Tobacco use, known for its links to lung cancer and respiratory diseases, extends its impact to various health conditions, medication interactions, and disparities across diverse populations. This complex interplay emphasizes the need to understand gender-specific consequences and variations among racial and ethnic groups. Beyond immediate health risks, tobacco’s influence on medication effectiveness adds complexity, requiring comprehensive approaches that consider individual differences, cultural nuances, and equitable access to resources. This exploration navigates the intricate landscape of tobacco-related health conditions, medication effects, and disparities, calling for tailored interventions for optimal public health outcomes.
The Health Issues of Tobacco Use: Short and Long-Term Consequences
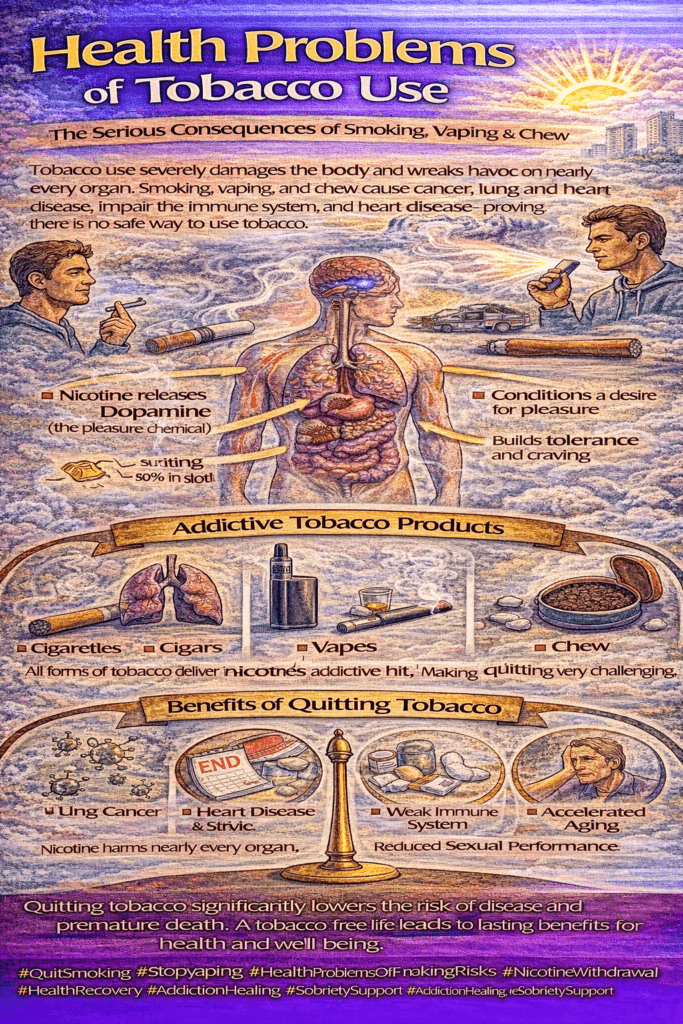
Tobacco use has well-documented health impacts, ranging from immediate, short-term effects to serious long-term consequences. Understanding these effects can help individuals make informed decisions about their health and encourage them to seek support in quitting. Here’s a breakdown of the short-term and long-term health consequences associated with tobacco use.
Short-Term Health Consequences of Tobacco Use
- Fatigue and Loss of Stamina: Tobacco smoke reduces oxygen levels in the bloodstream and increases carbon monoxide, which can lead to fatigue and reduced stamina. Smokers often experience decreased physical endurance and frequent fatigue due to these changes in oxygen levels.
- Coughing and Respiratory Irritation: Tobacco smoke irritates the respiratory system, leading to coughing and throat irritation. In the short term, smokers may develop a persistent cough as the body tries to expel harmful substances from the airways.
- Reduced Immune Function: Smoking weakens the immune system, making individuals more prone to infections, especially respiratory infections. Smokers are at higher risk of colds, bronchitis, and other respiratory conditions due to immune system compromise.
