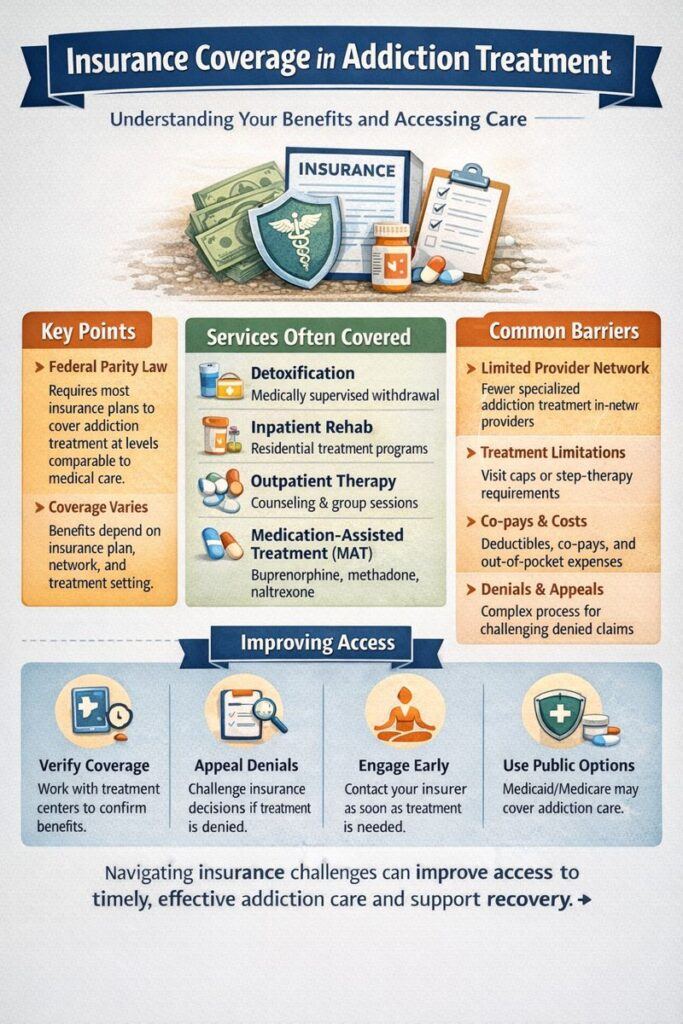
Insurance gaps in addiction treatment create significant barriers to accessing care due to limited coverage, high costs, and insufficient financial support. Government intervention is vital in enhancing coverage and funding through policy reforms. Self-management strategies, like seeking alternative financing and negotiating with providers, help individuals overcome financial obstacles. Family support, including education and advocacy, is vital for managing treatment costs, while community resource strategies, such as expanding low-cost services and increasing public awareness, play a crucial role in bridging these gaps and ensuring accessible addiction treatment.
The Impact of the Insurance Gap on Addiction Treatment: Challenges and Consequences
The insurance gap in addiction treatment can have profound effects, creating barriers that hinder access to care and exacerbate existing challenges for individuals seeking recovery. Here’s an overview of the critical impacts of inadequate insurance coverage on addiction treatment:
- Limited Access to Treatment
- Cost Barriers: Without sufficient insurance coverage, many individuals cannot afford the high costs associated with addiction treatment. This is particularly challenging for inpatient programs or long-term care, which can be prohibitively expensive.
- Reduced Availability of Services: Lack of comprehensive insurance may limit access to essential services, including detoxification, counseling, medication-assisted treatment (MAT), and aftercare. This limitation reduces the range of available treatment options and can compromise the effectiveness of recovery efforts.
- Delayed or Interrupted Care
- Delay in Seeking Treatment: High out-of-pocket costs can discourage individuals from seeking timely help, leading to worsening addiction and complicating the recovery process. Many may delay treatment until their situation becomes more severe.
- Incomplete Treatment: Individuals with insufficient insurance may have to leave treatment programs prematurely due to financial constraints, disrupting their recovery process and increasing the risk of relapse.
- Increased Financial Burden
- Debt Accumulation: Paying for addiction treatment out of pocket can result in significant debt, adding a layer of financial stress during an already challenging time. This economic burden can impede recovery and impact overall well-being.
