Training Programs:
- Workshops and Seminars: Organize training sessions for healthcare providers on the latest practices in OUD treatment, including medication-assisted treatment (MAT).
- Continuing Education: Partner with local universities and medical schools to offer continuing education credits for courses on addiction treatment.
- Foster Collaborative Networks:
- Interagency Collaboration: Create networks that bring together mental health providers, addiction specialists, primary care doctors, and other stakeholders to share resources and best practices.
- Referral Systems: To ensure comprehensive care, develop streamlined referral systems between mental health clinics and addiction treatment centers.
- Enhance Peer Support Services:
- Peer Recovery Coaches: Train and employ individuals with lived experience of addiction to provide peer support and mentoring within outpatient clinics.
- Support Groups: Establish peer-led support groups within the community to offer additional support for individuals in treatment.
- Promote Integrated Care Models:
- Co-Located Services: Encourage the co-location of mental health and addiction services within the same facility to provide integrated care.
- Case Management: Implement case management services to coordinate care across different providers and support holistic treatment approaches.
- Increase Access to MAT:
- Local Pharmacies: Partner with local pharmacies to ensure easy access to MAT medications and promote collaborative care.
- Mobile Clinics: Mobile health units provide MAT and other addiction services in underserved areas.
- Public Awareness and Education Campaigns:
- Community Outreach: Conduct outreach programs to educate the community about OUD, available treatments, and the importance of integrated care.
- Anti-Stigma Campaigns: Launch campaigns to reduce the stigma associated with addiction and mental health treatment, encouraging more individuals to seek help.
- Support Funding and Grant Applications:
- Grant Writing Assistance: Provide support to clinics and community organizations in applying for grants and other funding to expand OUD treatment services.
- Local Funding Initiatives: Advocate for local government and philanthropic funding to support expanding mental health and addiction services.
- Leverage Technology and Telehealth:
- Telehealth Platforms: Promote telehealth for OUD treatment to make it easier for individuals to access care, especially in remote areas.
- Digital Tools: Develop and distribute apps and online resources that provide information, support, and treatment options for OUD.
- Build Community Coalitions:
- Task Forces: Form community task forces that include healthcare providers, law enforcement, educators, and community leaders to address the opioid crisis comprehensively.
- Resource Sharing: Create platforms for sharing resources, data, and successful strategies among community organizations and clinics.
- Improve Social Support Services:
- Housing and Employment: Develop programs that provide stable housing and employment support for individuals in recovery.
- Family Support Programs: These programs offer counseling and support services to families affected by OUD, fostering a supportive environment for recovery.
By implementing these strategies, communities can enhance the capacity of mental health outpatient clinics to effectively treat OUD, providing comprehensive support and improving outcomes for individuals struggling with addiction.
Frequently Asked Questions
Here are some common questions:
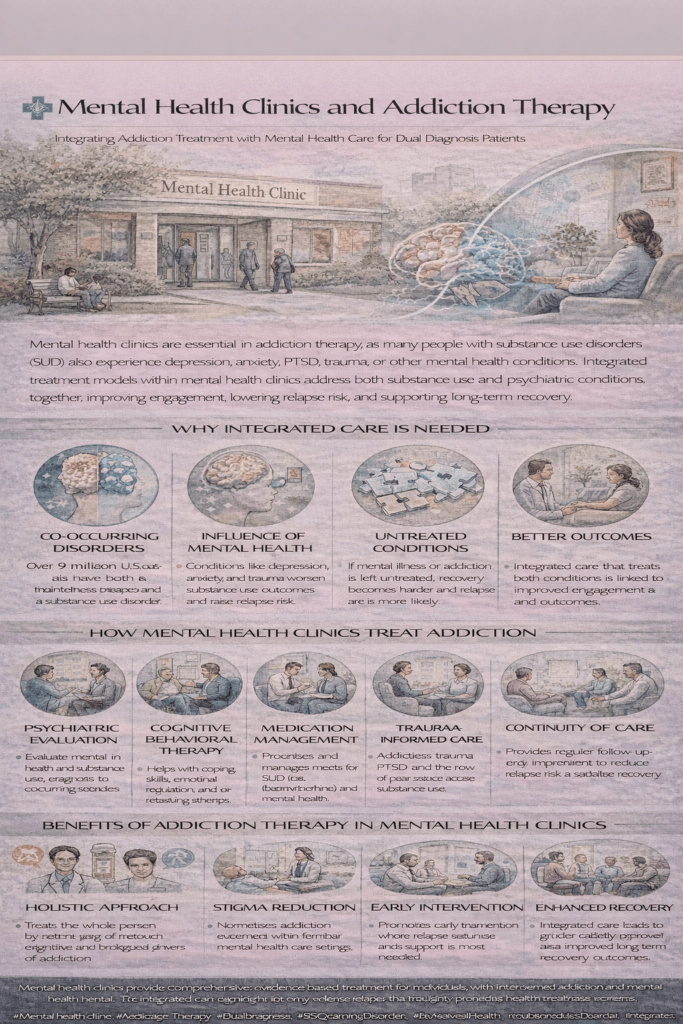
What role do mental health clinics play in addiction treatment?
Mental health clinics address both substance use disorders and co-occurring mental health conditions, recognizing that addiction and mental illness are often interconnected.
What does “co-occurring disorders” or “dual diagnosis” mean?
It refers to having both a mental health condition (such as depression, anxiety, PTSD, or bipolar disorder) and a substance use disorder at the same time.
Why is integrated treatment important?
Treating addiction and mental health conditions together leads to better outcomes than treating each condition separately, reducing relapse risk and improving stability.
What types of therapies are offered in mental health clinics for addiction?
Standard therapies include cognitive behavioral therapy, trauma-informed counseling, motivational interviewing, psychiatric medication management, and medications for substance use disorder when appropriate.
Do mental health clinics prescribe addiction medications?
Many mental health clinics can prescribe and manage medications such as buprenorphine or naltrexone, depending on provider training and clinic resources.
Are mental health clinics only for severe addiction?
No. They treat a wide range of substance use severity, from early problematic use to chronic addiction, especially when mental health symptoms are present.
How do mental health clinics help prevent relapse?
Ongoing monitoring, therapy, medication management, and early intervention help identify rising relapse risk and adjust treatment before crises occur.
Do mental health clinics reduce stigma?
Yes. Providing addiction treatment in behavioral health settings normalizes substance use disorders as medical conditions rather than moral failures.
Is the mental health clinic’s addiction therapy outpatient only?
Most services are outpatient, but clinics often coordinate with inpatient or residential programs when higher levels of care are needed.
Who benefits most from addiction therapy in mental health clinics?
Individuals with depression, anxiety, trauma histories, mood disorders, or repeated relapses benefit greatly from integrated mental health and addiction care.
Conclusion
The current limitations of mental health clinics in treating adults with opioid use disorder (OUD) and conducting dual diagnosis evaluations highlight a critical gap in comprehensive care. Addressing this issue requires concerted efforts through government intervention and the strategic use of community resources. By providing adequate funding, enhancing training programs, promoting integrated care models, and fostering collaborative networks, these initiatives can empower mental health clinics to deliver holistic treatment. Such coordinated efforts are essential for improving health outcomes, reducing the impact of the opioid crisis, and ensuring that individuals with co-occurring disorders receive the comprehensive care they need.
Video: This is why integrated care actually works #AddictionTherapy #MentalWellness #HealthcareMatters