- Decreased Sense of Taste and Smell: Chemicals in tobacco smoke can dull the senses of taste and smell by affecting the sensory receptors responsible for these perceptions. Many smokers notice a diminished appreciation for food flavors and scents.
- Delayed Wound Healing: Nicotine constricts blood vessels, reducing blood flow to tissues and impairing wound healing, increasing susceptibility to infection. Smokers may experience slower recovery from injuries or surgeries due to reduced circulation.
Long-Term Health Consequences of Tobacco Use
- Chronic Respiratory Conditions: Smoking is a leading cause of chronic respiratory conditions such as chronic bronchitis and emphysema. These conditions result in persistent coughing, shortness of breath, and often irreversible lung damage, limiting overall quality of life.
- Increased Risk of Cardiovascular Diseases: Long-term tobacco use significantly raises the risk of cardiovascular diseases, including coronary artery disease, heart attacks, and strokes. Smoking affects blood vessels and heart function, leading to a higher risk of these life-threatening conditions.
- Lung Cancer: Smoking is the primary cause of lung cancer, with long-term exposure to carcinogens in tobacco smoke drastically increasing the risk of this aggressive cancer. Lung cancer is one of the most serious outcomes of prolonged tobacco use.
- Increased Risk of Other Cancers: Beyond lung cancer, tobacco use is associated with various other cancers, including those of the mouth, throat, esophagus, pancreas, bladder, and cervix. The carcinogenic substances in tobacco affect multiple organs, elevating cancer risk throughout the body.
- Deterioration of Dental Health: Smoking contributes to dental problems such as gum disease, tooth decay, and tooth loss. Smokers also have a higher risk of oral cancers, which can severely impact quality of life and overall health.
- Reduced Lung Function: Over time, smoking causes a progressive decline in lung function, resulting in chronic obstructive pulmonary disease (COPD). COPD can significantly impact breathing and limit a person’s ability to engage in everyday activities.
- Complications in Pregnancy: Smoking during pregnancy increases the risk of preterm birth, low birth weight, and developmental issues in the child. It can also increase the likelihood of miscarriage and other pregnancy-related complications.
- Accelerated Aging: Long-term smoking reduces blood flow and oxygen supply to the skin, leading to premature aging. Smokers often develop wrinkles, fine lines, and a dull complexion much earlier than nonsmokers, as well as other signs of skin damage.
The health consequences of tobacco use range from immediate effects, like coughing and fatigue, to severe, long-term impacts, including cancer, cardiovascular disease, and chronic respiratory conditions. Quitting smoking brings both immediate and long-term health benefits, including improved stamina, better immune function, and a significantly lower risk of life-threatening diseases. By choosing a tobacco-free lifestyle, individuals can take a proactive step toward better health and longevity. Support from healthcare providers, family, and community resources can provide essential guidance and encouragement to help individuals quit smoking and embrace a healthier life.
The Less Obvious Health Consequences of Tobacco Use
While the major health risks of tobacco—such as lung cancer and heart disease—are well-known, there are many other, less obvious health consequences of smoking and tobacco use. These impacts, though less prominent, can significantly affect quality of life and overall health. Here’s a look at some of the lesser-known effects of tobacco use.
1. Gum Disease (Periodontitis)
Smoking is a significant risk factor for gum disease, contributing to gum inflammation, bone deterioration, and a higher likelihood of tooth loss. Tobacco hinders healing in the mouth, leading to periodontal disease that, over time, can result in serious oral health issues and even tooth loss.
2. Cervical Cancer
Women who smoke have a heightened risk of cervical cancer. Smoking can contribute to the persistence of HPV (human papillomavirus) infections, a primary cause of cervical cancer, by compromising the body’s ability to clear the infection effectively.
3. Infertility in Men and Women
Tobacco use is associated with reduced fertility in both genders. In men, it impacts sperm quality and production, while in women, it can disrupt the menstrual cycle and increase the likelihood of pregnancy complications.
4. Loss of Vision
Smoking accelerates the progression of age-related macular degeneration (AMD), a leading cause of vision loss in older adults. The chemicals in tobacco can damage the eyes, leading to impaired vision and, in advanced cases, blindness.
5. Intervertebral Disc Degeneration
Smokers are at higher risk for intervertebral disc degeneration, which can contribute to chronic back pain and severe spinal issues like herniated discs and spinal stenosis. Smoking affects circulation and the body’s ability to repair the spinal discs.
6. Diabetes Complications
Smoking complicates diabetes management by increasing the risks of cardiovascular disease, kidney problems, and poor circulation. These effects can slow wound healing, leading to severe complications, including the need for amputations in some cases.
7. Rheumatoid Arthritis
Tobacco use has been linked to the development and worsening of rheumatoid arthritis. Smoking may intensify joint pain, stiffness, and swelling, leading to an accelerated progression of this autoimmune condition and impacting joint health and mobility.
8. Erectile Dysfunction
Smoking is a known risk factor for erectile dysfunction (ED) due to its effects on blood flow. Poor blood circulation, aggravated by tobacco use, can make it difficult for men to achieve and maintain an erection, impacting sexual health and relationships.
9. Complications in Pregnancy
Beyond the commonly known risks, smoking increases the likelihood of complications like placental abruption, where the placenta separates from the uterine wall, and premature rupture of membranes, leading to risks during labor and delivery.
10. Osteoporosis
Tobacco contributes to decreased bone density, especially in postmenopausal women, increasing the risk of osteoporosis and fractures. By affecting bone health, smoking accelerates the natural loss of bone density and raises the risk of debilitating bone injuries.
11. Compromised Immune Function
Smoking weakens immune defenses, making smokers more vulnerable to infections like respiratory infections and other illnesses. A suppressed immune system means a reduced ability to fight off infections and an increased risk of illness.
In summary, recognizing these lesser-known health consequences is essential for individuals to understand the full impact of tobacco use on the body. Each cigarette contributes to a broad range of health risks, some immediate and others developing over time. Quitting smoking can significantly reduce these risks, leading to improved overall health and a better quality of life. By becoming aware of these hidden dangers, smokers may feel more motivated to seek support, make informed choices, and work toward a healthier, tobacco-free future.
The Impact of Smoking on Individuals with HIV/AIDS and Hepatitis C Virus (HCV)
For individuals living with chronic infections like HIV/AIDS and Hepatitis C Virus (HCV), smoking significantly increases health risks and complicates the management of these conditions. Smoking exacerbates the already fragile health of individuals with compromised immune systems, impacting disease progression, treatment effectiveness, and the overall quality of life. Here’s an overview of how smoking specifically affects people with HIV/AIDS and HCV.
Smoking and HIV/AIDS
- Increased Risk of Opportunistic Infections Smoking impairs immune function, heightening the risk of opportunistic infections for those with HIV/AIDS. Because the immune system is already compromised, smoking further weakens the body’s ability to fight infections, potentially speeding up disease progression.
- Accelerated Progression of HIV/AIDS Research indicates that smoking may lead to faster progression of HIV/AIDS, increasing the severity of symptoms and worsening the overall health status of affected individuals.
- Higher Rates of Co-Existing Conditions. People with HIV/AIDS who smoke have a greater likelihood of developing co-existing conditions, including cardiovascular disease, respiratory issues, and certain types of cancer. Smoking adds to the burden of these health complications, often requiring more intensive medical management.
- Reduced Effectiveness of Antiretroviral Therapy (ART) Smoking can impact the effectiveness of antiretroviral therapy (ART), the primary treatment for HIV/AIDS. ART relies on optimal body functioning to manage the virus effectively, but smoking may interfere with its efficacy, leading to suboptimal outcomes.
- Increased Risk of Cardiovascular Disease. Individuals with HIV/AIDS already face an elevated risk of cardiovascular diseases due to the infection and certain antiretroviral medications. Smoking further amplifies this risk, increasing the likelihood of heart attacks, strokes, and other cardiovascular complications.
Smoking and Hepatitis C Virus (HCV)
- Accelerated Liver Disease Progression. Smoking exacerbates liver disease progression in people with HCV by increasing liver inflammation and fibrosis. Over time, this can lead to severe liver damage, hastening the onset of cirrhosis and other liver-related conditions.
- Reduced Response to HCV Treatment. Smokers with HCV tend to have a diminished response to antiviral treatment compared to non-smokers. Quitting smoking can improve the likelihood of successful treatment outcomes, enhancing the effectiveness of medications aimed at managing HCV.
- Increased Risk of Liver-Related Complications. Smoking raises the risk of severe liver-related complications, such as cirrhosis and liver cancer, in those with HCV. This risk compounds the already high likelihood of liver issues in this population, emphasizing the need for smoking cessation.
- Interactions with Medications. Smoking can alter how the body processes medications used to treat HCV, impacting drug metabolism and reducing treatment efficacy. For people with HCV, careful medication management becomes even more critical if they continue to smoke.
- Impact on Liver Transplantation. For those with advanced liver disease due to HCV, smoking can jeopardize liver transplantation outcomes. Smokers face a higher risk of graft failure and post-transplant complications, making smoking cessation essential for successful recovery.
The Importance of Smoking Cessation for HIV/AIDS and HCV Patients
Quitting smoking can have a transformative effect on the health outcomes of people with HIV/AIDS and HCV. By quitting, individuals can slow disease progression, improve treatment effectiveness, and reduce the risk of associated complications. Healthcare providers play a vital role in supporting smoking cessation efforts, helping individuals achieve better overall health and quality of life. For those managing these chronic infections, quitting smoking is one of the most powerful steps they can take to improve their health trajectory.
How Smoking Affects Medication Efficacy and Dosage Requirements
Smoking can have a surprising impact on the efficacy of various medications, often requiring adjustments in dosage. This interaction occurs because certain compounds in tobacco smoke can induce or inhibit liver enzymes, which play a critical role in metabolizing many medications. Here’s a breakdown of how smoking affects commonly prescribed drugs across several medication categories.
1. Anti-Anxiety Medications
- Benzodiazepines (e.g., Diazepam, Alprazolam): Smoking accelerates the metabolism of benzodiazepines in the liver, reducing their effectiveness. For individuals who smoke, healthcare providers may need to adjust dosages to ensure adequate therapeutic effects.
2. Antidepressants
- Selective Serotonin Reuptake Inhibitors (SSRIs): Smoking can increase the liver metabolism of certain SSRIs, leading to lower levels of the drug in the bloodstream and potentially reducing their effectiveness in managing symptoms of depression.
- Tricyclic Antidepressants (TCAs): Similar to SSRIs, smoking can stimulate liver enzymes responsible for metabolizing TCAs, resulting in lower drug levels. Patients who smoke may need higher doses to achieve the intended effects.
3. Anti-Psychotic Medications
- Typical and Atypical Antipsychotics (e.g., Olanzapine, Risperidone): Smoking induces liver enzymes that break down these medications, which can reduce blood levels and effectiveness. Regular assessment and dosage adjustments may be required for smokers.
4. HIV Treatment Medications
- Protease Inhibitors (e.g., Ritonavir, Atazanavir): Smoking impacts the metabolism of protease inhibitors, which are crucial in HIV treatment. Alterations in drug levels due to smoking can affect therapeutic outcomes, often necessitating dosage changes.
5. Insulin
- Insulin: Smoking affects insulin sensitivity, making blood sugar regulation more challenging for people with diabetes. Smokers with diabetes may require more frequent adjustments in insulin dosage to maintain optimal blood sugar levels.
6. Oral Contraceptives
- Combined Oral Contraceptives (COCs): Smoking, especially in women over 35, greatly increases the risk of cardiovascular complications such as blood clots when combined with COCs. For women who smoke, healthcare providers often recommend alternative contraceptive methods to reduce these risks.
7. Warfarin (Anticoagulant)
- Warfarin: Smoking stimulates liver enzymes that metabolize warfarin, potentially altering its blood levels and effectiveness. Regular INR (International Normalized Ratio) monitoring is essential for smokers to ensure that warfarin is providing the intended anticoagulant effect.
8. Theophylline (Bronchodilator)
- Theophylline: Smoking increases theophylline metabolism, a medication often prescribed for respiratory conditions, leading to faster drug breakdown. Smokers taking theophylline may need higher doses to maintain therapeutic effects.
Importance of Informing Healthcare Providers About Smoking
Because smoking can significantly alter how the body processes medications, it’s crucial for individuals to disclose their smoking status to healthcare providers, as well as any changes in smoking habits. This information allows healthcare professionals to make informed decisions about medication regimens and adjust doses as needed. Quitting smoking is beneficial not only for overall health but also for ensuring that medications work as intended.
Gender-Specific and Racial/Ethnic Health Consequences of Tobacco Smoking
Tobacco use affects people across all demographics, but the specific health consequences often vary by gender, race, and ethnicity. Recognizing these differences is essential for developing effective, targeted strategies in tobacco prevention, cessation, and support.
Gender-Specific Health Consequences of Smoking
For Women:
- Reproductive Health: Smoking poses significant risks for reproductive health. In pregnancy, it’s linked to complications such as preterm birth, low birth weight, and developmental issues. It also increases infertility risk and can disrupt menstrual cycles.
- Cervical Cancer: Female smokers are at a heightened risk for cervical cancer. The combination of smoking and human papillomavirus (HPV) infection can increase the likelihood of developing this type of cancer.
- Early Menopause: Smoking can lead to an earlier onset of menopause, increasing women’s susceptibility to menopause-related health concerns like osteoporosis due to decreased bone density.
For Men:
- Erectile Dysfunction (ED): Smoking has been shown to increase the risk of erectile dysfunction due to its adverse effects on blood flow. Male smokers may experience reduced ability to achieve or maintain erections, a condition linked directly to the vascular impact of smoking.
Health Disparities Among Racial and Ethnic Groups
Different racial and ethnic groups experience unique challenges related to smoking, both in prevalence and health consequences.
African Americans:
- Lung Cancer Disparities: African American men, for instance, face a higher incidence of lung cancer compared to white men, despite generally lower smoking rates. This disparity may be attributed to genetic factors, secondhand smoke exposure, and differences in tobacco product use.
Hispanic/Latino Americans:
- Smoking Patterns: Smoking prevalence varies widely among Hispanic/Latino subgroups. For example, smoking rates are typically higher among Puerto Rican men and women compared to Mexican Americans. Tailored approaches are necessary to address the unique smoking trends within these subgroups.
Asian Americans:
- Tobacco Use Patterns: Asian American subgroups also show significant variability in smoking rates. For example, Southeast Asian men often report higher smoking rates than East Asian men, highlighting the need for culturally nuanced interventions.
Native Americans:
- High Smoking Rates: Native American populations often report higher smoking rates than other groups, influenced by historical, cultural, and socioeconomic factors. Addressing these disparities requires understanding and respecting cultural contexts, as well as providing targeted cessation support.
Health Disparities in Smoking-Related Diseases
Racial and ethnic groups may experience varying impacts of smoking-related diseases. For instance, cardiovascular diseases and respiratory illnesses are common among some populations, while others may see higher incidences of lung or oral cancers. These disparities emphasize the need for specialized health interventions and equitable access to resources.
Social and Cultural Influences on Smoking Behavior
Cultural and social factors strongly shape smoking behaviors. In some cultures, smoking may be normalized or even celebrated, while others discourage it. Culturally sensitive approaches that respect these nuances can be more effective in promoting cessation.
Access to Cessation Resources and Secondhand Smoke Exposure
- Barriers to Quitting: Access to cessation resources like counseling and nicotine replacement therapy varies widely. Racial and ethnic disparities in healthcare access can create barriers to quitting, underscoring the importance of ensuring equitable access to support services.
- Secondhand Smoke Exposure: Variability in exposure to secondhand smoke also exists across demographic groups. Households with smokers can pose health risks for non-smoking family members, including children and elderly individuals.
Moving Toward Culturally Tailored Solutions
Understanding and addressing the gender-specific and racial/ethnic disparities in tobacco-related health risks is critical to reducing the overall burden of smoking. By creating culturally informed interventions, healthcare providers and policymakers can contribute to more effective prevention and cessation efforts across diverse populations.
Frequently Asked Questions
Here are some common questions:
1. What are the main health problems caused by tobacco use?
Tobacco use increases the risk of cancer, heart disease, stroke, lung disease, diabetes, and weakened immune function.
2. Which cancers are linked to tobacco?
Lung, mouth, throat, esophagus, stomach, pancreas, kidney, bladder, and cervical cancers are strongly associated with tobacco use.
3. How does tobacco damage the lungs?
It destroys air sacs, inflames airways, increases mucus production, and reduces oxygen exchange, leading to chronic bronchitis, emphysema, and COPD.
4. How does tobacco affect the heart?
Nicotine raises blood pressure and heart rate, while carbon monoxide reduces the amount of oxygen in the blood. This increases the risk of heart attacks and strokes.
5. Can smoking cause breathing problems even in young people?
Yes. Young smokers often develop chronic cough, shortness of breath, and reduced athletic performance.
6. Does tobacco affect mental health?
Yes. Long-term tobacco use is linked to higher rates of anxiety, depression, and mood instability.
7. What effect does tobacco have on the immune system?
It weakens the immune response, making the body more vulnerable to infections and slower wound healing.
8. How does tobacco affect the mouth and teeth?
It causes gum disease, tooth loss, bad breath, stained teeth, and oral cancers.
9. Can tobacco use affect pregnancy?
Yes. Smoking during pregnancy increases the risk of miscarriage, premature birth, low birth weight, and sudden infant death syndrome.
10. Is secondhand smoke harmful?
Yes. Secondhand smoke increases the risk of lung cancer, heart disease, asthma, and respiratory infections in children.
11. Does vaping cause similar health problems?
Vaping reduces exposure to some toxins but still delivers nicotine and harmful chemicals that affect lung, heart, and brain development.
12. How quickly does health improve after quitting?
Heart rate and blood pressure improve within days, lung function improves in weeks, and cancer risk decreases over the years.
13. Why is tobacco addiction difficult to quit?
It combines chemical dependence, behavioral habits, and emotional coping, making quitting challenging without support.
14. Are chewing tobacco products safer than smoking?
No. They increase the risk of mouth cancer, gum disease, and nicotine addiction.
15. What is the most important message about tobacco use?
Tobacco is one of the leading preventable causes of disease and death — quitting at any stage greatly improves health.
Conclusion
The multifaceted impact of tobacco use extends beyond the well-known risks, intertwining with medication effectiveness and revealing stark health disparities across diverse groups. The intricate relationship between tobacco-related health conditions, medication interactions, and disparities necessitates a holistic approach to public health. Tailored interventions that address gender-specific consequences, acknowledge cultural nuances, and ensure equitable access to resources are imperative. As we strive for healthier communities, understanding the intricate dynamics of tobacco-related health challenges, their effects on medications, and the disparities that persist becomes paramount in shaping comprehensive strategies for prevention, cessation, and improved overall well-being. Only through a collective, nuanced effort can we hope to address the complex landscape that tobacco use introduces into public health.
Video: