The involvement of the judicial system in opioid use disorder (OUD) recovery introduces a complex mix of legal, medical, and ethical considerations. This approach, increasingly adopted in recent years, seeks to address OUD through treatment mandates and diversion programs. While it offers potential advantages such as increased accountability and access to treatment, it also raises concerns, including coercion and stigmatization. Ethical dilemmas arise, challenging principles such as autonomy and equitable treatment. Navigating the nuances of the judicial system’s role in OUD recovery necessitates a thorough examination of its benefits, drawbacks, and the ethical complexities inherent in this intricate intersection of legal and healthcare realms.
How the Judicial System Can Address Opioid Use Disorder (OUD) Effectively
The opioid epidemic has profoundly impacted communities, highlighting the urgent need for innovative strategies within the judicial system to address opioid use disorder (OUD). Recognizing addiction as a medical condition rather than solely a legal issue has shifted many judicial policies towards rehabilitation and recovery. Here are key ways the judicial system plays a vital role in supporting offenders with OUD:
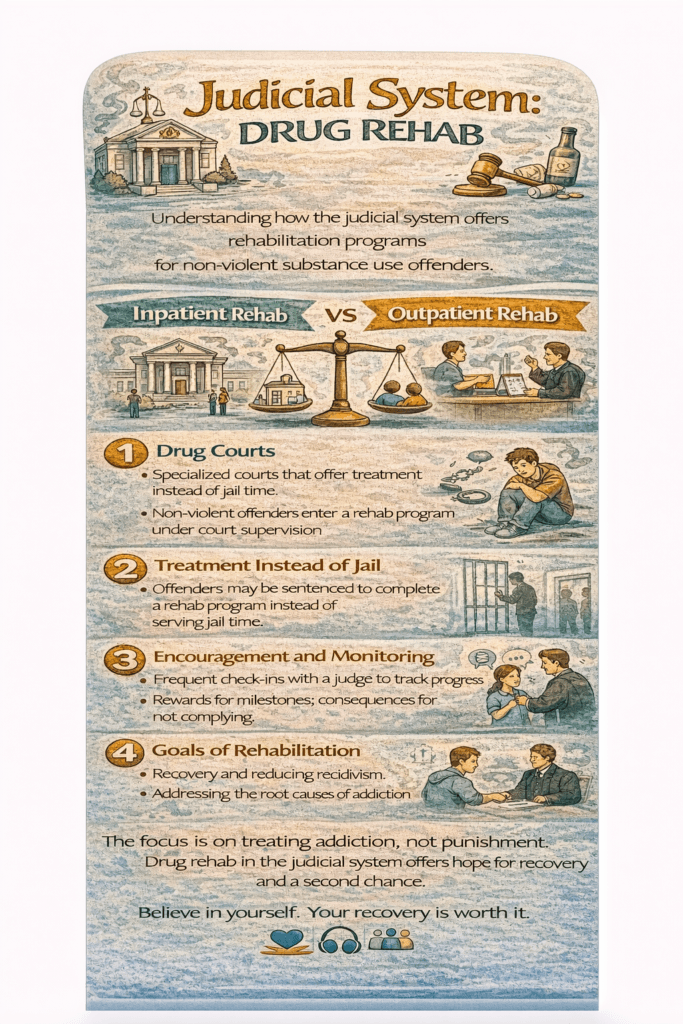
1. Drug Courts
Drug courts focus on rehabilitation rather than punishment for individuals with substance use disorders. These specialized dockets emphasize structured programs that include counseling, mandatory drug testing, and supervision. Participants who complete these programs often have their charges reduced or dismissed, providing a second chance at recovery.
2. Diversion Programs
Diversion programs allow eligible offenders to bypass traditional criminal proceedings by engaging in substance use treatment. These programs aim to address the root causes of addiction, offering participants the opportunity to rebuild their lives while reducing the burden on the judicial system.
3. Treatment as an Alternative to Incarceration
Many jurisdictions now prioritize treatment over incarceration for nonviolent offenders with OUD. Recognizing addiction as a chronic condition, these programs focus on long-term recovery through medication-assisted treatment (MAT) and counseling.
4. Mental Health Courts
For offenders with co-occurring mental health and substance use disorders, mental health courts provide specialized care. These courts aim to integrate treatment with judicial oversight, fostering recovery while addressing legal obligations.
5. Probation and Parole Support
Individuals on probation or parole can benefit from mandated substance abuse treatment as part of their supervision. These programs include regular check-ins, counseling sessions, and accountability measures to prevent relapse and recidivism.
6. Access to Treatment in Correctional Facilities
Increasingly, correctional facilities offer evidence-based treatments like MAT and counseling. Providing treatment during incarceration ensures continuity of care and better outcomes upon release, reducing the likelihood of relapse and reoffending.
