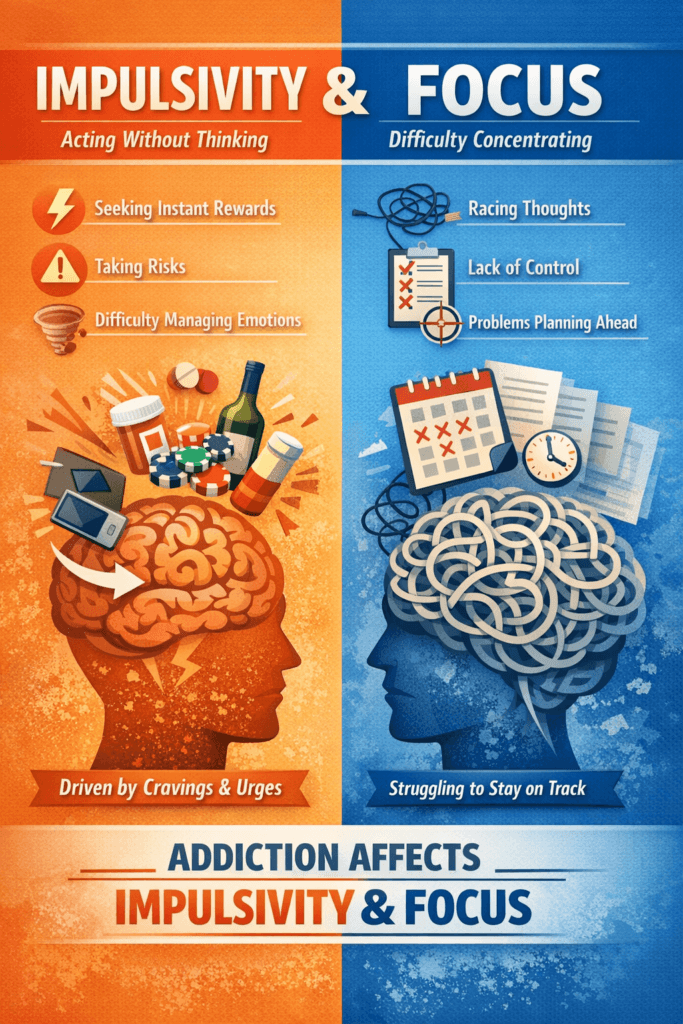
Impulse control problems and attention deficits play a significant role in addiction, as both are tied to dopamine pathways that regulate motivation and reward. When these systems are off balance, people may act on urges quickly or struggle to focus, making them more vulnerable to substance use. Medication can help improve attention and reduce impulsivity, but lasting recovery relies on more than treatment alone. Self-management strategies such as mindfulness, structure, and healthy coping skills build daily control, while family support provides encouragement and accountability. Community resources such as peer groups, counseling, and education provide a broader safety net for managing both addiction and attention challenges.
Strengthening Impulse Regulation and Attention Control: A Path to Safer and Healthier Lives
Impulse regulation and attention control are influential protective factors against risks like aggression, dangerous driving distractions, and relapse into addiction. By drawing from psychology, neuroscience, and behavioral science, we can see how improving these skills reshapes daily behavior and long-term outcomes.
1. Aggressive Behaviors
Impulsivity link: Aggression often stems from poor inhibitory control—the inability to pause before reacting emotionally. Impulsive individuals may lash out before considering consequences.
Attention regulation: Strengthening attention helps people recognize social cues, regulate emotions, and choose alternative responses. Cognitive-behavioral therapy (CBT) and mindfulness training enhance the brain’s prefrontal cortex (inhibition) to manage amygdala-driven emotional reactivity better.
Evidence: Research shows that mindfulness and impulse-control training reduce violent reoffending in criminal populations and lower aggression in schools and workplaces.
2. Dangerous Driving Distractions
Impulsivity link: Impulsive drivers tend to text while driving, speed, or take unnecessary risks, prioritizing immediate gratification over long-term safety.
Attention regulation: Training sustained attention lowers susceptibility to distractions such as smartphones, music, or daydreaming.
Evidence: Cognitive psychology and traffic safety studies reveal that stronger attentional control reduces lane deviations, improves reaction times, and lowers crash risk.
3. Addictive Relapse
Impulsivity link: Addiction is fueled by impulsive decision-making—choosing the quick fix of drugs over long-term goals. Impulsivity is a strong predictor of relapse after treatment.
