Gastrointestinal (GI) disorders connected to drug use are far more common than most people realize. Medications and substances, from prescription pills to recreational drugs, can directly impact the digestive system. Some cause mild issues, such as an upset stomach, while others trigger long-lasting or even permanent problems. After years of reading up and talking with people navigating these challenges, I’m convinced that understanding the link between drugs and GI health helps people spot trouble early and make wise choices. Here, I’ll break down the types of GI disorders drugs can cause, the most common culprit drugs, what symptoms to watch for, and some practical ways to take care of your gut if you’re managing regular medication or substance use.
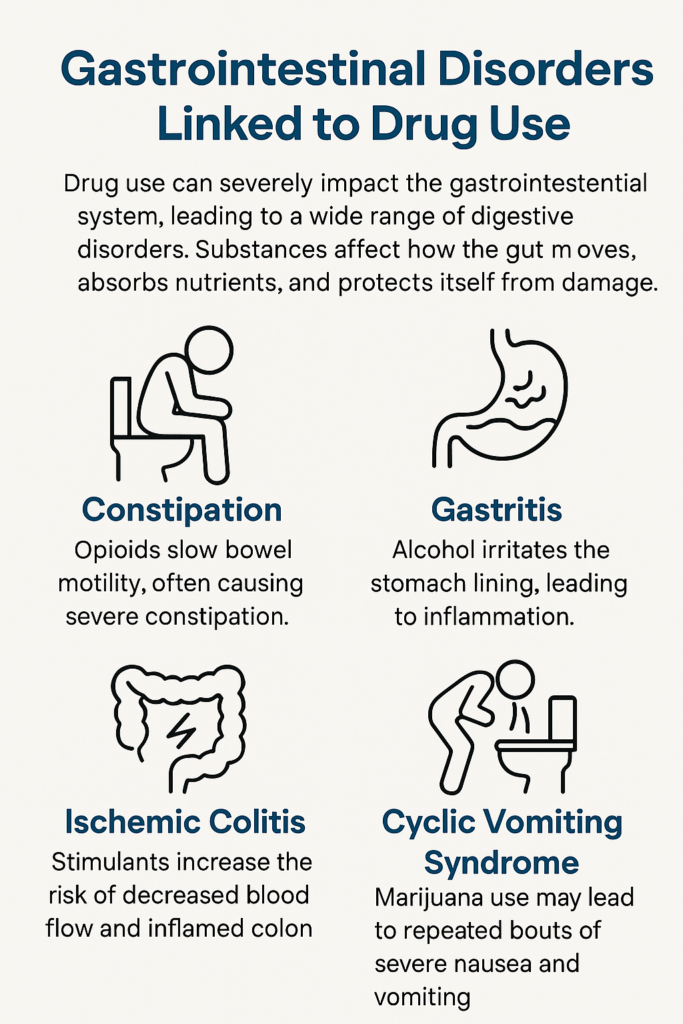
Main Types of Gastrointestinal Disorders from Drug Use
Not every upset stomach is caused by medication, but quite a few drugs can mess with how your digestive system works. Here are the main trouble spots I come across most often:
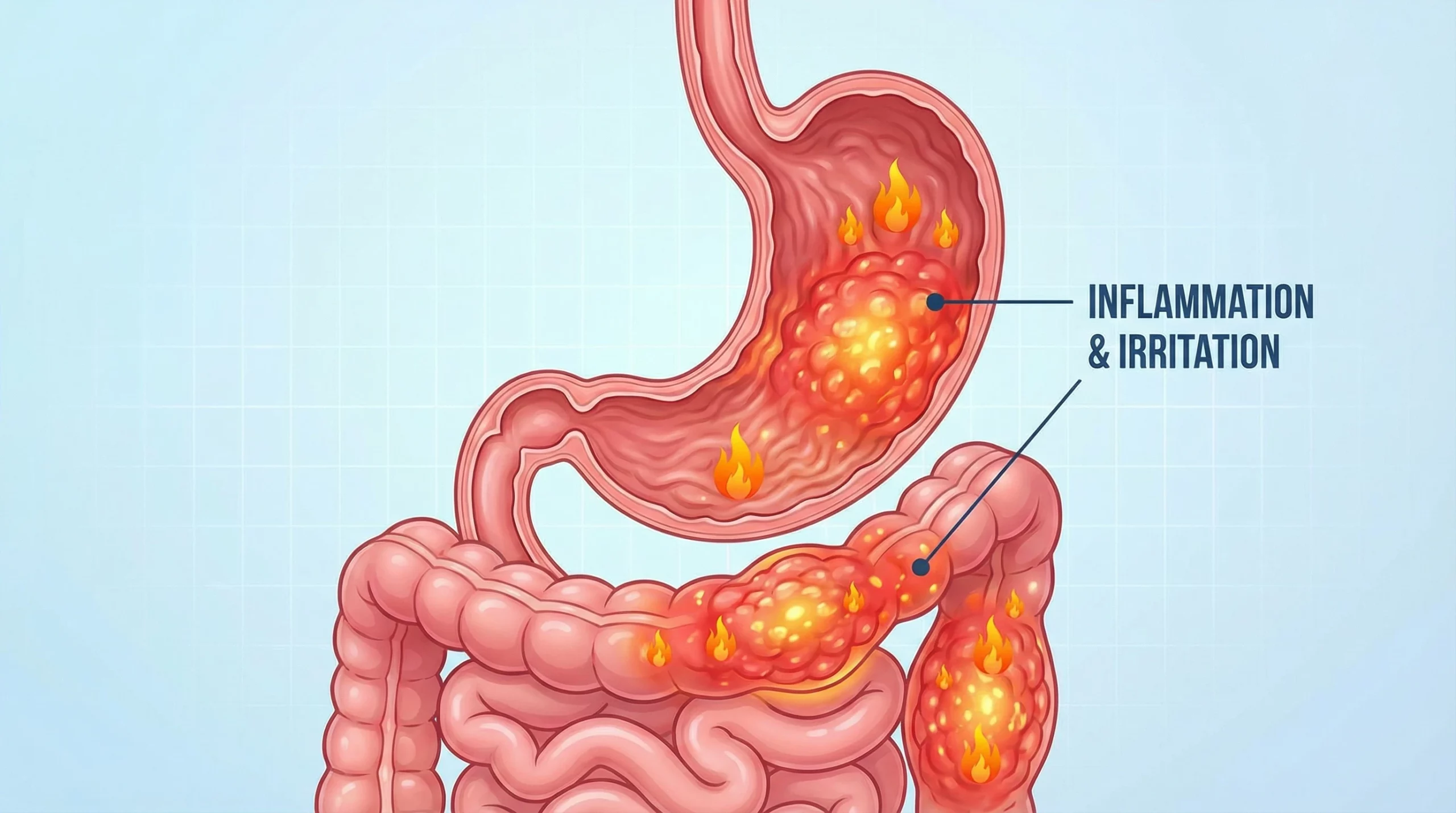
- Gastritis and Ulcers: Some meds, especially painkillers and anti-inflammatories, can wear at the stomach lining and cause irritation or sores.
- Constipation: Certain drugs slow down the bowels, leaving you backed up and uncomfortable.
- Diarrhea: A handful of antibiotics and other drugs irritate the gut, leading to frequent, loose stools.
- Liver and Pancreas Problems: Some substances can put heavy stress on these organs, causing pain, nausea, or more serious illness.
- GI Bleeding: Both prescription drugs and recreational substances can boost the risk of bleeding anywhere from the esophagus to the large intestine.
Recognizing the type of GI issue is the first step in determining whether a drug might be at fault.
Common Drugs Linked to GI Disorders
People are sometimes surprised when a medication that helps one problem ends up causing side effects somewhere else. Here’s a quick rundown of the drugs most often linked to gut issues:
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): Ibuprofen, aspirin, and naproxen are known to irritate the stomach and may cause ulcers or bleeding.
- Opioid Pain Medications: Drugs like oxycodone, codeine, and morphine often slow digestion and can cause persistent constipation.
- Antibiotics: These can knock out both good and bad gut bacteria, sometimes leading to diarrhea or stomach cramps.
- Stimulants: Caffeine and certain ADHD medications can ramp up stomach acid, occasionally causing gastritis or reflux.
- Alcohol: Heavy drinking inflames the stomach lining, potentially leading to ulcers, pancreatitis, and liver trouble.
- Cocaine and Methamphetamine: Beyond causing nausea and abdominal pain, these can also restrict blood flow to the intestines, sometimes leading to even more serious complications.
This isn’t a complete list, but it covers the prescriptions and substances I hear most about when folks are wrestling with GI problems.
How Drug Use Affects the Digestive Tract
The digestive system is more sensitive to drugs than many folks realize. The effects can vary, depending on what you’re taking and for how long, but the gut almost always notices when something new is in the mix. Here’s what happens with the most common offenders:
- Stomach Irritation: NSAIDs and alcohol strip away the protective mucus from the stomach lining, upping the risk of heartburn, nausea, or sores.
- Gut Motility Changes: Opioids slow everything down, causing constipation. Some antibiotics or laxatives do the opposite, speeding things up and causing diarrhea.
- Liver Strain: Medications and alcohol need to be filtered by the liver. Overuse or certain combinations can overload it, leading to swelling, pain, or jaundice (deep yellowing of the skin).
- Pancreatitis: Alcohol, certain diuretics, and high-dose steroids can inflame the pancreas, bringing intense pain and a host of digestive upsets.
Gut symptoms that don’t let up or keep getting worse after starting a new medication should be checked out by a healthcare provider. Sometimes just switching drugs or tweaking the dose can make a world of difference.
Recognizing the Symptoms: What to Watch For
It’s easy to write off GI symptoms as leftovers from questionable takeout or a stressful week. However, persistent symptoms can be linked to medications or substances. Here are the red flags that you shouldn’t ignore:
- Bloating, nausea, or frequent vomiting
- Sudden or unexplained abdominal pain
- Black, tarry stools or blood in the stool (signs of internal bleeding)
- Ongoing constipation or severe diarrhea
- Loss of appetite or sudden weight loss
- Yellowing of the skin or eyes
It’s smart to keep a list of current medications and report these symptoms to your doctor, especially if you’ve recently started something new.
Managing and Preventing GI Problems While Using Drugs
Looking after digestive health doesn’t always mean ditching your medication. Often, a few minor changes can reduce side effects:
- Take medicines with food or after meals, unless told otherwise.
- Drink plenty of water to keep things moving, especially with opioids or other constipating medications.
- Add fiber-rich foods to your diet to improve regularity and digestion.
- If you’re on antibiotics, adding probiotics can help reset gut bacteria balance (chat with your healthcare provider about the best options).
- Avoid mixing drugs with alcohol to prevent extra stress on your GI system and liver.
- Stick closely to dosing instructions and avoid experimenting with dosages without your provider’s input.
For folks using prescriptions long-term, regularly checking in with your provider can spot GI issues before they turn into something bigger. A little bit of prevention makes a big difference for gut health.
When to Seek Help
Not every stomachache is a significant concern, but there are times when you should get medical help right away. If these symptoms pop up, call your doctor or visit urgent care:
- Severe abdominal pain that won’t go away
- Vomiting blood or something that looks like coffee grounds
- Blood in your stools or very dark stools
- Signs of dehydration (parched mouth, hardly any urine, weakness)
- Yellow skin, confusion, or swelling in your belly
Trying to tough it out can make things worse. Medical professionals deal with these issues all the time, and the sooner you seek advice, the easier the recovery may be.
Extra Tips for Protecting Your Gut
Over the years, I’ve picked up a few tricks to keep my digestive system happy when starting new meds. Here are some strategies that have helped me and others:
- Stick to a steady, balanced diet to avoid extra stomach upset.
- Watch out for over-the-counter medications that might clash with prescriptions.
- Ask about alternative medications if side effects become unmanageable.
- Keep a journal of any side effects on paper or your phone; it can be helpful at doctor’s visits.
- Never mix recreational drugs and prescription meds without running it past your provider—the interaction might make GI symptoms much worse.
These steps make it easier to maintain gut health while still getting the benefits of necessary medications.
Frequently Asked Questions
GI side effects come up a lot whenever medication is discussed. Here are questions I’m often asked:
Why do some medicines upset my stomach?
Medications can irritate your digestive lining, disrupt gut bacteria, or change the speed at which food moves through your digestive tract. The way your body handles drugs varies, but some medications are especially notorious for causing stomach issues.
How can I avoid constipation when taking painkillers?
Upping your water and fiber intake, plus getting a little more active, can help. Some folks find stool softeners useful as well, but make sure to ask your healthcare provider first.
Is it safe to use probiotics if I’m on antibiotics?
Many people use probiotics to help restore gut bacteria to a balanced state after taking antibiotics. Not everyone needs them, but some find them helpful for antibiotic-induced diarrhea. Your provider can help you pick a probiotic that works for you.
Can over-the-counter drugs be just as hard on my gut as prescriptions?
Some OTC medications, including NSAIDs and famotidine, can cause GI trouble, especially with high doses or long-term use. Your risk depends on your health history, so always read the directions and check with a pharmacist or doctor if you have concerns.
Key Takeaways for Drug-Linked GI Health
Staying on top of how drugs can mess with your digestive system is crucial if you regularly use prescriptions or recreational substances. Knowing what symptoms could mean trouble—and acting fast—can help you avoid a lot of discomfort. Honest conversations with your doctor about what you’re taking and any gut woes you have usually lead to better, more comfortable solutions. GI issues don’t have to get in the way of effective treatment. Working together with your healthcare team can keep you on the right track for gut and overall health.
Video: Gastrointestinal Disorders Linked to Drug Use