- Financial Strain on Families: The costs associated with addiction treatment can place a considerable strain on families, leading to emotional and economic hardships. This strain can further destabilize the individual seeking help and affect the family’s stability.
- Exacerbation of Health Disparities
- Unequal Access: The insurance gap disproportionately affects low-income individuals, minorities, and those in rural areas, exacerbating existing health disparities in addiction treatment. These populations often face greater obstacles to accessing necessary care.
- Increased Mortality and Morbidity: Without adequate coverage, individuals are more likely to go untreated or receive inadequate care, increasing their risk of overdose, other health complications, and death.
- Higher Rates of Relapse and Recidivism
- Lack of Follow-Up Care: Insurance limitations often restrict access to ongoing care, such as counseling and relapse prevention. Without these crucial follow-up services, individuals are more likely to relapse or reenter the criminal justice system, hindering long-term recovery success.
- Overburdened Public Health Systems
- The strain on Public Programs: The uninsured or underinsured often rely on publicly funded treatment programs, which can become overwhelmed by demand. This strain can lead to long wait times and reduced service availability, affecting the quality of care.
- Emergency Room Visits: Many individuals without insurance turn to emergency rooms for crisis care, which is not ideal for managing addiction and places additional strain on healthcare systems.
Addressing the insurance gap is critical for improving access to comprehensive and affordable addiction treatment. By ensuring that more individuals can obtain the care they need without facing financial barriers, we can enhance recovery outcomes and support long-term success in overcoming addiction.
Understanding the Insurance Gaps in Addiction Treatment: Causes and Implications
Insurance gaps in addiction treatment arise from a complex interplay of systemic issues and limitations within the healthcare and insurance systems. These gaps can significantly affect access to necessary care and contribute to treatment disparities. Here are some of the key reasons for these insurance gaps:
- Limited Insurance Coverage
- Inadequate Mental Health Parity: Although laws require mental health and substance use disorders to be covered at par with physical health conditions, insurance plans often fall short in practice. Coverage for addiction treatment may be minimal or excluded altogether, limiting access to essential care.
- Variability in Coverage: Insurance plans vary widely in their coverage of addiction treatment services. Some may only cover outpatient services or exclude long-term residential care, leading to inconsistent access and potentially incomplete treatment options.
- High Costs of Addiction Treatment
- Expensive Treatments: Comprehensive addiction treatment, particularly inpatient or long-term programs, can be prohibitively costly. Many insurance plans do not cover the full spectrum of required services, such as detoxification or specialized therapies, making treatment financially inaccessible for many individuals.
- High Deductibles and Co-Pays: Even with insurance coverage, high deductibles and co-pays can render treatment unaffordable. This financial burden may cause individuals to delay or forgo necessary care, exacerbating their addiction.
- Insurance Policy Limitations
- Restrictions and Limitations: Insurance policies often limit the number of covered treatment sessions, the duration of care, or the types of services available. These restrictions can hinder access to the comprehensive care needed for effective addiction treatment.
- Preauthorization Requirements: Some insurance plans require preauthorization for specific treatments, creating additional barriers and potential delays in accessing care. This can complicate and slow down the treatment process for individuals seeking help.
- Lack of Integration Between Services
- Fragmented Care: Effective addiction treatment typically involves a combination of services, including medical care, mental health counseling, and social support. Insurance plans may not cover all these components comprehensively, leading to gaps in care and potential fragmentation of treatment.
- Stigma and Misunderstanding
- Stigma Around Addiction: The stigma associated with addiction can influence insurance companies’ willingness to provide robust coverage. This stigma may also affect policy decisions, leading to less comprehensive support for addiction treatment.
- Misunderstanding of Addiction as a Medical Condition: Some policymakers and insurers may not fully recognize addiction as a chronic medical condition requiring long-term, multifaceted treatment. This misunderstanding can result in inadequate coverage and support.
- Regulatory and Policy Gaps
- Inconsistent State Regulations: State regulations regarding insurance coverage for addiction treatment can vary significantly. These inconsistencies contribute to disparities in access and coverage, with some states offering more robust mandates than others.
