Healpods are new devices that create a calming space using lights, sounds, and other sensory tools to help people relax and manage stress. In addiction treatment, they are sometimes used to support recovery by reducing cravings and assisting people to feel more in control of their emotions. While some early results seem promising, Healpods also have drawbacks, including high cost, limited availability, and a lack of strong scientific evidence of effectiveness. There are also ethical concerns, such as whether everyone can access them fairly and whether it’s appropriate to use them before more research is done. Since Healpods are not FDA-approved and not covered by insurance, most people in treatment cannot easily use them.
Sensory Integration Treatment (SIT) in Addiction Recovery: How the HealPod Fits Into Broader Therapeutic Approaches
What Is Heal’s Sensory Integration Treatment (SIT)?
Heal, developed by SoundHeal, Inc., is a new form of Sensory Integration Treatment (SIT) designed for behavioral health and addiction recovery. The treatment is delivered through the HealPod, a compact 4×4-foot immersive space that combines sound, vibro-acoustic stimulation, light therapy, mindfulness, and journaling into short (~5-minute) therapeutic sessions.
Inside the HealPod, individuals can personalize their experience by selecting calming music, vibration settings, and light patterns. The goal is to support self-regulation, emotional balance, and readiness for traditional treatment programs such as counseling, group therapy, or medication-assisted recovery.
Reported Outcomes & Settings
A pilot program in San Luis Obispo County Juvenile Hall—including the Coastal Valley Academy and Phoenix programs—showed promising outcomes:
- 96% of participants reported that Heal sessions consistently supported their well-being.
- 99% said it helped them develop at least one coping skill.
- Reported benefits included reduced anxiety, stress, and depression, as well as improved focus, mood, self-esteem, and relaxation after sessions.
Additionally, Heal leverages generative AI to tailor treatment plans and evaluate progress through journaling data.
How This Relates to Traditional Sensory Integration Therapy (SIT)
Traditional SIT is most commonly used in pediatric settings for children with developmental disorders such as autism or ADHD. Delivered by occupational therapists, it often includes activities like:
- Play-based exercises
- Deep-pressure techniques
- Sensory brushing and weighted tools
- Swings or movement-based interventions
These approaches aim to improve sensory processing and emotional regulation.
By contrast, addiction-focused sensory interventions are emerging in clinical settings. Some treatment centers use multisensory rooms (“Snoezelen” environments) or sensory-friendly tools (weighted blankets, sound machines, soft lighting) to help individuals regulate emotions, manage cravings, and reduce the risk of relapse. For example, Iris Health Clinic in Wisconsin integrates sensory tools into addiction and mental health programs, while broader frameworks highlight the role of sensory health in relapse prevention.
Comparison at a Glance
| Support emotional regulation, coping, and motivation in addiction treatment.t | Traditional SIT (Child Development) | HealPod SIT (Addiction Recovery) |
|---|---|---|
| Purpose | Improve sensory processing, motor skills, and regulation in neurodiverse youth | Early pilot data in addiction/juvenile justice: promising but limited |
| Delivery | Therapist-led, play-based sensory activities | Brief immersive sessions with sound, vibration, light, mindfulness, journaling |
| Clients | Children with developmental disorders (ASD, ADHD, etc.) | Justice-involved youth and individuals in behavioral health programs |
| Reported Outcomes | Better sensory processing, motor skills, behavior | Reduced distress, stronger coping skills, improved engagement |
| Evidence Base | Established research in pediatrics (some RCTs, pilot studies) | Early pilot data in addiction/juvenile justice; promising but limited |
In summary, the HealPod represents a cutting-edge application of Sensory Integration Treatment in behavioral health and addiction. Unlike traditional SIT, which relies on play-based and therapist-led methods, Heal provides a short, immersive, AI-personalized experience designed to help individuals manage stress and engage more effectively in treatment.
Although the evidence is still emerging, early results are promising—especially for youth in high-stress recovery settings. If further validated through larger clinical trials, HealPods may become a valuable adjunct tool in addiction recovery, helping to reduce relapse risks and prepare individuals for deeper therapeutic engagement.
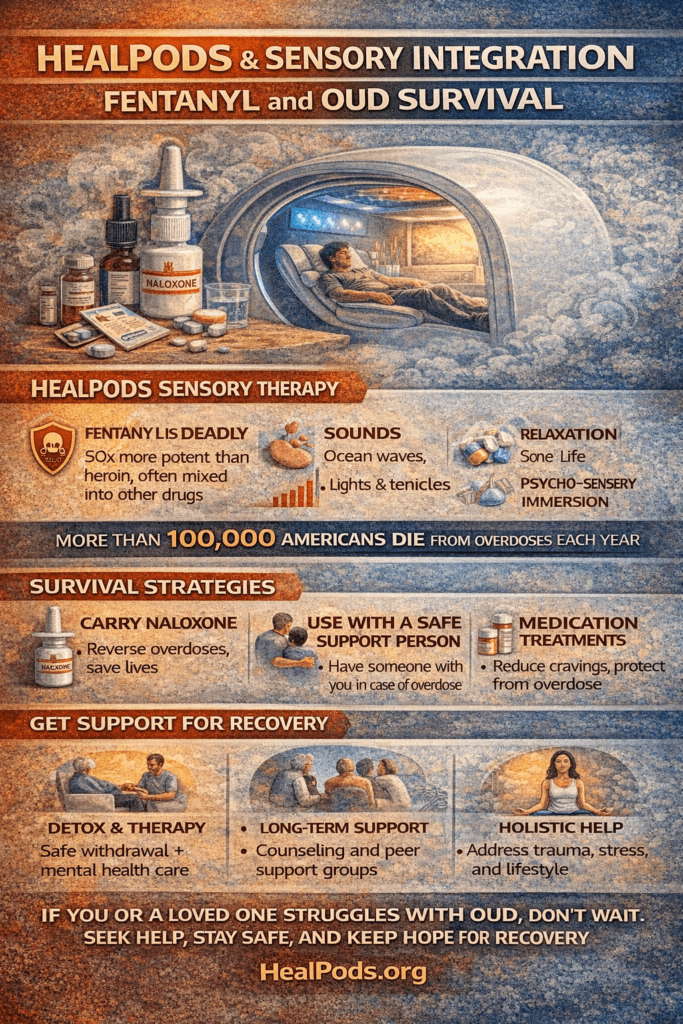
HealPods in Addiction Therapy: A Sensory Integration Approach to Recovery
Addiction treatment is evolving, and new tools are being designed to support patients beyond traditional therapy and medication. HealPods, created as part of Sensory Integration Treatment (SIT), are enclosed therapeutic spaces equipped with calming features such as sound therapy, aromatherapy, gentle lighting, tactile feedback, and even soft vibrations. Their goal is to help individuals regulate their nervous system, manage cravings, and find emotional balance in the midst of recovery.
How HealPods Work in Practice
1. Stress and Craving Regulation
By creating a controlled sensory environment, HealPods reduce stress responses and help individuals manage cravings—particularly useful during moments that might otherwise trigger relapse.
2. Emotional Self-Regulation
The combination of soothing lights, gentle vibrations, and calming sounds activates the body’s natural relaxation response, easing anxiety, agitation, or mood swings.
3. Enhancing Therapy Engagement
For patients who struggle to focus in traditional counseling, HealPods can be used before or after therapy sessions to help them be more attentive and emotionally present.
4. Coping Skills Training
Some treatment programs integrate HealPod use into relapse-prevention plans, teaching patients to turn to the pod as a healthier coping tool instead of substances when under stress.
5. Neurobiological Reset
Grounded in SIT theory, HealPods aim to retrain the brain’s stress pathways by engaging multiple senses in a structured and calming way, potentially strengthening long-term resilience against relapse.
A Reset Space in Treatment
Think of a HealPod as a therapeutic “reset space” inside treatment centers—a safe place where patients can step away, calm down, and restore balance before re-engaging in group or individual therapy. While research is still growing, many programs report that these pods can increase self-regulation, reduce emotional overload, and improve readiness for recovery work.
Scientific Evidence and Limitations of HealPods in Addiction Therapy
The treatment of addiction increasingly includes complementary and technology-assisted interventions designed to help patients regulate stress, manage cravings, and stay engaged in recovery. HealPods, which apply Sensory Integration Treatment (SIT) principles, are one such innovation. These enclosed pods use sound therapy, vibro-acoustic stimulation, calming lights, and mindfulness prompts to create short, structured sensory sessions. While early results are promising, the evidence base is still developing.
Scientific Evidence Supporting HealPods
Sensory Integration Treatment (SIT) Research
SIT has been widely studied in occupational therapy, particularly for conditions like autism, PTSD, and anxiety. Research shows that structured sensory input can regulate arousal, stabilize mood, and reduce stress reactivity. These mechanisms are directly relevant to addiction, where stress and emotional dysregulation are primary relapse triggers.
Mind-Body Interventions
Evidence from mindfulness, meditation, and biofeedback suggests that controlled sensory environments help improve impulse control and manage cravings. HealPods can be seen as a tech-enabled, structured version of these practices.
Trauma-Informed Care
Many people with substance use disorders have trauma histories. The enclosed, safe, and predictable environment of a HealPod may reduce hyperarousal and provide grounding, making it especially relevant for trauma-sensitive addiction care.
Adjunct to MAT and CBT
Preliminary pilot programs, though still limited, suggest that HealPods may enhance patient readiness for therapy and reduce anxiety, thereby improving engagement in counseling, group therapy, and medication-assisted treatment (MAT).
Limitations & Gaps in Evidence
Limited Clinical Trials
Most research so far comes from small-scale or observational studies, many outside addiction care (e.g., autism, PTSD). There are no large randomized controlled trials yet demonstrating HealPods’ impact on relapse rates.
Short-Term vs. Long-Term Benefits
Evidence points to immediate calming effects, but it remains unclear whether these translate into sustained recovery outcomes such as reduced relapse over months or years.
Placebo & Novelty Effects
Some patient improvements may stem from the novelty of the pods or the expectation of benefit, rather than the therapeutic mechanisms themselves.
Accessibility & Cost
HealPods are resource-intensive, limiting their availability in low-resource or community-based treatment programs. Equity and scalability remain significant challenges.
Risk of Over-Reliance
While effective for calming, pods may unintentionally encourage external dependence for regulation. For best results, they must be paired with cognitive-behavioral therapy (CBT), skill-building, and peer recovery supports to strengthen internal coping mechanisms.
In summary, healPods show significant promise as adjunctive tools for addiction treatment, drawing on established evidence from SIT, mindfulness practices, and trauma-informed care. They can help regulate stress, manage cravings, and prepare patients for deeper engagement in therapy. However, without large-scale trials and clear cost-access models, HealPods should be used as supplements—not substitutes—for evidence-based approaches such as MAT, CBT, and peer support programs. Continued research will determine whether these innovative tools can find a permanent place in mainstream addiction care.
Potential Disadvantages of HealPod’s Sensory Integration Treatment (SIT) Approach in Addiction Therapy
The HealPod offers a novel, tech-enabled version of Sensory Integration Treatment (SIT), aiming to help individuals in addiction recovery regulate stress, manage cravings, and improve emotional balance. While early pilot programs show encouraging feedback, there are essential limitations and concerns to consider. Understanding these potential disadvantages ensures the HealPod is viewed as a supplementary tool—rather than a replacement—for evidence-based treatment.
1. Limited Evidence Base
The HealPod is supported mainly by pilot data and lacks large-scale, peer-reviewed studies specific to addiction recovery. Even traditional SIT has faced scrutiny, with the American Academy of Pediatrics noting that the evidence for sensory-based therapies remains limited and inconclusive beyond pediatric populations.
2. Risk of Over-Reliance
While the HealPod can provide immediate relief, there is a risk that individuals may grow dependent on its structured sensory environment for emotional regulation. This may slow the development of internal coping strategies, which are critical for long-term recovery.
3. Variable Comfort & Sensory Overload
Not everyone responds positively to sensory inputs like lights, vibrations, or sounds. For some, these stimuli may feel overwhelming or unpleasant, potentially leading to irritability, anxiety, or disengagement if sessions are not personalized carefully.
4. Ethical and Autonomy Concerns
Critics of sensory therapies raise ethical questions about autonomy. If HealPod sessions are viewed as directive or mandatory, individuals—particularly those in vulnerable settings like juvenile justice programs—may feel pressured rather than empowered, challenging the principles of informed consent and personal agency.
5. Focus on Symptoms Rather Than Root Causes
HealPods may help regulate stress and mood in the short term, but they do not directly address underlying trauma, co-occurring mental health conditions, or the neurobiology of addiction. Without integration into a broader treatment plan, the benefits may be temporary and surface-level.
6. Scalability and Access
Setting up HealPods requires financial investment, physical space, and staff training. For resource-limited clinics or rural areas, these barriers could prevent widespread access, raising equity concerns and creating gaps in continuity of care.
Summary Table
| Resources needed for pods may limit availability in many treatment settings. | Details |
|---|---|
| Limited evidence base | Early pilot data; broader SIT lacks strong conclusive support |
| Possible over-reliance | Risk of dependency on external sensory input instead of developing personal coping skills |
| Discomfort or overload risks | Not all users tolerate sensory input well; customization required |
| Ethical autonomy concerns | Structured sensory environments may feel coercive or limiting to participant control |
| Root cause not addressed | Focuses on regulation, not underlying trauma or addiction drivers |
| Accessibility and cost issues | Resources needed for pods may limit availability in many treatment settings |
In summary, the HealPod represents a creative and promising approach to supporting addiction recovery through sensory-based interventions. However, its effectiveness is likely to be situational and supplemental. For best outcomes, it should be integrated into comprehensive treatment plans that include evidence-based therapies such as medication-assisted treatment (MAT), cognitive-behavioral therapy (CBT), and peer recovery support. As research grows, careful monitoring of individual responses and ethical implementation will determine whether HealPods become a sustainable part of addiction care.
Ethical Dilemmas of HealPod’s Sensory Integration Treatment (SIT) in Addiction Care
As behavioral health continues to explore new technologies, ethical concerns become especially important. HealPods, designed to deliver Sensory Integration Treatment (SIT) through immersive environments of light, sound, vibration, and mindfulness, represent an innovative approach to addiction therapy. Yet their novelty also raises complex ethical questions that providers, patients, and policymakers must consider.
1. Informed Consent & Transparency
Clients must clearly understand what a HealPod does, how it works, and what the evidence does—or does not—support. Because research is still limited, overstating effectiveness or failing to disclose uncertainties undermines informed consent. This is particularly concerning in vulnerable populations, such as individuals with addiction or trauma histories, who may feel pressured to participate without fully grasping risks or alternatives.
2. Autonomy vs. Control
Sensory immersion therapies can create strong emotional or physical effects. If patients feel confined or “controlled” by the pod environment, their autonomy may be compromised. In mandated treatment settings, such as court-ordered rehab, the structured nature of HealPod sessions risks being perceived as coercive rather than voluntary.
3. Equity & Access
Because HealPods are specialized and resource-intensive, they are more likely to be available in well-funded, urban facilities. This creates disparities in access, leaving lower-income or rural populations without equal opportunities for innovative care. From an ethical standpoint, this raises concerns about justice in who benefits from cutting-edge therapies.
4. Risk of Over-Promise
Marketing HealPods as “revolutionary” or “cutting-edge” can unintentionally raise false hope. Without large-scale clinical evidence, positioning them as central to recovery risks misleading patients and families—potentially diverting attention from proven treatments such as medication-assisted treatment (MAT) or cognitive-behavioral therapy (CBT).
5. Dependency vs. Empowerment
While HealPods may offer short-term relief, over-reliance on the sessions could discourage patients from developing their own coping skills. Ethically, providers must ensure that pods are used to support resilience, not replace the process of building internal strength and independence.
6. Privacy & Data Concerns
If HealPods collect biometric or psychological data—such as heart rate, mood, or journaling content—strict safeguards must protect confidentiality. Clear policies on data use, storage, and sharing are essential to prevent privacy breaches or the misuse of sensitive health information.
