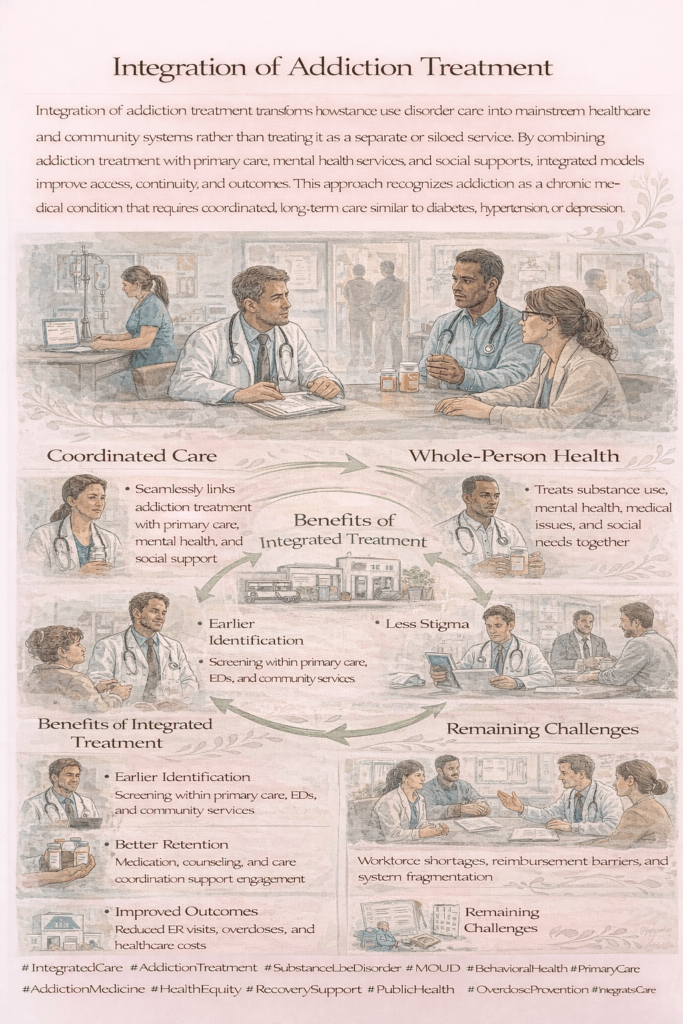
Integrating addiction treatment into primary care, hospitals, and broader healthcare systems is a pivotal strategy for providing holistic support to individuals with substance use disorders. This comprehensive approach enhances access to care, improves continuity of treatment, and helps to diminish the stigma often associated with addiction. However, it also presents several challenges that must be addressed to ensure effective and equitable care.
The Power of Integration: Incorporating Addiction Treatment into Primary Care and Hospitals
Integrating addiction treatment into primary care settings is a promising strategy for addressing substance use disorders early and effectively. Primary care providers (PCPs) are often the first point of contact for patients, placing them in an ideal position to identify the early signs of addiction and initiate treatment within the context of general health care. By making addiction care a routine part of primary care visits, healthcare systems can offer early interventions, closely monitor progress, and manage long-term recovery efforts more effectively.
One of the key benefits of integrating addiction care into primary care is the ability to normalize the conversation around substance use disorders. When addiction treatment is woven into routine health screenings, it reduces the stigma associated with seeking help for substance use. Patients are more likely to disclose substance use in a familiar environment, where it can be addressed with the same care and compassion as other chronic health conditions. This early identification is critical, as it allows for timely interventions that can prevent more severe health complications or crises from developing.
Primary care providers can also offer long-term, holistic management of addiction. By incorporating addiction treatment into regular check-ups, PCPs can monitor a patient’s recovery progress, adjust treatment plans as needed, and address any co-occurring health issues that may complicate recovery. This continuity of care ensures that patients have ongoing support and supervision, which is essential for maintaining sobriety and managing the complexities of addiction.
While primary care is instrumental in managing addiction in its earlier stages, hospitals play a crucial role when it comes to acute or severe cases. For patients experiencing a crisis, such as an overdose or withdrawal, hospitals provide immediate, life-saving interventions. Specialized treatment services within the hospital setting can offer comprehensive care, addressing both the physical and psychological aspects of addiction. This is especially important in cases where patients require medical detoxification, mental health support, or emergency care for complications related to substance use.
However, the role of hospitals doesn’t end with crisis management. Effective discharge planning ensures patients transition smoothly from the hospital to community-based addiction treatment services. Without proper follow-up care, patients are at a high risk of relapse after leaving the hospital. Hospitals must work closely with primary care providers, addiction specialists, and support services to create a comprehensive aftercare plan that includes counseling, medication-assisted treatment (MAT), and regular check-ins. This continuity of care helps bridge the gap between acute treatment and long-term recovery, giving patients the best chance of maintaining sobriety and rebuilding their lives.
Incorporating addiction treatment into both primary care and hospital settings is key to creating a healthcare system that can manage substance use disorders at every stage. By offering early interventions in primary care and comprehensive support in hospitals, we can ensure that patients receive the right care at the right time, improving treatment outcomes and reducing the stigma surrounding addiction.
This holistic approach saves lives and strengthens the entire healthcare system, making it better equipped to address the complexities of addiction and support patients on their journey to recovery.
Reducing Stigma: The Impact of Integrating Addiction Treatment into Mainstream Healthcare
One of the most profound benefits of integrating addiction treatment into mainstream healthcare is its potential to reduce the pervasive stigma surrounding substance use disorders. Addiction has long been misunderstood and viewed as a moral failing rather than a chronic medical condition. This misconception often leads to discrimination, fear, and shame, discouraging individuals from seeking the help they desperately need.
By embedding addiction care into the broader healthcare system, we can challenge these harmful stereotypes and change the way society perceives addiction. When addiction treatment becomes part of routine medical services, offered alongside management for diabetes, hypertension, or other chronic conditions, it helps to normalize addiction as a legitimate health issue rather than a personal shortcoming.
This integration shifts the conversation from blame to compassion. When primary care providers, hospitals, and healthcare specialists treat addiction like any other condition, it sends a clear message that addiction is a medical issue that can be effectively managed and treated. This can reduce the feelings of guilt and isolation that many individuals with substance use disorders experience, making it easier for them to come forward and seek treatment without fear of judgment.
Furthermore, when addiction treatment is integrated into regular healthcare services, it becomes more accessible and visible. Patients are more likely to encounter discussions about substance use during routine visits, whether through screenings, education, or treatment options provided by their general practitioners. This creates more opportunities for early interventions, making it easier to address substance use before it escalates into a more severe or life-threatening condition.
The ripple effects of this approach extend beyond the individual patient. As healthcare professionals become more accustomed to discussing and treating addiction in their everyday practice, they also contribute to changing public perceptions. When addiction is treated no differently from other health concerns, it breaks down the long-standing barriers of stigma, helping communities see that addiction is a medical issue, not a moral one.
For individuals struggling with addiction, this shift can be life-changing. The fear of being judged or discriminated against is one of the main reasons many people hesitate to seek help for substance use disorders. By making addiction treatment a routine part of healthcare, we can remove this barrier and encourage more people to take the first step toward recovery.
In the long run, integrating addiction treatment into mainstream healthcare can create a more compassionate, effective, and equitable healthcare system—one where individuals feel empowered to seek help without shame or fear and where addiction is recognized and treated as the chronic health condition it truly is. Reducing stigma is not just about changing perceptions; it’s about making care accessible and ensuring everyone can recover and live healthier lives.
Navigating the Challenges of Integrating Addiction Treatment into Healthcare Systems
While integrating addiction treatment into healthcare systems offers clear benefits, it also presents several complex challenges. One of the primary concerns is the allocation of resources. The integration process requires a significant investment in trained healthcare professionals, infrastructure, and sustained funding. Balancing the need for addiction services with the demands on existing healthcare resources is no small task. Without careful planning and prioritization, there is a risk that the expansion of addiction treatment could strain healthcare systems or divert attention from other essential services.
Resource allocation is a particularly pressing issue because addiction treatment requires specialized care. Healthcare professionals need specific training to recognize and manage substance use disorders effectively, but many healthcare systems are already operating under tight budgets and staff shortages. Expanding addiction services in these settings can create competition for resources, making it challenging to ensure that all patients receive the care they need. To address this, healthcare systems must find ways to integrate addiction care without undermining the delivery of other critical services, such as mental health, chronic disease management, or emergency care.
In addition to resource challenges, ethical dilemmas often arise during the integration process. One of the central concerns is ensuring that addiction treatment is provided equitably. Access to care must be fair, without discrimination based on socioeconomic status, race, or geographic location. Achieving this equitable care model requires a commitment to reducing healthcare disparities and ensuring that addiction treatment is available to all who need it.
At the same time, healthcare systems must balance comprehensive care with respect for patient autonomy and confidentiality. Addiction is a deeply personal issue, and patients may be reluctant to disclose substance use due to fear of judgment, stigma, or legal consequences. This fear can be compounded in integrated healthcare systems where addiction treatment is more visible and potentially shared across departments. Safeguarding patient privacy, particularly concerning sensitive health data, is crucial in maintaining trust between patients and providers. Healthcare providers must navigate the fine line between offering comprehensive, integrated care and respecting the privacy rights of individuals seeking addiction treatment.
Moreover, maintaining high standards of care while navigating these resource and ethical challenges is an ongoing struggle. Healthcare providers must ensure that addiction treatment is not only accessible but also practical and patient-centered. This means building a healthcare system that not only offers addiction services but also respects each patient’s rights, preferences, and dignity. Providers must be mindful of the ethical implications of their decisions, especially when it comes to issues like informed consent, shared decision-making, and the potential for coercion in addiction treatment.
Successfully integrating addiction treatment into healthcare systems requires a delicate balance between resource allocation and patient rights. As healthcare providers and policymakers work to expand addiction care, they must navigate the complexities of providing equitable, high-quality treatment while ensuring that patient autonomy and confidentiality remain central to the care process.
Despite the challenges, addressing these issues is essential for creating a healthcare system that can meet the needs of individuals struggling with addiction. With thoughtful planning, ethical vigilance, and a commitment to fairness, healthcare systems can provide comprehensive addiction care without compromising other vital services or patient rights.
Empowering Patients, Families, and Communities: Key Strategies for Integrating Addiction Treatment
A successful strategy for integrating addiction treatment into healthcare systems must go beyond clinical care—it requires empowering patients, engaging families, and leveraging community resources. These elements work together to provide a comprehensive, holistic approach that supports individuals throughout their recovery journey.
One of the most effective ways to enhance addiction treatment outcomes is by empowering patients through self-management. Educating patients about their condition, treatment options, and recovery processes helps them understand the complexities of addiction and the importance of their active participation in treatment. When patients are given the tools and knowledge to take ownership of their recovery, they are more likely to engage in healthy behaviors, adhere to treatment protocols, and make informed decisions that benefit their long-term well-being.
Self-management not only promotes personal accountability but also boosts patients’ confidence in their ability to manage their addiction. This empowerment can lead to improved treatment outcomes, as individuals who feel in control of their recovery are more likely to maintain sobriety and build a healthier lifestyle. Providing patients with resources such as relapse-prevention strategies, coping mechanisms, and access to peer support groups can further enhance their ability to navigate the challenges of recovery.
Family support is another crucial component of effective addiction treatment. Families can provide emotional and practical support during recovery, offering encouragement, understanding, and stability. Involving family members in the treatment process—through family therapy, education, and participation in recovery planning—creates a supportive environment that helps address underlying issues contributing to substance use. It also allows families to understand addiction better, which can reduce the stigma within the home and foster a more compassionate, cohesive approach to recovery.
For many individuals, addiction is rooted in complex family dynamics, and involving loved ones in treatment can help resolve these challenges, promoting long-term healing for both the patient and their family. When families work with healthcare providers, they create a robust support system that can offer ongoing encouragement and accountability, which are critical to preventing relapse and maintaining recovery.
Beyond the individual and family, community resources are essential for supporting sustained recovery from addiction. Community-based organizations, support groups, and local services provide additional layers of support that extend beyond the healthcare system. These resources offer counseling, job training, housing assistance, and social reintegration services that address the broader impacts of addiction on an individual’s life.
Community engagement also promotes social inclusion, reducing the isolation that often accompanies addiction. Support groups like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) provide safe spaces for individuals to connect with others who share similar experiences, fostering a sense of belonging and shared understanding. Moreover, job training programs and housing assistance can help individuals rebuild their lives after addiction, addressing critical social determinants of health that influence long-term recovery.
By integrating these elements—patient empowerment, family involvement, and community resources—into addiction treatment, healthcare systems can offer a more comprehensive approach that addresses not just the medical aspects of addiction but also its social and emotional dimensions. This holistic strategy improves treatment outcomes and helps individuals build a foundation for lasting recovery and a healthier future.
Successful addiction treatment is not a one-size-fits-all solution. It requires collaboration between healthcare providers, patients, families, and communities to create a network of support that addresses the many facets of addiction. By empowering patients, involving families, and utilizing community resources, healthcare systems can foster recovery in a sustainable, compassionate, and effective way.
Frequently Asked Questions
Here are some common questions:
What does “integration of addiction treatment” mean?
It means delivering substance use disorder care within general healthcare and community settings—such as primary care, hospitals, mental health clinics, and social services—rather than isolating it in separate specialty programs.
Why is integration necessary for addiction care?
Addiction is a chronic medical condition that often co-occurs with mental health issues, chronic disease, and social challenges. Integrated care improves access, continuity, and outcomes by addressing all needs together.
How is addiction treatment integrated into primary care?
Primary care clinics may screen for substance use, prescribe medications like buprenorphine or naltrexone, provide brief counseling, and coordinate referrals to behavioral health or specialty services.
What role do medications for substance use disorder play in integration?
Medications such as buprenorphine, methadone, and naltrexone are central to integrated care and can be prescribed alongside treatment for other chronic conditions.
How does integration reduce stigma?
When addiction is treated alongside diabetes, depression, or hypertension, it reinforces that substance use disorder is a medical condition—not a moral failure—reducing shame and bias.
Can addiction treatment be integrated into hospitals and emergency departments?
Yes. Many hospitals now initiate addiction treatment during admissions or emergency visits and connect patients to outpatient care after discharge.
How does integrated care help people with co-occurring mental health conditions?
Integrated models allow mental health and addiction treatment to occur together, improving symptom control and reducing relapse risk.
What is a multidisciplinary care team?
It includes medical providers, behavioral health clinicians, nurses, peer recovery specialists, social workers, and case managers working together in a coordinated system.
How does care coordination improve outcomes?
Shared records, warm handoffs, and team communication reduce gaps in care during transitions like hospital discharge or release from incarceration.
Does integrated care improve treatment retention?
Yes. People are more likely to stay engaged when treatment is accessible, coordinated, and delivered in familiar healthcare settings.
Conclusion
Integrating addiction treatment into primary care, hospitals, and healthcare systems is essential for providing comprehensive and practical support for individuals with substance use disorders. This approach improves access to care, ensures continuity of treatment, and helps reduce the stigma associated with addiction. However, addressing the challenges and ethical dilemmas involved requires careful planning, collaboration, and resource management. By combining patient self-management, strong family support, and community resources, healthcare systems can create a more supportive and effective environment for individuals affected by addiction, ultimately leading to better outcomes and improved quality of life.
Video: Team-based addiction treatment actually works #health #recovery