7. Community Collaboration
Partnerships between courts and treatment providers enable seamless transitions from incarceration to community-based care. These collaborations often include housing support, employment assistance, and ongoing medical treatment.
8. Education for Legal Professionals
Courts can foster a compassionate approach by educating judges, attorneys, and staff about the science of addiction. Understanding addiction’s complexities equips legal professionals to make informed decisions and advocate for rehabilitation-focused outcomes.
9. Naloxone Distribution
Some jurisdictions include naloxone distribution programs in their judicial processes. By equipping individuals with life-saving tools like naloxone, courts actively contribute to harm reduction and prevent opioid-related fatalities.
10. Specialized Training for Court Personnel
Providing targeted training for judges, prosecutors, and defense attorneys enhances their ability to handle OUD cases effectively. Knowledge of evidence-based treatments ensures that judicial decisions align with best practices in addiction care.
In summary, the opioid crisis requires a multifaceted response, and the judicial system is uniquely positioned to promote change. By shifting from punitive measures to a focus on treatment, rehabilitation, and harm reduction, courts can play a pivotal role in combating the epidemic and fostering healthier communities.
Through collaboration, education, and innovative programs, the judicial system can help bridge the gap between addiction and recovery, offering individuals with OUD the support they need to reclaim their lives.
The Role of the Judicial System in Supporting Opioid Use Disorder (OUD) Recovery
Opioid use disorder (OUD) remains a pressing public health challenge, but the judicial system has emerged as a key player in addressing it. By focusing on rehabilitation and recovery rather than punishment, courts and legal frameworks can offer meaningful support to individuals struggling with addiction. Here are some of the advantages of the judicial system’s involvement in OUD recovery:
1. Diversion into Treatment Programs
Rather than pursuing traditional criminal proceedings, courts can divert individuals with OUD into specialized treatment programs. This approach prioritizes rehabilitation over incarceration, targeting the root causes of addiction and offering a path to recovery.
2. Individualized Treatment Plans
Judicially supervised treatment often involves developing individualized plans tailored to each person’s unique needs. By collaborating with treatment providers, courts can ensure that offenders receive the care most likely to support their recovery journey.
3. Supervised Rehabilitation
Participants in court-mandated OUD programs are closely monitored to ensure compliance with treatment requirements. This supervision fosters accountability and provides structured support, increasing the chances of sustained recovery.
4. Access to Medication-Assisted Treatment (MAT)
Judicial programs often facilitate access to evidence-based treatments like MAT. Medications such as methadone, buprenorphine, and naltrexone play a critical role in managing withdrawal symptoms and reducing cravings, which are vital steps toward long-term recovery.
5. Reduced Recidivism
By addressing the underlying issues of addiction, judicially supervised treatment programs help reduce recidivism. Successful recovery empowers individuals to reintegrate into society as law-abiding, productive citizens.
6. Community Reintegration
Court-involved recovery programs focus on preparing individuals for life beyond the justice system. By addressing factors contributing to substance use and criminal behavior, these programs promote successful reintegration into communities.
7. Addressing Co-occurring Disorders
Many individuals with OUD also struggle with mental health disorders. The judicial system’s involvement allows for comprehensive treatment plans that address both substance use and mental health needs, leading to better outcomes.
8. Court-Supervised Probation and Parole Programs
Probation and parole requirements often include participation in ongoing treatment and support services. This ensures continuity of care and creates a structured environment for individuals transitioning out of the justice system.
9. Public Health Approach
By framing addiction as a health issue, the judicial system aligns with evidence-based practices that emphasize treatment over punishment. This compassionate approach reflects a growing recognition of addiction’s medical and social dimensions.
10. Naloxone Distribution Programs
Courts can contribute to harm reduction by supporting naloxone distribution. Providing individuals with this life-saving tool upon release helps prevent overdose deaths and underscores the importance of reducing harm.
11. Community Engagement and Collaboration
Judicial involvement encourages partnerships between legal systems, treatment providers, and community organizations. This collaborative approach ensures a holistic response to addiction, addressing the multifaceted challenges faced by individuals with OUD.
In summary, the judicial system’s involvement in OUD recovery is a powerful opportunity to break the cycle of addiction and improve public health. By integrating treatment-focused strategies, courts can reduce the burden on the justice system while promoting recovery, reducing harm, and addressing the complex interplay between legal and health challenges.
This shift towards a compassionate and evidence-based approach marks a significant step in tackling the opioid crisis and fostering healthier, more resilient communities.
Challenges in Judicial System Involvement in Opioid Use Disorder (OUD) Recovery
The judicial system plays an influential role in addressing opioid use disorder (OUD) recovery, offering structured programs and pathways to rehabilitation. However, despite its potential benefits, integrating OUD recovery efforts within the legal system presents significant challenges and drawbacks. Recognizing these issues is essential for shaping a more effective and compassionate approach.
1. Stigmatization and Labeling
The involvement of individuals with OUD in the judicial system can inadvertently reinforce stigma and negative stereotypes. Labeling addiction as a criminal matter may hinder broader societal efforts to view addiction as a treatable health condition, complicating recovery and reintegration.
2. Limited Access to Treatment Resources
Judicially supervised programs often lack adequate treatment resources. Without access to comprehensive, evidence-based care—such as medication-assisted treatment (MAT) and counseling—individuals may face barriers to achieving sustainable recovery.
3. Mandatory Abstinence Requirements
Some court-mandated programs enforce strict abstinence policies, including discontinuation of MAT. This approach, which conflicts with harm reduction principles, may undermine recovery by neglecting the medical evidence supporting MAT’s effectiveness.
4. Coercion and Lack of Voluntariness
Court-mandated participation in recovery programs can be perceived as coercive, which may weaken the therapeutic alliance and reduce an individual’s intrinsic motivation to seek help. Voluntary engagement is often a key component of successful addiction treatment.
5. Potential for Legal Consequences
Failure to comply with treatment requirements can result in punitive outcomes, such as incarceration. This creates stress and can disrupt the therapeutic relationship, placing individuals at higher risk of relapse and disengagement from recovery efforts.
6. Limited Focus on Underlying Causes
Judicial programs frequently prioritize legal compliance over addressing the root causes of addiction. Underlying factors such as trauma, mental health disorders, and social determinants of health may be overlooked, limiting the long-term effectiveness of interventions.
7. Resource Allocation Challenges
The implementation of OUD recovery programs within the judicial system often faces resource constraints. Insufficient funding and staffing may compromise program quality and accessibility, reducing the likelihood of successful outcomes.
8. Inequities in the Justice System
Disparities in the justice system can exacerbate inequities in OUD recovery programs. Minority populations often face disproportionate legal representation and may have less access to culturally competent treatment and support.
9. Criminalization of a Health Issue
Critics argue that involving the judicial system in OUD recovery perpetuates the criminalization of addiction. Framing substance use disorders as legal issues rather than health conditions may conflict with public health approaches aimed at reducing harm and improving outcomes.
10. Limited Continuum of Care
Judicial programs frequently fail to provide ongoing support after court-mandated requirements are met. Without a robust continuum of care, individuals may face increased risks of relapse and difficulty maintaining long-term recovery.
11. Resistance to Change in Legal Practices
Traditional legal perspectives on addiction often resist adopting progressive, health-focused strategies. This resistance can hinder the implementation of evidence-based, harm reduction practices within the judicial system.
12. Lack of Cultural Competence
Many judicial programs lack cultural competence, making it challenging to provide effective, tailored care for diverse populations. This gap can contribute to disparities in access and outcomes for individuals from varying cultural and socioeconomic backgrounds.
In summary, while the judicial system has the potential to contribute positively to OUD recovery, its involvement must be carefully balanced with evidence-based practices and a public health perspective. Addressing these challenges requires collaboration among policymakers, legal professionals, and healthcare providers to create equitable, compassionate, and effective programs.
By prioritizing destigmatization, comprehensive treatment, and cultural competence, the judicial system can move toward an approach that better aligns with the complexities of addiction and recovery. Balancing legal accountability with health-focused strategies is essential for improving outcomes for individuals with OUD and their communities.
Ethical Dilemmas in Judicial System Involvement in Opioid Use Disorder (OUD) Recovery
The judicial system’s role in opioid use disorder (OUD) recovery is fraught with ethical complexities that arise at the intersection of legal, medical, and social domains. While the intent is often to promote rehabilitation and public safety, numerous ethical dilemmas highlight the challenges of navigating this approach effectively and compassionately.
1. Voluntariness and Autonomy
Ethical Dilemma:
Court-ordered participation in OUD recovery programs may undermine individual autonomy and self-determination. Ethical principles emphasize the importance of allowing individuals to make informed decisions about their healthcare, but mandated treatment can conflict with this ideal.
2. Coercion vs. Informed Consent
Ethical Dilemma:
Judicially mandated treatment often operates under a framework that may feel coercive. Individuals may comply with treatment plans out of fear of legal repercussions, raising questions about whether their consent to treatment is truly informed and voluntary.
3. Privacy and Confidentiality
Ethical Dilemma:
The sharing of sensitive health information between healthcare providers and legal entities can jeopardize an individual’s right to privacy. Striking a balance between necessary disclosures for legal compliance and maintaining confidentiality is a persistent ethical challenge.
4. Stigmatization and Dignity
Ethical Dilemma:
Involvement in the judicial system can perpetuate stigma against individuals with OUD, framing addiction as a moral or criminal failing rather than a medical condition. Upholding the dignity of individuals is critical to ensuring ethical treatment in both legal and healthcare settings.
5. Equity and Disparities
Ethical Dilemma:
Systemic inequities, including racial and socioeconomic disparities, often manifest in the judicial system’s handling of OUD cases. Ensuring fair and equitable access to recovery programs while avoiding discriminatory practices remains an ongoing ethical priority.
6. Criminalization of a Health Issue
Ethical Dilemma:
Critics argue that involving the judicial system in OUD recovery perpetuates the criminalization of addiction. Punitive approaches to a medical condition raise ethical concerns, highlighting the need for a shift toward public health-oriented strategies.
7. Treatment Effectiveness and Coercive Measures
Ethical Dilemma:
If mandated interventions fail to produce meaningful recovery outcomes, the use of coercive measures—such as incarceration for noncompliance—becomes ethically questionable. Balancing the goals of rehabilitation and justice is particularly challenging in these cases.
8. Cultural Competence and Sensitivity
Ethical Dilemma:
Judicial systems may lack the cultural competence needed to address the diverse backgrounds of individuals in OUD recovery. Ethical concerns arise when treatment plans fail to consider cultural nuances, leading to interventions that may not align with individuals’ values or needs.
9. Resource Allocation and Availability
Ethical Dilemma:
Limited resources within both judicial and healthcare systems pose challenges in allocating adequate support to individuals with OUD. Ethical questions arise when the needs of individuals must be weighed against broader societal demands.
10. Ongoing Support and Risk of Relapse
Ethical Dilemma:
Completing court-mandated treatment does not always guarantee long-term recovery support. The lack of a continuum of care raises ethical concerns about setting individuals up for potential relapse without sufficient follow-up resources.
In summary, navigating these ethical dilemmas requires a collaborative and multidisciplinary approach. Legal professionals, healthcare providers, ethicists, and policymakers must work together to ensure that judicial involvement in OUD recovery prioritizes ethical principles such as autonomy, justice, and compassion.
Frequently Asked Questions
Here are some common questions:
What is court-ordered drug rehabilitation?
Court-ordered drug rehab is a treatment program mandated by the judicial system for individuals whose substance use contributed to legal offenses. Instead of incarceration, eligible participants attend supervised treatment to support recovery and reduce repeat offenses.
Why does the judicial system use drug rehab programs?
The justice system uses rehab programs to address addiction as a health issue rather than only a criminal issue. Treatment lowers recidivism, reduces prison overcrowding, and helps individuals reintegrate into society safely.
What are drug courts?
Drug courts are specialized court programs that oversee individuals with substance use disorders. Participants follow structured treatment plans, attend counseling, submit to drug testing, and appear regularly before a judge to review progress.
Who qualifies for court-ordered rehab?
Eligibility depends on the offense, criminal history, and severity of substance use. Non-violent offenders with diagnosable addiction disorders are most commonly accepted.
What happens if someone fails court-ordered rehab?
Failure to follow treatment requirements may lead to sanctions such as stricter supervision, extended program length, or incarceration, depending on the violation.
How long do judicial rehab programs last?
Programs typically last from several months to over a year. Duration depends on progress, compliance, and individual treatment needs.
Are judicial rehab programs effective?
Research shows drug court and mandated treatment programs significantly reduce relapse and re-arrest rates when compared to traditional incarceration.
What types of treatment are included?
Programs may include detox services, medication-assisted treatment, individual counseling, group therapy, life-skills training, and relapse-prevention education.
Does court-ordered rehab respect patient rights?
Participants retain healthcare rights, confidentiality protections, and informed consent, although progress reporting to the court is required.
How does rehab benefit the community?
Successful rehabilitation lowers crime, reduces healthcare costs, strengthens families, and supports safer communities.
Can participation remove criminal charges?
In many programs, successful completion can reduce charges, shorten probation, or dismiss certain offenses depending on jurisdiction.
Is relapse considered failure?
Relapse is treated as part of recovery. Programs focus on accountability and continued treatment rather than immediate punishment.
Conclusion
The involvement of the judicial system in opioid use disorder (OUD) recovery represents a multifaceted approach with both potential benefits and inherent challenges. The advantages, including enhanced accountability and access to treatment, offer promising avenues for supporting individuals in their journey towards recovery. However, the disadvantages, such as concerns related to coercion and stigmatization, underscore the need for careful consideration and ethical scrutiny. The moral dilemmas arising from the intersection of legal mandates and healthcare interventions highlight the importance of balancing the pursuit of justice with respect for autonomy and equitable treatment. Moving forward, addressing these complexities requires collaborative efforts among legal professionals, healthcare providers, and policymakers to develop a holistic and ethically sound approach that prioritizes the well-being and dignity of individuals navigating the intricate terrain of OUD recovery within the judicial system.
Video: