If you’re caring for someone close who’s struggling with substance use, the idea of them having an overdose can be frightening. I know that feeling of wanting to do everything you can, just in case something goes wrong. Getting prepared ahead of time isn’t about expecting the worst; it’s about making sure you’re ready to respond effectively if needed. Here’s how I’ve learned to prepare for a drug overdose from an addicted loved one, and what you might want to consider.
Understanding Overdose Risk in Loved Ones with Addiction
Knowing how and why overdoses can happen is a really important first step. Overdose risk shows up in a few different ways, depending on the substance used, changes in tolerance, and even what someone might mix together. Opioids like heroin, prescription painkillers, and even fentanyl are the most commonly linked to fatal overdoses, but danger can also come from mixing drugs or using unfamiliar supplies.
Relapses, changes in life stress, or getting new drugs from a different source might all bump up the odds. Many overdoses happen right after a period of not using, since tolerance drops. Even someone who looks healthy or seems to be “doing better” can still be at risk. If a person has recently left a rehab program or jail, their body’s tolerance can be much lower than expected, making any use much riskier. Knowing these patterns helps you stay alert and ready to step up if something feels off.
What to Look For: Signs of an Overdose
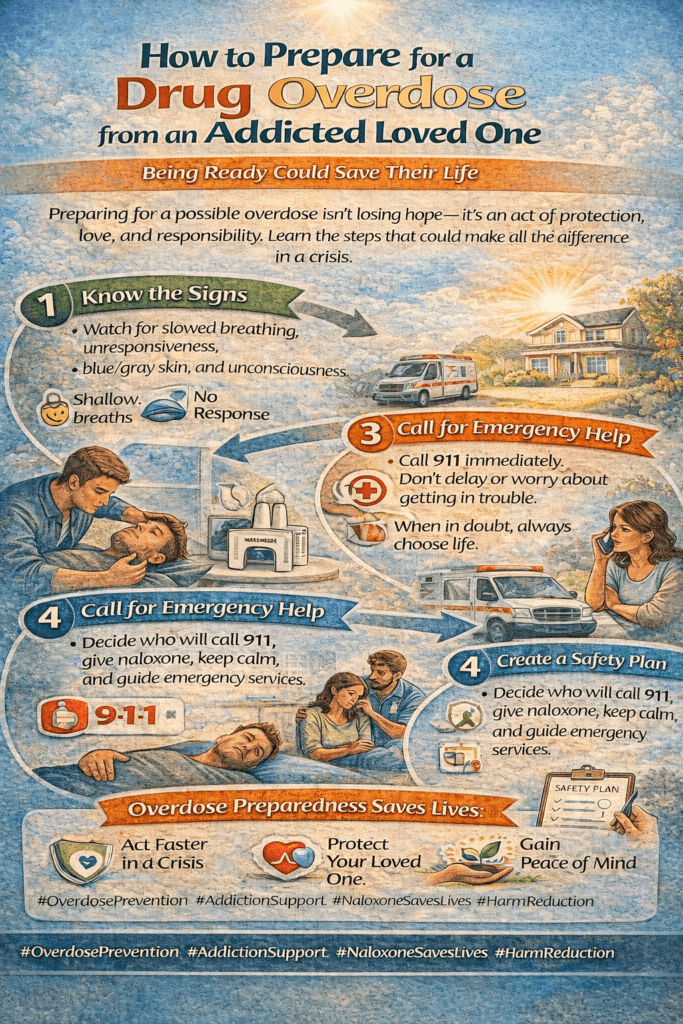
Recognizing an overdose quickly makes a huge difference in the outcome. Some signs can be subtle, so trusting your gut and looking for changes is pretty handy. Here are some key symptoms I always keep an eye out for:
- Loss of consciousness or unresponsiveness: Not waking up or responding to your voice or touch is a major red flag.
- Slow, irregular, or stopped breathing: Gasping, gurgling, or very shallow breathing means there’s an emergency.
- Pale, clammy, or bluish skin, lips, or fingernails: When oxygen drops, skin often changes color, especially around lips and fingertips.
- Snoring or choking sounds: Some overdoses sound like deep snoring or gurgling, called a “death rattle.”
- Pupils looking tiny (pinpoint) or wide/open, depending on the drug: Opioids usually cause pinpoint pupils, but other substances may have the opposite effect.
Noticing these details fast gives you the best shot at helping in time. It is also important to remember that each individual could react differently, and sometimes the warning signs may not be obvious. If you’re ever uncertain, it’s safest to treat the situation as a possible overdose.
Getting Prepared: Steps to Take Before an Emergency
Being prepared before an overdose happens can really save lives. Here are the top things I keep on hand and lines of action I find most useful:
- Get Naloxone (Narcan): This medication reverses opioid overdoses and can be a true lifesaver. Many pharmacies sell naloxone without a prescription, and some local groups offer free kits and training. I always check the expiration date and keep at least two doses in the house and car.
- Learn How to Use It: Watching a quick video or attending a local training helps a lot. You’ll practice using nasal spray or injectables. Easy-to-follow instructions come with most kits, so it’s not too complicated once you know how it works.
- Build an Emergency Response Kit: In addition to naloxone, I include gloves, a rescue breathing mask, hand sanitizer, and a printed step-by-step instruction sheet for responding to overdoses. Keeping everything in one place, easy to grab, helps when you’re in a rush.
- Share the Plan with Others: Family members, roommates, and even frequent visitors should know where the kit is and how to use it. I make sure to mention this, even if it feels awkward, since teamwork matters during emergencies.
- Have Emergency Numbers Ready: Program local emergency lines into your phone. Having numbers handy saves time when seconds count.
Extra preparation can also include regular check-ins with your loved one about how they’re feeling and what’s going on in their life. Set up a routine of reviewing your emergency supplies every few months and re-read the instructions with any household members who might assist in an emergency. You may also consider keeping some form of visible written instructions in a prominent spot. All these steps help create a safer and calmer environment if an urgent situation ever occurs.
Talking to Your Loved One About Overdose Risk and Safety
Even though it’s a tough subject, I find that starting an open, nonjudgmental chat about overdose and safety often helps. Instead of laying down the rules or voicing only your worries, I try to listen and make the goal all about keeping everyone as safe as possible.
It’s not always easy, especially if your relationship feels strained. I often stick with clear statements, like “I care about you and want you to be safe—would you be willing to help me practice what to do if something happens?” Some people push back at first, but most appreciate that you’re watching out for them deep down. Sharing stories from others who’ve faced emergencies can help break the ice and make the discussion feel less personal or confrontational. You can also bring pamphlets or information from respected organizations to the conversation, showing this is about health, not judgment.
How to Respond in an Overdose Emergency
Responding to an overdose can feel overwhelming, but acting quickly makes a big difference. Here’s the approach I’d suggest, which matches guidance from organizations like the Substance Abuse and Mental Health Services Administration (SAMHSA) and Harm Reduction Coalition:
- Check Responsiveness: Gently shake their shoulder or call out their name. If there’s no response, it’s time to act.
- Call 911: Always get emergency services on the way, even if you give naloxone. Provide the dispatcher with clear details on your location and what you suspect happened.
- Administer Naloxone: Follow the kit instructions for nasal sprays or injectable naloxone. Use the second dose if there’s no improvement within 2 to 3 minutes.
- Support Breathing: If the person isn’t breathing properly, start rescue breaths using a mask if available. Give one breath every five seconds if you’ve been trained and keep their airway open.
- Monitor and Comfort: Stay with them and watch for any changes. Recovery can take a few minutes. Sometimes, people wake up confused or upset, but that’s normal. If they start breathing normally, turn them on their side (the recovery position) to keep the airway clear.
I’ve read lots of stories online and heard from people in the recovery community that waiting to call for help is one of the most common mistakes, so I always try to act quickly. Good Samaritan laws often protect those who call for help, but the specifics vary with location.
If you’re ever worried about what to say when calling emergency services, just describe what’s happening: “My friend isn’t responding and is barely breathing after taking drugs.” This clears up any confusion for professionals and helps move things fast. Remember, your calm presence and willingness to act can make a life-saving difference.
Common Challenges and Safety Considerations
Having naloxone or an emergency kit isn’t the whole picture. Sometimes you’ll face real challenges, so staying aware of the bigger situation helps. Here are some things I keep in mind and often talk about with others in the same boat:
- Access to Supplies: Some places don’t have naloxone as easily available. Checking with local health departments, harm reduction groups, or even mail-order programs can fill the gap.
- Stigma and Shame: This can keep people from asking for help or even carrying naloxone. I try to keep the conversation grounded in health and safety, not blame or judgment.
- Multiple Substances: Overdoses get complicated when more than one drug is in the mix, like opioids and benzodiazepines. Still, naloxone is always worth giving for any suspected opioid involvement.
- Personal Safety: Sometimes people become disoriented or agitated after naloxone. I give space and approach calmly to keep the environment as safe as possible.
Other safety considerations include recognizing the potential for accidental exposure to fentanyl or other potent substances. Wearing gloves and washing your hands before and after responding reduces risk. If you notice drug residue on surfaces, be extra careful and avoid touching your face during the response.
Tips for Long-Term Preparation and Support
Being ready for an overdose is part of the adventure, not the endpoint. Here are a few things I focus on to stay ready over time:
- Check and Replace Supplies: Naloxone expires, so I set reminders to get fresh kits yearly. I also restock masks, gloves, and first-aid supplies.
- Keep Learning: Online organizations like Harm Reduction Coalition and SAMHSA have really helpful videos, guides, and updates on new overdose interventions. Signing up for their newsletters keeps you in the loop when guidelines change.
- Stay Connected: Support groups, harm reduction programs, and counseling services offer both guidance and emotional backup for people in your situation. These places can address questions about mental health, trauma, stress, and everything in between. Joining an online community can help lessen isolation and keep you informed on best practices in your area.
- Be Kind to Yourself: Even the best plan can’t control everything. Taking breaks, checking in with your own mental health, and reaching out for professional help when needed can make a huge difference for both you and your loved one. Remember, you’re only human, and getting support is a sign of strength, not weakness.
You can also make a habit of attending local harm reduction workshops when they’re offered. These events sometimes include first aid courses, opportunities to talk with people who’ve been through similar situations, and practical demonstrations. Each bit you learn adds to your comfort level in case of a real emergency.
Frequently Asked Questions
Some questions come up a lot for people preparing for a possible drug overdose at home. Here’s what I usually hear:
Question: Can I get in trouble for calling 911 during an overdose?
Answer: Most states have Good Samaritan laws to protect you from legal problems when asking for medical help during an overdose. Local rules vary by state, so checking state resources is a good idea.
Question: How do I get naloxone, and is it hard to use?
Answer: Many major pharmacies stock naloxone, and some areas give it out for free at health clinics. Using it gets easier with practice, and most kits come with simple instructions. Free videos online show you the steps if you want to rehearse.
Question: What if my loved one refuses help?
Answer: This is super common. Keeping naloxone close and responding during an emergency is always the right move, even if the person is not open to discussing it beforehand. Harm reduction works best when you lead with respect and kindness, no matter the situation.
Question: Do I need special training to help during an overdose?
Answer: While formal training is helpful, it’s not required. Many naloxone kits include clear, simple instructions, and online tutorials are widely available. Even without special classes, following the steps as best you can matters most. Never let the lack of training keep you from acting.
Resources to Support Overdose Preparedness
Lots of trustworthy organizations offer training, support, and up-to-date info. Here are a few that I recommend bookmarking or reaching out to:
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- Harm Reduction Coalition
- Centers for Disease Control and Prevention (CDC) – Overdose Prevention
Being informed, prepared, and compassionate goes a long way when you’re supporting someone through addiction. Every bit of preparation helps when facing tough situations, and the right resources can give you confidence to handle whatever comes your way. Wrapping up, knowing how to prepare and respond could save a life, and your willingness to jump in makes all the difference for your loved one.
Video: This Could Save Their Life During an Overdose #AddictionSupport #HarmReduction #MentalHealth