- Lack of Enforcement: Even where laws mandate parity in coverage, enforcement can be inconsistent. Insurance companies may exploit policy loopholes or restrictive practices to limit financial liability, undermining the intended coverage.
- Economic and Market Factors
- Cost Control Measures: Insurers often implement cost-control measures that can limit coverage for addiction treatment. These measures might include restricting the types of facilities or treatments covered or negotiating lower reimbursement rates with providers.
- Market-Driven Decisions: Insurance companies may prioritize profit margins over comprehensive coverage, leading to plans that offer minimal support for addiction treatment compared to other medical conditions.
- Underfunded Public Programs
- Limited Public Funding: Publicly funded programs like Medicaid or community health centers often face limited resources and long waiting lists. This underfunding contributes to gaps in coverage and access to addiction treatment services.
Addressing these insurance gaps requires systemic changes, including improving mental health parity, expanding coverage options, and increasing both public and private investment in addiction treatment services. By tackling these issues, we can work towards a more equitable and effective system of care for individuals struggling with addiction.
Government Reform: Closing Insurance Gaps in Addiction Treatment
Government reform is crucial for addressing insurance gaps in addiction treatment and ensuring that individuals have access to the comprehensive care they need. By tackling systemic issues and enhancing coverage, government initiatives can significantly improve the accessibility and quality of addiction treatment services. Here’s how government reform can make a positive impact:
- Enhanced Parity Laws
- Strengthen Enforcement of Mental Health Parity: The government can ensure that laws mandating parity between mental health and substance use disorder treatment and physical health care are strictly enforced. This includes requiring insurance plans to provide equal coverage for addiction treatment in terms of benefits, copayments, and out-of-pocket costs.
- Expand Coverage Requirements: Updating and expanding regulations to cover a broader range of addiction treatments—such as long-term residential care, detoxification, and follow-up services—can help address existing coverage gaps.
- Increase Funding and Support for Public Programs
- Expand Public Health Funding: Increasing funding for publicly funded programs like Medicaid and community health centers is essential. This can improve access to a broader range of addiction treatment services and reduce waiting times for care.
- Support for Underserved Areas: Allocating resources to expand addiction treatment services in underserved and rural areas ensures that individuals in these regions can access necessary care.
- Reduce Financial Barriers
- Implement Cost-Sharing Reforms: Policy changes or subsidies can reduce high deductibles and co-pays for addiction treatment services, making treatment more affordable for underinsured or uninsured individuals.
- Provide Financial Assistance Programs: Developing and funding financial assistance programs, such as grants or sliding-scale fees based on income, can help individuals cover addiction treatment costs.
- Improve Insurance Coverage and Regulation
- Standardize Coverage Requirements: Establishing national standards for addiction treatment coverage ensures consistency across insurance plans. This should include mandatory coverage for a full spectrum of services, including prevention, treatment, and recovery support.
- Regulate Insurance Practices: Implementing regulations to prevent insurance companies from using restrictive practices—such as limiting the number of covered treatment sessions or imposing unnecessary preauthorization requirements—can help ensure more comprehensive coverage.
- Promote Integration of Services
- Encourage Integrated Care Models: Supporting integrated care models that combine addiction treatment with mental health care and primary care can improve overall care coordination and reduce treatment gaps.
- Facilitate Seamless Referrals: Improving the referral process between care providers ensures individuals receive comprehensive, continuous treatment.
- Increase Public Awareness and Education
- Fund Educational Campaigns: Investing in public education campaigns to raise awareness about addiction as a chronic medical condition and the importance of comprehensive treatment can help reduce stigma and promote acceptance of addiction treatment services.
- Train Healthcare Providers: Training healthcare providers to address addiction as part of overall healthcare and to understand available treatment options can improve the quality of care.
- Enhance Data Collection and Research
- Support Research on Addiction Treatment: Funding research to better understand practical addiction treatment approaches and identify coverage gaps can inform policy decisions and improve treatment strategies.
- Improve Data Collection: Collecting and analyzing addiction prevalence, treatment outcomes, and insurance coverage gaps helps guide policy reforms and allocate resources more effectively.
