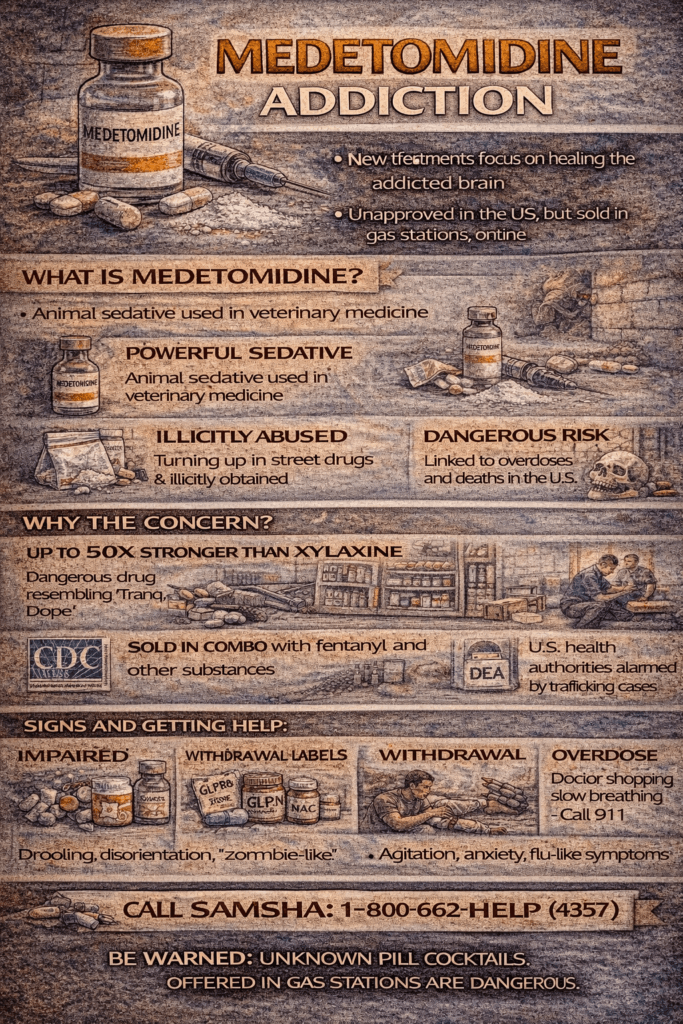
Medetomidine is a powerful veterinary sedative found in illicit drugs, often mixed with fentanyl to intensify and prolong its effects. As an alpha-2 agonist, it causes deep sedation and respiratory depression. Its presence poses serious health risks, especially since standard toxicology screens often miss it, making overdose treatment difficult. Combined with fentanyl, it dramatically increases the risk of fatal overdose and is less responsive to naloxone.
Understanding Medetomidine: A Potent Veterinary Sedative with Rising Public Health Concerns
Medetomidine is a powerful sedative and analgesic used primarily in veterinary medicine. It belongs to the class of alpha-2 adrenergic agonists, which reduce the release of norepinephrine in the brain. This action causes profound sedation, pain relief, and muscle relaxation—making medetomidine highly effective in animal care.
🔬 Key Details About Medetomidine:
- Uses:
- Sedation and pre-anesthetic medication in dogs and cats
- Occasionally used in wildlife capture and immobilization
- Produces dose-dependent sedation and pain relief
- Mechanism of Action:
- Binds to alpha-2 receptors in the central nervous system
- Suppresses sympathetic jumpy activity, lowering heart rate and blood pressure
- Common Brand Name:
- Domitor®
- Reversal Agent:
- Atipamezole (Antisedan®) – a specific antidote that reverses both sedation and cardiovascular effects
- Side Effects:
- Bradycardia (slow heart rate)
- Hypotension (low blood pressure)
- Vomiting
- Respiratory depression
- Use in Humans:
- Medetomidine is not approved for human use, but its close relative dexmedetomidine (brand name Precedex) is used for ICU sedation.
⚠️ Public Health Note:
Medetomidine has recently appeared as a cutting agent in illicit opioids like fentanyl, contributing to rising overdose risks. It is not detected on standard drug screens, making it a growing concern in emergency and public health settings.
Medetomidine in the Illicit Drug Supply: A Rare but Emerging Threat
While fentanyl and xylazine remain dominant concerns in the illicit drug landscape, a lesser-known veterinary sedative—medetomidine—is quietly beginning to surface. Although still rare, this compound has recently been detected in a small but growing number of drug samples, raising red flags among toxicologists and public health experts.
📊 Current Prevalence (2024–2025)
As of now, medetomidine is uncommon in most drug seizures and toxicology screens. However, isolated reports have emerged from:
- Philadelphia
- New York City
- Parts of Ohio and Massachusetts
In these locations, medetomidine has been identified in combination with fentanyl and xylazine, indicating its potential use as a poly-drug adulterant to enhance or prolong sedation.
🧪 How It’s Being Detected
Medetomidine is appearing in:
- Wastewater analysis
- Expanded toxicology panels
- Street drug samples tested by labs like NPS Discovery and DEA forensic units
It is often misidentified or missed unless tested explicitly for, due to similarities with other veterinary tranquilizers.
🧬 Why It’s Being Used
Medetomidine is a potent alpha-2 adrenergic agonist, much like xylazine. It induces deep sedation, analgesia, and muscle relaxation. As restrictions tighten around xylazine, illicit drug producers may turn to alternatives like medetomidine, which is still accessible in veterinary contexts and offers similar effects.
🚫 Not a Major Trend—Yet
Compared to xylazine, which contaminates 20–30% of fentanyl samples in some regions, medetomidine is still in its early stages of emergence. Most jurisdictions have not yet seen it at scale.
⚠️ Why It’s a Concern
Medetomidine does not respond to naloxone, the standard opioid overdose reversal medication. This makes its presence in street drugs a serious overdose risk, especially when combined with opioids or other sedatives.
Public health agencies are now applying early surveillance tactics, hoping to track and mitigate this substance’s spread before it follows the same trajectory as xylazine.
In summary, Medetomidine is not common yet, but it’s emerging. Its increasing appearance alongside fentanyl and xylazine signals a potential new wave of sedative adulterants in the illicit market. Continued surveillance, awareness, and harm reduction efforts are crucial to stay ahead of this developing issue.
Is Medetomidine the Next Xylazine? Emerging Concerns in the Illicit Drug Supply
As xylazine becomes more tightly regulated, a new veterinary sedative—medetomidine—is drawing attention as a potential replacement in the illicit drug market. While still rare, medetomidine’s pharmacological similarity to xylazine and its increased detection in a few regions suggest it may be entering the early stages of misuse.
🔁 Similar Sedative Effects
Both xylazine and medetomidine are alpha-2 adrenergic agonists, producing sedation, muscle relaxation, and pain relief. In veterinary settings, medetomidine is known to be:
- More potent
- Longer-acting
- More selective in targeting receptors
These properties may make it appealing to those seeking to enhance or prolong the sedative effects of opioids like fentanyl.
🚫 Regulation of Xylazine Fuels Shift
Xylazine has become a controlled substance in several U.S. states. It is under federal scrutiny due to its role in the “tranq dope” crisis—a deadly combination with fentanyl responsible for numerous overdoses.
As xylazine access becomes more limited, illicit manufacturers may be exploring alternatives like medetomidine to maintain the sedative effects users expect.
🧪 Veterinary Availability
Although not as commonly stocked as xylazine, medetomidine is still available in veterinary medicine, particularly for small animals. This opens a window for diversion into the illicit market, mainly as awareness of its effects spreads.
⚠️ Higher Potency = Higher Risk
Medetomidine is stronger than xylazine, which raises significant public health concerns:
- Its potency may increase the risk of respiratory depression and overdose.
- Like xylazine, naloxone does not reverse its effects, limiting overdose intervention options.
- There are no approved human uses, and little research exists on its impact on humans.
📉 Still Emerging—But Watch Closely
Unlike xylazine, which is now detected in 20–30% of fentanyl samples in some cities, medetomidine remains uncommon. However:
- Wastewater testing
- Toxicology screenings
- Forensic lab reports
…are beginning to pick up signs of its presence, suggesting early patterns of misuse.
🚨 Implications for Public Health
If medetomidine begins to replace xylazine in the street drug supply, it will bring new challenges:
- Overdose responses may need to be revised.
- Harm reduction workers and first responders may need updated training.
- Labs must expand drug-testing protocols to reliably detect it.
In summary, Medetomidine is not yet widespread, but it’s a chemical cousin of xylazine with the potential to take its place in certain drug mixtures. Its greater potency, lack of reversal, and emerging detection in a handful of cities make it a growing concern for public health officials, toxicologists, and harm reduction advocates. Ongoing surveillance and proactive education are essential to stay ahead of this emerging threat.
Recognizing and Responding to Medetomidine Overdose: Symptoms, Risks & Emergency Care
Understanding Medetomidine Overdose
Medetomidine is a potent veterinary sedative that can cause serious, potentially life-threatening effects if overdosed—mainly due to its impact on the central nervous and cardiovascular systems. While most commonly used in veterinary settings, both animal and accidental human exposures require urgent medical intervention.