Attention regulation: Improving attentional control allows individuals to notice cravings and triggers without immediately acting on them.
Evidence: Strategies such as contingency management, mindfulness-based relapse prevention, and cognitive training strengthen self-regulation and reduce relapse rates.
4. The Underlying Mechanism
Neuroscience: Both impulsivity and poor attention control reflect underactivation in the prefrontal cortex (planning, inhibition, working memory) and overactivation in emotion/reward regions such as the amygdala and nucleus accumbens.
Self-regulation training: Mindfulness, executive function training, and behavioral therapies enhance “top-down” brain control, shifting responses from reactive to deliberate.
✅ Conclusion
Strengthening impulse regulation and attention control protects multiple domains—reducing aggression, preventing risky driving, and lowering the risk of addictive relapse. This is why modern treatment approaches like Dialectical Behavior Therapy, mindfulness practices, and cognitive control training focus directly on building these capacities. By enhancing self-control and focus, individuals gain not only safety and resilience but also greater freedom to pursue long-term goals.
Medications That Help With Impulsivity and Poor Attention
Clinicians often use specific medications to manage impulsivity and poor attention, especially when these symptoms appear in conditions like ADHD, traumatic brain injury, mood disorders, or substance use disorders. Here’s a breakdown of the main categories:
1. Stimulant Medications (first-line for ADHD)
- Examples: Methylphenidate (Ritalin, Concerta), Amphetamine salts (Adderall, Vyvanse).
- Mechanism: Boosts dopamine and norepinephrine in the prefrontal cortex, improving executive function, attention, and inhibitory control.
- Effects:
- Reduce hyperactive and impulsive behaviors.
- Improve sustained attention.
- Limitations: Carry misuse potential, so they must be carefully monitored, especially in those with substance use disorders.
2. Non-Stimulant ADHD Medications
- Atomoxetine (Strattera): A selective norepinephrine reuptake inhibitor that improves attention and reduces impulsivity without abuse risk.
- Guanfacine (Intuniv) / Clonidine (Kapvay): Alpha-2 adrenergic agonists that calm overactive circuits, reduce impulsivity, and improve emotional regulation.
- Best Use: Often preferred when there are concerns about addiction or stimulant side effects.
3. SSRIs / Mood Stabilizers (for mood-linked impulsivity or aggression)
- SSRIs (e.g., fluoxetine, sertraline): Sometimes reduce impulsive aggression in mood disorders.
- Mood Stabilizers (e.g., lithium, valproate, lamotrigine): Useful when impulsivity stems from bipolar disorder or severe emotional swings.
- Atypical Antipsychotics (e.g., risperidone, aripiprazole): Can help manage impulsive aggression in certain psychiatric conditions.
4. Medications for Addiction-Related Impulsivity
- Naltrexone: An opioid antagonist that reduces impulsive drinking or gambling by blunting reward pathways.
- Bupropion: A dopamine/norepinephrine reuptake inhibitor that may reduce impulsivity and cravings, especially for nicotine or stimulants.
📌 Key Point
- The most effective medications for impulsivity and poor attention are stimulants and non-stimulant ADHD medications.
- When impulsivity is linked to mood disorders, aggression, or addiction, clinicians may consider SSRIs, mood stabilizers, or targeted options like naltrexone or bupropion.
By tailoring treatment to the underlying cause—whether ADHD, mood instability, or substance use—clinicians can reduce impulsivity, improve attention, and help individuals build stronger self-regulation skills.
Stimulant vs. Non-Stimulant Medications for Impulsivity and Poor Attention: Risks to Consider
Stimulant and non-stimulant medications are widely used to manage impulsivity and poor attention, especially in the treatment of ADHD. While both can be effective, each class comes with disadvantages and risks that patients, families, and clinicians need to weigh carefully.
🚨 Stimulant Medications (e.g., Methylphenidate, Amphetamines)
Disadvantages / Risks
- Side Effects
- Insomnia, decreased appetite, and weight loss
- Increased heart rate and blood pressure
- Headaches, stomachaches
- Jitteriness or anxiety
- Misuse / Addiction Potential
- Can be abused or diverted (e.g., taken in high doses, crushed, or snorted)
- Risk is higher in individuals with a history of substance use disorder
- Tolerance / Dependence
- Some develop tolerance, needing higher doses for the same effect
- Rare withdrawal symptoms (fatigue, low mood) if stopped suddenly
- Psychiatric Risks (less common)
- Can worsen anxiety, agitation, or tics
- Rarely triggers mania or psychosis in vulnerable individuals
🌱 Non-Stimulant Medications
Atomoxetine (Strattera)
- Disadvantages:
- Slower onset (takes weeks vs. days for stimulants)
- Side effects: nausea, fatigue, decreased appetite, sexual side effects
- Rare: liver injury, suicidal thoughts in young people
Alpha-2 Agonists (Guanfacine, Clonidine)
- Disadvantages:
- Sedation, fatigue, dizziness
- Low blood pressure, slow heart rate
- Risk of rebound hypertension if stopped abruptly
⚖️ Key Comparison
| Feature | Stimulants | Non-Stimulants |
|---|---|---|
| Effectiveness | Fast, strong effect | Moderate, slower onset |
| Addiction Risk | Higher (abuse potential) | Very low |
| Side Effects | Insomnia, appetite loss, CV effects | Sedation, dizziness, GI issues |
| Best For | Most ADHD cases, unless contraindicated | Patients with substance use risk, anxiety, or poor stimulant tolerance |
✅ Bottom Line
- Stimulants remain the most effective option but carry risks of misuse and cardiovascular/psychiatric side effects.
- Non-stimulants are safer for those at risk of addiction or sensitive to stimulants, though they are slower-acting and less potent.
Both options can be life-changing when prescribed thoughtfully. The best choice depends on an individual’s health history, risks, and long-term treatment goals.
Ethical Dilemmas in Using Stimulant and Non-Stimulant Medications for Attention and Impulsivity
Medications that target impulsivity and poor attention—whether stimulants or non-stimulants—can transform lives. But because they affect cognition, behavior, and risk of misuse, they raise critical ethical questions. Here’s a breakdown:
⚖️ Ethical Dilemmas with Stimulant Medications
- Fairness and Cognitive Enhancement
- Students or professionals sometimes use stimulants without ADHD to boost performance.
- Raises debate: Is this like cheating, similar to doping in sports? Does it create unfair advantage in academics or careers?
- Misuse and Diversion
- Prescribed stimulants can be sold, shared, or abused.
- Physicians face tension between serving the patient’s needs and preventing wider societal harm.
- Informed Consent in Children/Adolescents
- Parents often decide on medication for minors.
- Raises the dilemma: How much say should children have in taking a drug that changes mood, focus, and self-control?
- Medicalization of Normal Behavior
- Critics worry stimulants pathologize normal variations in attention or energy.
- Overdiagnosis and overprescription remain real concerns.
- Identity and Authenticity
- Some patients ask: “Am I myself, or the medicated version of me?”
- Raises ethical questions about authenticity and selfhood when medication alters personality.
🌱 Ethical Dilemmas with Non-Stimulant Medications
- Slower, Less Effective Treatment
- Clinicians may avoid stimulants for safety, but patients may feel denied the most effective option.
- Balancing individual benefit vs. societal safety can be ethically complex.
- Side Effects vs. Benefits
- Non-stimulants may cause sedation, low blood pressure, or sexual side effects.
- Raises the question: Is it ethical to prescribe a less effective drug with a significant impact on life?
- Access and Cost
- Non-stimulants are often more expensive and sometimes not covered by insurance.
- Raises concerns about fair and equitable access to care.
🌍 Broader Ethical Considerations (Both Types)
- Public Safety: Should stimulants be more tightly regulated to reduce misuse, even if that makes access harder for those who need them?
- Autonomy: Do patients always get complete information to make an informed choice about risks, benefits, and alternatives?
- Stigma: Some feel shame about “needing medication to function,” highlighting issues of social acceptance and mental health equity.
✅ Summary
- Stimulants raise dilemmas around fairness, misuse, and identity.
- Non-stimulants raise dilemmas around access, efficacy, and treatment trade-offs.
- At the core, these ethical questions balance individual benefit, societal risk, and fairness in use.