- Encourage Innovation in Treatment Delivery
- Support Alternative Treatment Models: Encouraging the development and implementation of innovative treatment models—such as telemedicine and mobile health applications—can increase access to care for individuals who face barriers to traditional treatment settings.
- Pilot Programs: Funding and evaluating pilot programs that explore new approaches to addiction treatment and insurance coverage can yield successful models for broader policy changes.
By implementing these reforms, the government can play a pivotal role in bridging insurance gaps and making addiction treatment more accessible and practical. Such reforms improve individual outcomes, enhance public health, and reduce the broader societal impacts of addiction.
Self-Management Strategies to Navigate Insurance Gaps in Addiction Treatment
Facing an insurance gap in addiction treatment can be challenging. Still, there are several self-management strategies that individuals can use to effectively manage their care and access necessary services despite financial constraints. Here are some practical steps to help navigate these obstacles:
- Research and Understand Insurance Options
- Review Insurance Plans: Take the time to thoroughly review various insurance plans to understand what each offers in terms of addiction treatment coverage. Pay attention to benefits, co-pays, deductibles, and out-of-pocket maximums.
- Seek Assistance: Contact insurance brokers or navigators for expert guidance on selecting a plan that offers the best coverage for addiction treatment needs.
- Explore Alternative Funding Sources
- Look for Grants and Financial Aid: Research grants, scholarships, and financial aid programs designed to assist with addiction treatment costs. Many nonprofits and local organizations provide financial support for these services.
- Utilize Community Resources: Contact community organizations, charities, and religious groups that may offer financial assistance or support for addiction treatment.
- Consider Sliding-Scale Fees
- Seek Providers with Sliding-Scale Fees: Look for treatment providers who offer sliding-scale fees based on income. This approach can make addiction treatment more affordable for those with limited financial resources.
- Negotiate with Providers
- Discuss Payment Plans: Talk with treatment providers about setting up a payment plan that allows you to spread the cost of treatment over time, making it more manageable.
- Inquire About Discounts: Ask providers whether they offer upfront payment discounts or have special programs for uninsured or underinsured patients.
- Leverage Telehealth and Online Resources
- Utilize Telehealth Services: Take advantage of telehealth options for therapy and counseling. These services can be more affordable and eliminate travel costs.
- Access Online Support Groups: Join online support groups and forums to receive peer support and resources without the expense of traditional in-person meetings.
- Advocate for Yourself
- Appeal Insurance Decisions: If your insurance coverage is denied or insufficient, file an appeal with your insurance company. Provide thorough documentation and advocate for the necessary treatment coverage.
- Request Case Management: Seek assistance from case managers or patient advocates to navigate the insurance system and explore all available options.
- Maintain Comprehensive Records
- Keep Detailed Records: Maintain detailed records of all treatment sessions, communications with insurance companies, and financial transactions. This documentation can be crucial when addressing coverage issues or seeking reimbursement.
- Utilize Preventive and Early Intervention Services
- Engage in Preventive Care: Participate in preventive services and early intervention programs to address addiction issues before they require more intensive and costly treatments.
- Focus on Self-Care: Incorporate self-care practices, such as regular exercise, healthy eating, and stress management techniques, to support overall well-being and potentially reduce the need for more extensive treatment.
- Educate Yourself About Insurance and Treatment Options
- Stay Informed: Keep yourself updated on changes in insurance policies, addiction treatment options, and available resources. Being well-informed will help you make better decisions and advocate more effectively for your needs.
- Connect with Local Support Networks
- Engage with Local Support Groups: Join local support groups and networks to access guidance, resources, and help navigating insurance and treatment options.
By employing these self-management strategies, individuals can better navigate the complexities of insurance coverage and access the addiction treatment they need, even when faced with financial barriers. Taking proactive steps can lead to more effective care and improved outcomes in the recovery journey.
How Family Support Can Bridge Insurance Gaps in Addiction Treatment
Family support is crucial in addressing the insurance gap in addiction treatment. Families can help manage and mitigate these gaps by taking proactive steps. Here are some strategies that can make a significant difference:
- Educate and Advocate
- Understand Insurance Coverage: Take the time to educate yourself and your family members about the specifics of the insurance policy. Familiarize yourself with coverage limits, co-pays, deductibles, and the types of addiction treatment services included.