⚠️ Symptoms of Medetomidine Overdose
🧠 Central Nervous System Effects:
- Profound sedation or unresponsiveness
- Ataxia (loss of coordination)
- Depressed reflexes
- Coma (in severe cases)
❤️ Cardiovascular Symptoms:
- Severe bradycardia (very slow heart rate)
- Hypotension (low blood pressure)
- Pale or cyanotic (blue) mucous membranes
- Arrhythmias (irregular heart rhythms)
😤 Respiratory Effects:
- Respiratory depression
- Shallow or slowed breathing
- Possible apnea (temporary cessation of breathing)
🧬 Other Possible Effects:
- Hypothermia
- Hypoglycemia (rare)
- Vomiting
🆘 Emergency Management
- Seek immediate veterinary or medical help.
- Administer atipamezole (Antisedan®), the standard reversal agent in animals.
- Provide supportive care: oxygen therapy, IV fluids, temperature stabilization, and monitoring of vital signs.
🚫 Human Risk (Accidental Exposure)
Although not approved for human use, accidental exposure—particularly among veterinary professionals or researchers—can lead to:
- Dizziness
- Sedation
- Low heart rate
- Loss of consciousness (with high doses)
🧪 If exposed, immediately contact poison control or emergency services.
The Rising Threat of Medetomidine: A Potent Sedative Fueling Overdoses in the Illicit Drug Supply
Medetomidine Overdoses Surge as the Drug Enters the Illicit Market
Reports of medetomidine-related overdoses are rapidly increasing across the United States due to its growing use as an adulterant in illicit opioids, particularly fentanyl. Developed initially as a veterinary sedative, medetomidine is far more potent than xylazine and is now being added to street drugs to intensify and prolong their effects. However, this combination is dangerous—causing severe sedation, slowed heart rate (bradycardia), and respiratory depression that are often unresponsive to naloxone, the standard opioid overdose reversal medication.
⚠️ Why Medetomidine Use Is Spreading
Several key factors explain medetomidine’s growing presence in the illicit drug supply:
- Potency and Effect: Its strong sedative effects make medetomidine appealing to illicit drug manufacturers looking to amplify the potency of opioids like fentanyl.
- Regulatory Evasion: As xylazine becomes more tightly regulated, medetomidine is being used as a legal workaround, not yet subject to the same restrictions.
- Detection Challenges: Medetomidine is not routinely detected in standard toxicology screenings, making it difficult to monitor, diagnose, or treat in overdose cases.
Sources: Fentanyl Free Communities, The Hospitalist, Partnership to End Addiction, JAMA Network, San Francisco Chronicle, NPR
🧠 A Growing Public Health Concern
The infiltration of medetomidine into the street drug market highlights the evolving landscape of substance use and overdose risk. This trend demands urgent updates to public health strategy, including:
- Expanded drug testing capabilities
- Education for clinicians, first responders, and the public
- Policy changes to regulate new adulterants
- Increased access to harm-reduction resources and evidence-based treatment
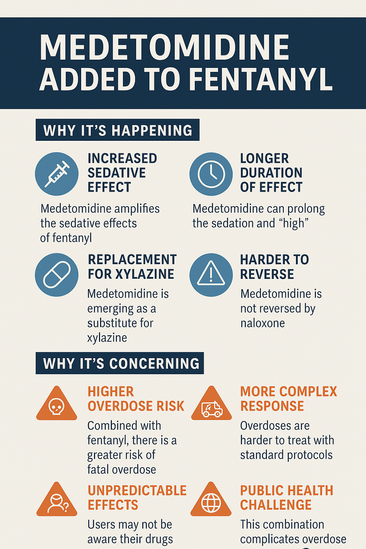
Why Medetomidine Is Being Added to Fentanyl—and Why It’s a Growing Public Health Risk
Medetomidine and Fentanyl: A Dangerous New Drug Combination
Medetomidine is not replacing fentanyl—it’s being added to it in the illicit drug supply. This combination is spreading rapidly, not to substitute opioids, but to enhance potency and extend sedation. Medetomidine, a veterinary sedative, is increasingly used as a cutting agent or booster to intensify fentanyl’s effects, leading to new and dangerous overdose patterns.
🔍 Why Medetomidine Is Being Added to Fentanyl
1. Increased Sedative Effect
- Medetomidine is a potent alpha-2 adrenergic agonist used in veterinary settings.
- When paired with fentanyl, it amplifies sedation, increasing the perceived “high.”
2. Longer Duration of Effect
- Fentanyl acts fast and fades quickly; medetomidine prolongs the sedative phase, making the drug experience feel stronger and last longer.
3. Replacement for Xylazine
- As xylazine (another veterinary tranquilizer) faces tighter regulation, medetomidine is emerging as a less detectable, loosely regulated substitute.
4. Harder to Reverse
- Medetomidine is not an opioid, so naloxone (Narcan)—the go-to reversal drug for opioid overdoses—does not affect it.
- This makes overdoses involving medetomidine more dangerous and more challenging to treat.
⚠️ Why This Is Concerning
- Higher overdose risk due to compounded respiratory depression from fentanyl and medetomidine
- Emergency treatments are less effective, complicating overdose response
- Unpredictable effects on unaware users exposed to sedatives not meant for human use
- Toxicology screens often miss medetomidine, delaying diagnosis and intervention
In summary, the rise of medetomidine in the drug supply reflects the ongoing evolution of substance adulteration. Public health agencies, treatment providers, and emergency responders must adapt quickly, updating drug screening tools, overdose protocols, and community education to reduce harm and save lives.
Frequently Asked Questions
Here are some common questions:
Question: Sample flyer about Medotomidine
Answer:
Question: What is the potency of medetomidine versus fentanyl?
Answer: Medetomidine and fentanyl are both highly potent drugs, but they act on different systems and are not directly comparable in terms of potency like two opioids would be. Here’s a breakdown to help clarify:
⚖️ Medetomidine vs. Fentanyl: Potency Comparison
| Property | Medetomidine | Fentanyl |
|---|---|---|
| Drug Class | Alpha-2 adrenergic agonist (sedative/analgesic) | Opioid agonist (pain reliever, euphoria, sedation) |
| Approved Use | Veterinary sedation and analgesia | Human and veterinary pain relief/surgical sedation |
| Sedative Potency | ~10–40× stronger than xylazine | Not a sedative, but causes profound sedation due to opioid effects |
| Analgesic Potency | Moderate (in animals) | ~50–100× stronger than morphine |
| Respiratory Depression | Moderate to severe (especially when combined) | Severe, primary cause of opioid overdose death |
| Reversal Agent | Atipamezole (Antisedan®) | Naloxone (Narcan®) |
🧪 Key Notes:
- Medetomidine is not an opioid, so it doesn’t cause euphoria like fentanyl.
- In the context of illicit use, it’s often added to fentanyl to intensify sedation and prolong its effects, making overdoses more dangerous and more challenging to reverse.
- Fentanyl remains far more potent as an analgesic and is directly linked to opioid-related overdose deaths.
🚨 Street-Level Risk:
Together, fentanyl + medetomidine cause:
- Compounded respiratory depression
- Extended unconsciousness
- Decreased responsiveness to naloxone
This cocktail is far more lethal than either drug alone.
Question: What government strategies to limit access and the use of medetomidine in veterinary facilities?
Answer: Government strategies to limit access and misuse of medetomidine in veterinary settings are beginning to evolve in response to its growing appearance in the illicit drug supply. These strategies aim to prevent diversion while maintaining legitimate medical and veterinary access.
U.S. Government and Regulatory Strategies
1. Monitoring Through DEA Schedule Review
- While medetomidine is not currently a federally scheduled controlled substance, the Drug Enforcement Administration (DEA) is assessing the growing risk of diversion.
- If misuse escalates, it may be classified as a controlled substance under the Controlled Substances Act, which increases regulation, storage, and prescribing requirements.
2. Enhanced Prescription Controls
- Veterinarians may be required to:
- Use tamper-resistant prescription pads
- Limit refill quantities
- Implement usage logs for high-risk sedatives
- Some states are already discussing Prescription Drug Monitoring Programs (PDMPs) for veterinary medications.
3. Restricted Distribution Channels
- Government agencies can work with manufacturers and distributors to:
- Limit bulk sales
- Require licensure verification
- Track distribution quantities more strictly
4. Veterinary Facility Security Protocols
- Encouraging or mandating:
- Locked storage cabinets for high-risk drugs
- Inventory audits and documentation
- Internal reporting of losses, theft, or suspicious use
5. Professional Education and Compliance
- State boards and veterinary associations can implement:
- Training on diversion prevention
- Reporting mechanisms for suspected diversion
- Guidelines for ethical prescribing and documentation
6. Collaboration with Law Enforcement and Public Health
- Encourage partnerships between:
- Veterinary boards and the DEA for compliance checks
- Public health departments for early warning alerts
- Local law enforcement will investigate thefts or illegal distribution
🛑 Future Considerations
If medetomidine becomes more widely misused:
Labeling requirements (e.g., “Not for human use”) may become stricter or mandated for visibility in drug seizures
Rescheduling and tighter federal control may become necessary
Cross-sector surveillance between veterinary, public health, and addiction services could be standardized
Conclusion
The emergence of medetomidine in the illicit drug market, particularly when combined with fentanyl, presents a growing public health threat. Its high potency and synergistic sedative effects drastically increase the risk of overdose, while its resistance to naloxone complicates emergency treatment. The inability of standard toxicology screens to reliably detect medetomidine further hinders timely diagnosis and intervention. As this trend spreads, it underscores the urgent need for updated drug screening protocols, targeted public education, and enhanced clinical awareness to mitigate the escalating risks associated with this dangerous drug combination.
Video: Vets Are Desperate to Stop This Addiction Trend #medetomidine #drugawareness #shorts