Self-Management Strategies While Using Medications for Impulsivity and Poor Attention
Medications can significantly improve focus and reduce impulsivity, but they work best when paired with intentional self-management strategies. Building structure, awareness, and coping skills maximizes the benefits while lowering risks like aggression, driving distractions, or addictive relapse. Here’s how to integrate self-management with medication use:
1. Medication Adherence & Monitoring
- Stick to prescribed doses/timing → prevents rebound impulsivity, misuse, or side effects.
- Use pill organizers, reminders, or apps to avoid skipped or double doses.
- Track side effects and benefits in a journal to share with healthcare providers.
2. Aggressive Behavior Reduction
- Pause-and-Plan Strategy: Count to 10 or take deep breaths before reacting—medications make this pause easier by improving inhibitory control.
- Cognitive-Behavioral Tools: Challenge thoughts (“What’s another way to see this?”) to stop anger from escalating.
- Mindfulness Practices: Meditation or grounding exercises reinforce calm, reducing reactive aggression.
3. Driving Safety & Distraction Control
- Medication Scheduling: Align peak focus times with driving; avoid driving if meds are wearing off.
- Distraction Minimization: Silence notifications or use “Do Not Disturb While Driving” features.
- Attention Training: Practice sustained focus tasks (e.g., driving simulators, “spot-the-difference” apps) to carry medication benefits into real-world driving.
4. Addiction & Relapse Prevention
- Trigger Journaling: Identify high-risk times/places and plan coping strategies—meds enhance awareness of cravings.
- Delay the Urge: Pair meds with the “10-minute rule” to reduce impulsive relapse decisions.
- Healthy Reward Substitution: Exercise, hobbies, or social connections can replace quick-reward seeking.
- Support Networks: Combine meds with peer support (e.g., AA, SMART Recovery) to reduce isolation-driven relapse.
5. Lifestyle Foundations (work with meds, not against them)
- Sleep Hygiene: Regular sleep prevents irritability from stimulant rebound.
- Balanced Nutrition: Small, regular meals stabilize focus and energy.
- Exercise: Boosts dopamine/norepinephrine naturally, complementing medication effects.
- Stress Management: Practices such as yoga, breathing exercises, and structured relaxation lower baseline impulsivity.
✅ Summary
Self-management with medications = awareness, structure, and coping skills.
- For aggression: pause-and-plan, mindfulness.
- For driving: minimize distractions, time doses wisely.
- For relapse: manage triggers, delay cravings, substitute healthy rewards.
- All reinforced by lifestyle routines that stabilize attention and strengthen self-control.
Family Support Strategies for Medications and Attention/Impulsivity
Family plays a critical role in supporting someone who uses medications for impulsivity and attention issues. While medications can regulate brain chemistry, family support strategies help turn those improvements into real-life gains in behavior, relationships, and safety.
1. Encourage Adherence & Monitoring
- Routine reminders: Use pill organizers, phone alarms, or simple check-ins.
- Side effect tracking: Families can notice changes in sleep, appetite, or mood that the person might overlook.
- Normalize medication use: Treat meds like any other health tool to reduce stigma.
2. Reducing Aggressive Behaviors
- Model calm responses: Family calmness reinforces the self-control supported by medication.
- De-escalation scripts: Agree on safe phrases, such as “Let’s take 5 minutes,” when tension rises.
- Reinforce positive behavior: Praise when coping strategies replace aggression.
3. Driving Safety & Attention Support
- Plan driving schedules: Encourage driving at peak medication times, avoid when focus wanes.
- Set boundaries: No phones while driving, pull over for texts.
- Monitor readiness: If meds are skipped or side effects occur, use alternative transportation.
4. Relapse Prevention in Addiction
- Trigger awareness: Help avoid or plan around risky places or situations.
- Accountability partners: Join support groups or medical appointments.
- Celebrate progress: Recognize milestones to build motivation.
- Compassion over criticism: Replace blame with supportive language.
5. Building Healthy Routines Together
- Shared habits: Exercise, healthy meals, and relaxation activities as a family.
- Sleep environment: Maintain calm, consistent evening routines.
- Stress management as a team: Practice mindfulness, yoga, or family walks.
✅ Summary
Family strategies make medications more effective by:
- Supporting adherence with reminders and encouragement.
- Reducing aggression through calm modeling and positive reinforcement.
- Promoting safe driving with clear boundaries and planning.
- Preventing relapse through accountability and compassion.
- Building healthy routines together that reinforce attention and self-control.
Community Resource Strategies to Support Medications for Impulsivity and Attention
Community resources extend the benefits of medication into real-world environments where aggression, unsafe driving, and relapse risks are most likely to occur. By combining medical treatment with social, educational, and behavioral supports, individuals gain the tools they need for safer, more stable lives. Here’s a breakdown of strategies:
1. Aggression Reduction & Emotional Regulation
- Anger Management Groups: Group therapy at community centers reinforces the benefits of medication with practical coping skills.
- Conflict Resolution & Restorative Justice Programs: Provide structured ways to resolve disputes and prevent escalation.
- Mentorship Programs: Pair individuals with role models who encourage healthy behavior and medication adherence.
2. Driving Safety & Attention Support
- Driver Safety Courses: Defensive driving and distraction-prevention training align with medication’s attention benefits.
- Digital Resources: Apps and simulators offered by DMVs or nonprofits help reduce distraction and improve focus.
- Employer & School Partnerships: Provide carpooling, transit passes, or alternative transport when medication coverage is low.
3. Relapse Prevention in Addiction
- Peer Support Groups: NA, AA, SMART Recovery, or Celebrate Recovery provide accountability and structure.
- Recovery Community Centers: Offer sober events, job support, and social connections to reduce isolation.
- Medication-Assisted Treatment Clinics: Integrate ADHD/impulsivity meds with addiction-focused medications like buprenorphine or naltrexone.
- Crisis Hotlines & Peer Coaches: Immediate support during cravings or relapse urges.
4. Education & Skill-Building Resources
- Workshops at Colleges or Libraries: Teach time management, stress management, and mindfulness skills.
- Family Education Programs: NAMI and similar initiatives help families reinforce the benefits of medication.
- Job Skills Training: Vocational programs foster stability and reduce the risk of relapse or aggression.
5. Integrated Care Models
- Community Health Clinics: Provide wraparound care with doctors, therapists, and peer specialists working together.
- Court & Probation Programs: Link medications with behavioral monitoring for aggression or driving violations.
- Faith-Based and Cultural Organizations: Offer spiritual and cultural support to make medication use more meaningful.
✅ Summary
Community resources extend the medication’s benefits into real-life settings by:
- Reinforcing anger management and impulse control.
- Supporting safe driving practices through training and transport options.
- Preventing relapse with peer support, recovery centers, and crisis resources.
- Promoting holistic stability through education, family programs, and integrated care.
Together, these resources create a bridge between medical treatment and the daily environments where challenges—and growth opportunities—are most real.
Frequently Asked Questions
Here are some common questions:
Question: Provide a comparison chart of medications used to treat impulsivity and poor attention.
Answer: Comparison chart that shows which medications are most often used to treat impulsivity and poor attention, depending on the clinical context:
📊 Medications for Impulsivity & Poor Attention
| Condition | First-Line Medications | Alternative / Adjunctive | Notes on Impulsivity & Attention |
|---|---|---|---|
| ADHD (most common cause) | Stimulants: Methylphenidate (Ritalin, Concerta), Amphetamines (Adderall, Vyvanse) | Non-stimulants: Atomoxetine (Strattera), Guanfacine (Intuniv), Clonidine (Kapvay) | Stimulants most effective; non-stimulants preferred if risk of addiction, anxiety, or tics. |
| Mood Disorders / Aggression | SSRIs: Fluoxetine, Sertraline (esp. if impulsivity linked to irritability/anxiety) | Mood stabilizers: Lithium, Valproate, Lamotrigine Atypical antipsychotics: Risperidone, Aripiprazole | Reduce impulsive aggression and emotional reactivity rather than directly boosting attention. |
| Addiction / Substance Use Disorders | Naltrexone (for alcohol, gambling, opioid reward regulation) Bupropion (for nicotine, stimulant cravings) | Sometimes Atomoxetine or SSRIs if comorbid ADHD or anxiety present | Targets reward sensitivity and relapse risk; less about direct attention, more about impulse control. |
| Traumatic Brain Injury (TBI) / Neurological Causes | Stimulants (Methylphenidate, Amantadine) for cognitive rehab | SSRIs or Mood stabilizers for irritability/aggression | Often used short-term to improve focus and reduce behavioral dyscontrol. |
✅ Summary:
For addiction, medications like naltrexone and bupropion help by dampening reward-driven impulses and cravings.
ADHD medications (stimulants & non-stimulants) are the primary evidence-based treatments for impulsivity + poor attention.
If impulsivity is part of mood instability or aggression, SSRIs, mood stabilizers, or atypical antipsychotics may be added.
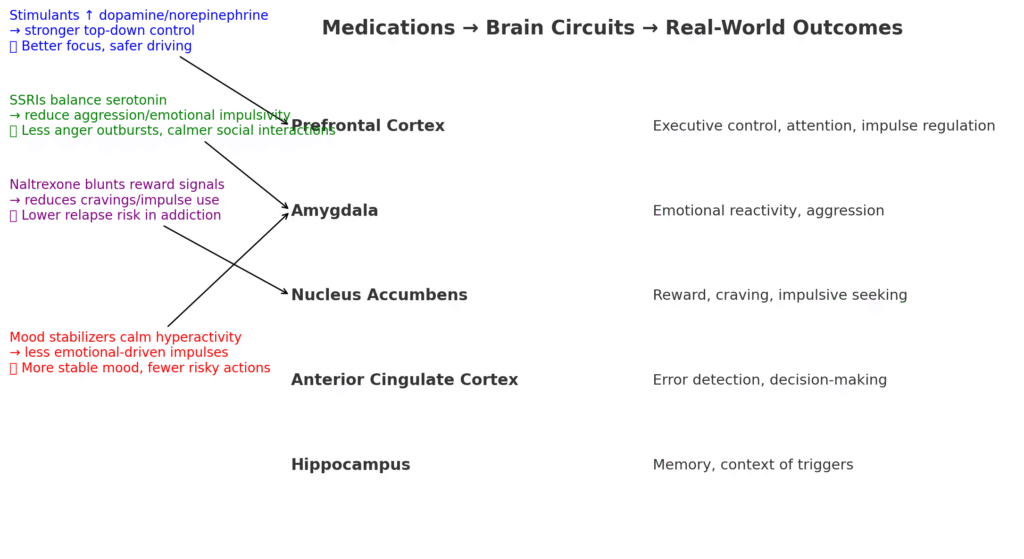
Question: Provide a real-world outcome (e.g., “reduced relapse,” “safer driving,” “less aggression”)
Answer: Brain-to-behavior diagram:
- Stimulants → strengthen prefrontal cortex → ✅ better focus, safer driving.
- SSRIs → calm amygdala → ✅ fewer anger outbursts, calmer social interactions.
- Naltrexone → blunts reward signals in nucleus accumbens → ✅ lowers relapse risk.
- Mood stabilizers → regulate emotional circuits → ✅ more stable mood, fewer risky actions.
Question: Why is ADHD more common in individuals with addiction?
Answer: ADHD Is More Common in People with Addiction.
Family and Genetics
ADHD and addiction both run in families. Genes that affect dopamine can make someone more likely to have ADHD and a higher risk for addiction.
Brain Chemistry
ADHD and addiction both involve problems with the brain’s reward system. People with ADHD often have lower levels of dopamine, the “feel-good” chemical. Drugs and alcohol boost dopamine so that they can feel extra rewarded for someone with ADHD.
Impulsivity
People with ADHD tend to act quickly without thinking things through. That makes them more likely to try drugs or alcohol and less likely to stop once they start.
Self-Medication
Sometimes, people with ADHD use substances to cope with their symptoms. For example, stimulants like nicotine or cocaine can make them feel more focused, while alcohol or cannabis may calm them down. But this often leads to misuse.
Stress and Struggles
ADHD can make school, work, and relationships harder. Stress, frustration, and rejection can push people toward drugs or alcohol as a way to cope.
Conclusion
The link between impulse control, attention deficits, and addiction highlights how deeply brain pathways, behavior, and environment are connected. While medication can help regulate focus and reduce impulsivity, real progress requires consistent self-management, such as building routines, practicing coping skills, and setting healthy goals. Family support strengthens resilience by offering stability and encouragement, while community resources—like peer groups, counseling, and educational programs—extend a safety net beyond the home. Together, these strategies create a comprehensive framework that empowers individuals not only to manage addiction but also to improve attention and impulse control for long-term recovery.
Videos: Addiction Expert Reveals Top Techniques to Regain FOCUS and Control IMPULSIVITY,
5 Easy Habits to Beat Impulsivity Fast