- Advocate for Necessary Coverage: Help the individual with addiction navigate the insurance system. File appeals for coverage denials and advocate for the inclusion of necessary services to ensure comprehensive treatment.
- Explore Financial Assistance and Resources
- Research External Funding: Find financial assistance programs, grants, and scholarships to cover treatment costs. Many nonprofits and community organizations offer financial support specifically for addiction treatment.
- Utilize Community Resources: Connect with local community organizations, charities, and support groups that may provide financial aid or discounted treatment options.
- Assist with Treatment Navigation
- Help Find Affordable Care: Support the search for treatment providers who offer sliding-scale fees or who work with low-income clients. This can make addiction treatment more accessible and affordable.
- Coordinate Care: Aid in coordinating between various care providers and services to ensure that all aspects of treatment are covered and that the individual receives comprehensive care.
- Provide Emotional and Practical Support
- Offer Emotional Support: Encouragement and understanding to help the individual stay motivated and engaged in their treatment, even when financial barriers arise.
- Help with Logistics: Assist with transportation to treatment facilities, managing appointments, and ensuring consistent session attendance.
- Promote Healthy Communication
- Foster Open Dialogue: Encourage open communication within the family about the challenges and needs related to addiction treatment. This collective approach can help in planning and addressing financial concerns more effectively.
- Work Together: Collaborate with family members to share responsibilities and resources. Pooling resources or adjusting budgets may help cover treatment costs.
- Manage Finances Together
- Create a Budget: Develop a family budget that includes provisions for addiction treatment costs. This will help manage expenses and plan for any out-of-pocket costs.
- Explore Financial Planning: Consult with a financial advisor or counselor to explore options for efficiently managing and financing treatment expenses.
- Encourage Preventive Care
- Support Preventive Measures: Encourage participation in preventive care and early intervention services to address addiction issues before they require more intensive treatments.
- Promote Healthy Habits: Support lifestyle changes and self-care practices that can help manage addiction and improve overall well-being, potentially reducing the need for costly treatments.
- Stay Informed and Involved
- Stay Updated: Stay informed about changes in insurance policies, treatment options, and available resources. This knowledge can help you make better decisions and access the proper care.
- Engage in Family Therapy: Participate in family therapy or counseling to address any dynamics affecting treatment and to improve overall support for the individual.
- Leverage Support Networks
- Connect with Support Groups: Engage with support groups for families affected by addiction. These groups can provide valuable information, resources, and emotional support.
- Build a Support Network: Connect with other families who have navigated similar challenges. Sharing experiences and strategies can offer practical solutions and emotional encouragement.
By implementing these family support strategies, families can play a pivotal role in bridging insurance gaps in addiction treatment and ensuring that their loved ones receive the care they need.
Community Resource Strategies to Address the Insurance Gap in Addiction Treatment
Community resource strategies play a crucial role in bridging the insurance gap in addiction treatment. By leveraging local resources and fostering collaboration, communities can support individuals facing financial barriers to care. Here are some key strategies communities can use:
- Increase the Availability of Low-Cost and Free Services
- Develop Community Health Centers: Establish or expand community health centers that offer low-cost or sliding-scale addiction treatment services. These centers provide critical care regardless of an individual’s insurance status.
- Support Nonprofit Organizations: Fund and encourage nonprofits that offer free or subsidized addiction treatment and support services, such as detox programs, counseling, and recovery support.
- Enhance Public Awareness and Education
- Conduct Awareness Campaigns: Run public education campaigns to inform the community about available addiction treatment resources, including those offering financial assistance or sliding-scale fees.
- Provide Educational Resources: Offer workshops and seminars on navigating insurance coverage, understanding addiction treatment options, and accessing financial aid.
- Facilitate Access to Financial Assistance
- Promote Grants and Scholarships: Share information about grants, scholarships, and financial aid programs that can help cover the costs of addiction treatment. Assist individuals in applying for these resources.
- Collaborate with Local Businesses: Partner with local businesses and organizations to create sponsorships or funding initiatives to support addiction treatment services.
- Develop and Support Peer Support Networks
- Create Peer Support Groups: Establish and support peer-led groups that provide emotional support, share information about financial resources, and offer practical advice on navigating treatment options.
- Facilitate Recovery Communities: Build and sustain recovery communities that offer social support and connections to additional resources and services.
- Advocate for Policy and System Changes
- Engage in Advocacy: Advocate for policy changes that improve access to addiction treatment and address insurance coverage gaps. Support legislation that mandates comprehensive coverage and reduces financial barriers.
- Support Insurance Reform: Work with policymakers to develop and implement reforms that increase insurance coverage for addiction treatment and reduce out-of-pocket costs.
- Improve Service Coordination and Integration
- Enhance Service Coordination: Develop programs that coordinate between providers to ensure seamless access to addiction treatment and support services, including those offering financial assistance.
- Promote Integrated Care Models: Support models that combine addiction treatment with other health services to ensure comprehensive care and reduce the need for multiple insurance claims.
- Expand Access to Telehealth Services
- Support Telehealth Options: Advocate for and facilitate the expansion of telehealth services for addiction treatment. Telehealth can reduce costs and improve accessibility for those with limited insurance coverage.
- Provide Virtual Support Groups: Offer online support groups and counseling services accessible to individuals facing barriers to in-person treatment.
- Create Resource Directories and Referral Services
- Develop Resource Directories: Create and maintain directories of available addiction treatment resources, including those offering financial assistance, sliding-scale fees, and low-cost services.
- Establish Referral Services: Set up referral services that connect individuals to appropriate treatment options based on their financial situation and insurance coverage.
- Encourage Community-Based Fundraising
- Organize Fundraising Events: Host community fundraising events to support addiction treatment programs and individuals in need. These events can raise awareness and generate financial support.
- Crowdfunding Campaigns: Support and promote crowdfunding campaigns to raise money for individuals seeking addiction treatment and help cover insurance coverage gaps.
- Strengthen Collaboration Among Local Agencies
- Foster Partnerships: Encourage collaboration between local government agencies, healthcare providers, social services, and community organizations to create a coordinated response to addiction treatment needs.
- Share Best Practices: Facilitate information sharing and collaboration among organizations to improve the effectiveness of community resource strategies and address insurance gaps.
By implementing these community resource strategies, communities can play a vital role in addressing the insurance gap in addiction treatment and ensuring that individuals receive the care they need, regardless of their financial situation.
Frequently Asked Questions
Here are some common questions:
Why do insurance companies deny addiction treatment?
Denials may occur due to lack of prior authorization, out-of-network providers, failure to meet “medical necessity” criteria, or step-therapy requirements that mandate trying lower levels of care first.
Does insurance always cover inpatient rehab?
Not always. Many plans cover inpatient or residential treatment only when outpatient care is deemed insufficient. Coverage may also be limited to a specific number of days.
Does insurance cover medication-assisted treatment (MAT)?
Most plans cover MAT, but restrictions such as prior authorization, dosage limits, pharmacy lock-ins, or higher copays may apply.
How does Medicaid coverage differ from private insurance?
Medicaid often provides broader addiction treatment coverage, including MAT and counseling, but access depends on state policies and provider availability.
What can patients do if treatment is denied?
Patients can appeal insurance denials, request a medical necessity review, or seek help from treatment centers that specialize in insurance verification and advocacy.
Conclusion
Addressing insurance gaps in addiction treatment is essential for improving access to care and supporting recovery. These gaps are often caused by limited coverage and high costs, which can be mitigated through targeted government intervention, such as policy reforms and increased funding. Self-management strategies and family support are crucial in navigating financial barriers and ensuring continuity of care. Additionally, community resource strategies, including expanding low-cost services and raising public awareness, are vital for bridging these gaps and making effective addiction treatment more accessible to those in need. Together, these approaches can help create a more equitable and supportive system for addiction recovery.
Video: They’re Required to Cover It, So Why Won’t They? #InsuranceCoverage #Recovery