7. Opportunity Cost
HealPod sessions require time, space, and staff support. If not carefully integrated, they could displace participation in more evidence-based treatments. Ethically, providers must weigh whether these sessions enhance or compete with therapies that already have stronger clinical support.
In summary, the ethical dilemmas surrounding HealPods highlight the importance of informed consent, autonomy, equitable access, privacy, and responsible integration into care. While they may offer meaningful benefits as a supplemental tool for emotional regulation and stress management, they should never replace comprehensive, evidence-based addiction treatment. Careful implementation—grounded in transparency and ethical safeguards—will determine whether HealPods become a trusted complement to recovery programs or a source of unintended risk.
Healpods Enter Addiction Treatment: Practical Steps Toward Clinical Integration
Healpods, innovative sensory integration treatment pods, are poised to enter the landscape of addiction care. Before widespread adoption, they must navigate a series of practical, clinical, and policy steps to ensure effectiveness, safety, and accessibility.
1. Clinical Integration
Pilot programs in residential treatment centers, detox units, and intensive outpatient programs (IOPs) are the first step. Healpods should serve as adjunctive tools, complementing established treatments such as medication-assisted treatment (MAT), cognitive-behavioral therapy (CBT), contingency management, and peer support. Targeted sessions could help patients manage stress, regulate trauma responses, reduce cravings, or stabilize after withdrawal.
2. Training & Staffing
Staff must be trained in safe pod operation and in integrating the pod into treatment goals. Some patients may require guided sessions, incorporating mindfulness or trauma-informed strategies, while others could benefit from independent use. Counselors, occupational therapists, and peer specialists will play key roles.
3. Funding & Reimbursement
Early adoption will rely on demonstrating cost-effectiveness, such as lower relapse rates or shorter inpatient stays, to appeal to insurance providers and Medicaid. Grants from federal innovation programs such as SAMHSA and NIH, as well as support from private foundations, may help fund pilot programs. Healpods could also be integrated into bundled “whole-person care” billing models covering non-traditional supportive therapies.
4. Evidence & Research
Randomized controlled trials measuring craving reduction, relapse prevention, stress biomarkers, and patient satisfaction are critical. Standardized protocols—defining session length, frequency, and indications—will help build credibility. Peer-reviewed publications will support regulatory acceptance and broader clinical adoption.
5. Accessibility & Equity
Scalable, portable, or modular pod designs can make Healpods available to smaller clinics and community centers. Integration with telehealth could extend access to rural populations. Sliding-scale programs and nonprofit partnerships may ensure that uninsured or underinsured individuals can benefit.
6. Ethical & Policy Oversight
Clear informed consent protocols, cultural sensitivity adaptations, and adherence to regulatory standards—potentially through FDA classification as adjunctive wellness devices—will be essential for ethical integration.
✅ In Practice: With careful planning, evidence-based trials, and thoughtful integration, Healpods have the potential to enhance addiction treatment by offering patients a novel, supportive tool for recovery.
Healpods could be scheduled like group therapy or meditation sessions—patients sign up for 20–30 minutes of guided sensory regulation to reduce stress, improve emotional balance, and prepare for therapy engagement. Over time, if studies validate their benefits, insurance and Medicaid could fund them as recognized adjunctive therapies.
Frequently Asked Questions
Here are some common questions:
Question: Provide a sample framework showing how Healpods could be integrated into a daily addiction treatment program without replacing evidence-based care.
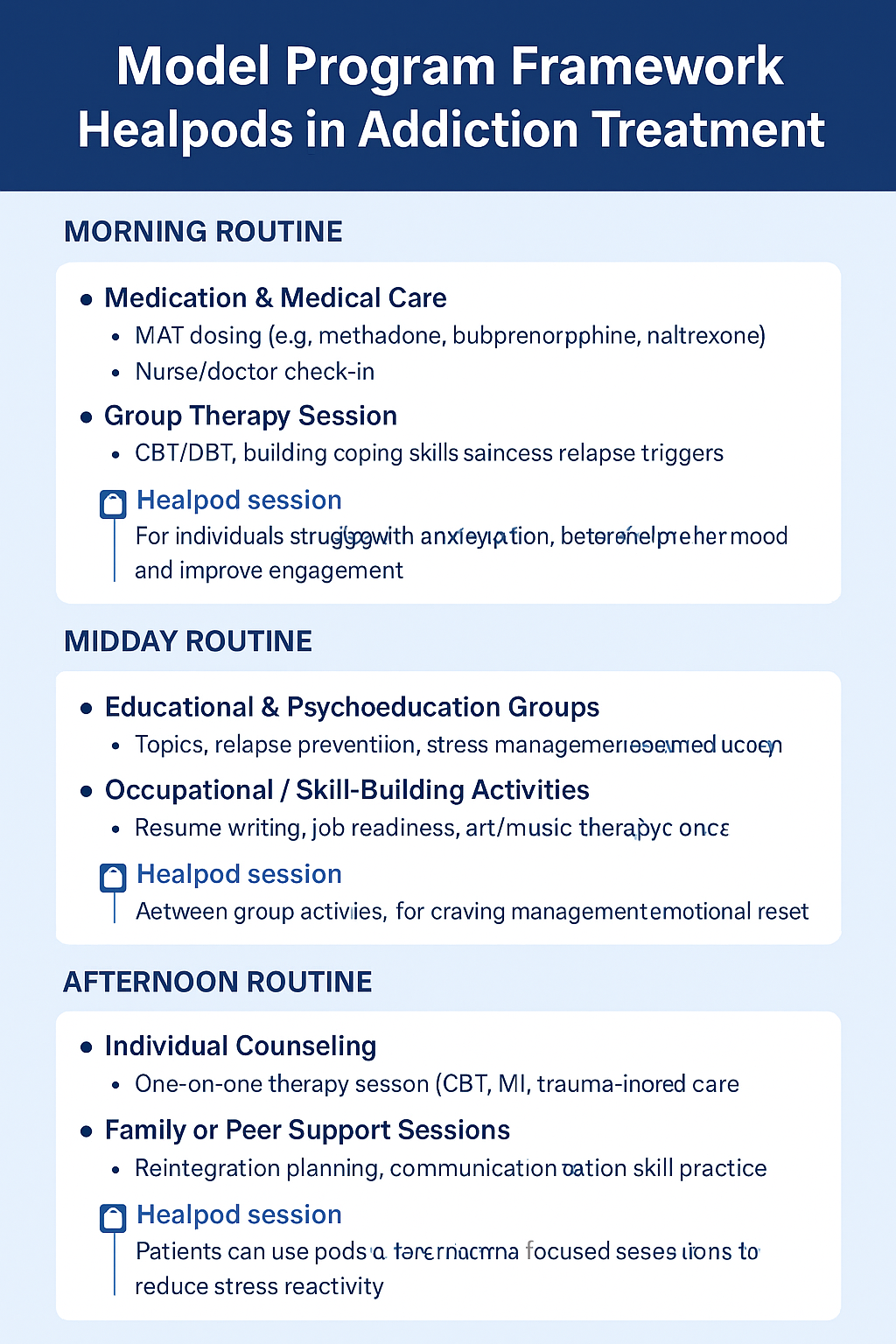
Answer: A sample framework showing how Healpods could be integrated into a daily addiction treatment program without replacing evidence-based care:
Model Program Framework: Healpods in Addiction Treatment
Morning Routine (8:00 – 10:00 AM)
- Medication & Medical Care
- MAT dosing (e.g., methadone, buprenorphine, naltrexone).
- Nurse/doctor check-in.
- Group Therapy Session (CBT/DBT focus)
- Building coping skills and addressing relapse triggers.
🔹 Optional Healpod session: For individuals struggling with anxiety before therapy to help regulate mood and improve engagement.
Midday Routine (10:30 – 1:00 PM)
- Educational & Psychoeducation Groups
- Topics: relapse prevention, stress management, trauma education.
- Occupational / Skill-Building Activities
- Resume writing, job readiness, art/music therapy.
🔹 Optional Healpod session: Scheduled between group activities for craving management and emotional reset.
Afternoon Routine (2:00 – 5:00 PM)
- Individual Counseling
- One-on-one therapy sessions (CBT, MI, trauma-informed care).
- Family or Peer Support Sessions
- Reintegration planning, communication skill practice.
🔹 Optional Healpod session: Patients can use pods before brutal family or trauma-focused sessions to reduce stress reactivity.
Evening Routine (6:00 – 8:00 PM)
- Community Integration Activities
- 12-Step meetings, SMART Recovery, peer groups.
- Recreation / Physical Wellness
- Gym, yoga, mindfulness, and outdoor activity.
🔹 Optional Healpod session: End-of-day relaxation or guided meditation pod session to improve sleep hygiene and reduce nighttime cravings.
Role of Healpods in the Program
✅ Adjunctive Tool, Not Replacement – used alongside MAT, counseling, and group therapy.
✅ Flexible Scheduling – patients opt in when stress, cravings, or emotional dysregulation peak.
✅ Therapeutic Goal-Oriented – staff guide pod use (stress relief, mindfulness, trauma grounding).
✅ Data-Driven – monitor outcomes like reduced cravings, improved therapy engagement, and sleep quality.
Question: Provide an infographic chart about the Healpod program in addiction treatment.
Answer: Chart of Healpod use in addiction treatment.
Question: Are HealPods FDA-approved, and can insurance cover the cost?
Answer: FDA approval status of Healpods and insurance coverage possibilities:
FDA Approval Status
As of now, Healpods are not FDA-approved:
- The FDA has not cleared any sensory integration pods or immersive multisensory environments, such as Healpods, for use in addiction treatment.
- The only FDA-approved devices in the addiction space are limited to digital therapeutics, such as:
- reSET®, cleared under the De Novo pathway in 2017 to support outpatient SUD treatment through CBT, and
- reSET-O®, cleared in 2018 for OUD treatment as an adjunct to buprenorphine and contingency management, Bynder.
Healpods currently fall outside of these recognized categories of medical devices or digital therapeutics, meaning they do not benefit from FDA validation or oversight.
Insurance Coverage Landscape
Since Healpods lack FDA approval, insurance coverage is unlikely at this stage:
- Coverage Is Typically Limited to Approved Treatments
- Health plans rarely reimburse for unapproved, experimental, or adjunctive therapies — especially those not recognized as medically necessary.
- Parity Laws and Essential Health Benefits
- The Affordable Care Act (ACA) mandates that mental health and SUD treatment are treated as essential benefits on HealthCare.gov.
- The Mental Health Parity and Addiction Equity Act ensures parity, meaning behavioral health services must be covered similarly to physical health services. But this applies only when services are recognized and evidence-based PMCEBSCOOASS.
- Unproven interventions like Healpods generally fall outside these protections.
- Barriers in Practice
- In reality, insurance coverage for SUD treatments faces barriers such as state-by-state Medicaid variability, restrictive definitions of medical necessity, reimbursement limits, and administrative hurdles—even for standard therapies, PMCEBSCO.
- Experimental tools like Healpods would likely encounter even greater difficulty gaining coverage.
Summary Table
| Aspect | Status for Healpods |
|---|---|
| FDA Approval | Not approved or cleared as a medical device |
| Insurance Coverage | Unlikely to be covered without FDA approval and evidence |
| Analogous Approved Devices | reSET®, reSET-O® are FDA‐cleared digital therapeutics |
In summary, Healpods are not FDA-approved, and without such designation, insurance companies are unlikely to cover their cost. For coverage to become possible, Healpods would need to undergo rigorous clinical trials demonstrating safety and efficacy, obtain proper regulatory classification, and align with medical necessity standards used by payers.
Conclusion
Healpods show potential as a supportive tool in addiction treatment by creating calming spaces that may help with stress and cravings. But without strong scientific evidence, FDA approval, or insurance coverage, their use remains very limited. Until more research is done, Healpods should be seen as an extra option rather than a primary form of treatment, and fairness, cost, and access need to be carefully considered.
Video: How HealPods Rewire Addiction Recovery #Innovation #MentalWellness #AddictionRecovery