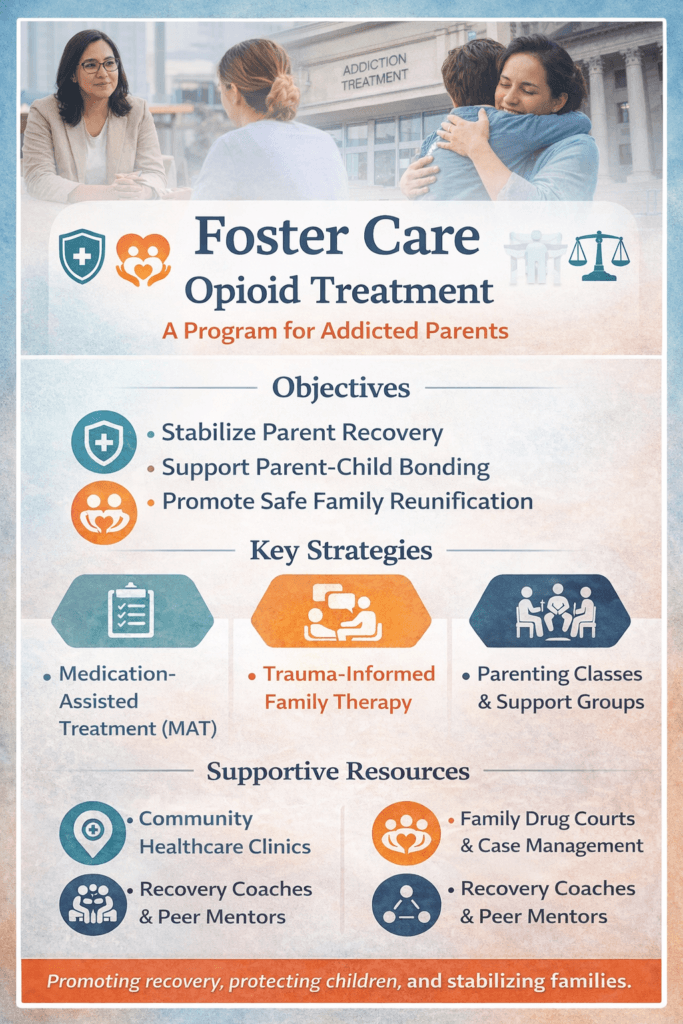
Foster care involvement related to opioid use disorder (OUD) represents one of the most complex intersections of public health and child welfare. When parental substance use leads to child removal, the focus must extend beyond crisis response toward coordinated recovery and family stabilization. Foster Care Opioid Treatment requires more than medication or court compliance—it demands structured self-management from parents, informed and supportive family engagement, and accessible community resources. Together, these layers create a framework that prioritizes child safety while recognizing addiction as a treatable, chronic medical condition. Effective intervention addresses trauma, stability, accountability, and long-term recovery rather than short-term compliance alone.
Foster Care and Opioid Treatment: Supporting Vulnerable Youth Affected by the Opioid Crisis
The opioid crisis has profoundly impacted the foster care system across the United States. As opioid use disorder (OUD) affects parents and caregivers, increasing numbers of children enter foster care due to neglect, parental incapacity, or overdose-related deaths. This intersection between foster care and opioid treatment presents both urgent challenges and opportunities for coordinated, trauma-informed care.
Many children entering foster care have experienced significant instability, including exposure to substance use, inconsistent caregiving, domestic conflict, or economic hardship. Some infants are born with neonatal abstinence syndrome (NAS), requiring specialized medical monitoring and follow-up care. For these children, early intervention is critical to support physical health, emotional regulation, and developmental milestones.
Effective opioid treatment within the foster care context must be comprehensive. For parents, evidence-based treatment such as medication-assisted treatment (MAT)—including buprenorphine or methadone—combined with counseling and social services can improve stability and increase the likelihood of family reunification. When treatment is accessible, consistent, and supported by child welfare systems, outcomes improve for both parents and children.
For children and adolescents in foster care, trauma-informed mental health services are essential. Many youth in care experience anxiety, depression, behavioral challenges, or attachment disruptions linked to parental substance use. Access to therapy, stable placements, educational support, and consistent caregiving environments helps mitigate the long-term risk of substance use in the next generation.
Collaboration between healthcare providers, child welfare agencies, courts, and community organizations is key. When systems communicate effectively, treatment plans can align with permanency goals, ensuring that parental recovery efforts are considered within custody decisions. Family drug courts and integrated case management programs have shown promise in supporting recovery while prioritizing child safety.
Ethically, the foster care–opioid treatment intersection requires balancing child protection with compassionate support for parents in recovery. Addiction is a chronic medical condition, and stigma can undermine family-centered solutions. Policies that emphasize evidence-based treatment rather than punitive removal alone can reduce long-term harm.
Addressing opioid use within the foster care system demands prevention, early treatment access, and long-term recovery support. When communities invest in coordinated care, they not only protect vulnerable children but also strengthen families and interrupt cycles of intergenerational addiction.
Self-Management Strategies in Foster Care Opioid Treatment: Strengthening Recovery and Family Stability
When opioid use disorder (OUD) intersects with the foster care system, self-management becomes a critical component of recovery and family reunification. Parents involved in child welfare cases often face intense emotional stress, court oversight, and structured treatment requirements. Developing strong self-management strategies can improve treatment outcomes, demonstrate stability, and increase the likelihood of safe family restoration.
One of the most important strategies is consistent engagement in medication-assisted treatment (MAT), such as buprenorphine or methadone, when prescribed. Taking medication as directed, attending appointments reliably, and communicating openly with providers builds both physiological stability and documented progress—an important factor in child welfare evaluations.
Structured daily routines also support recovery. Establishing consistent sleep schedules, work or vocational training, therapy attendance, and parenting classes helps regulate stress and reinforce responsibility. Predictability strengthens emotional regulation, which is essential when navigating court hearings, supervised visits, and caseworker expectations.
Emotional self-regulation is equally vital. Foster care involvement can trigger guilt, shame, fear, or anger. Practicing stress-management techniques—such as mindfulness, journaling, breathing exercises, or physical activity—reduces the risk of relapse during high-pressure moments. Recognizing emotional triggers early and seeking support proactively can prevent setbacks.
Another key strategy is transparent communication. Keeping documentation of treatment attendance, negative drug screens, therapy participation, and progress goals helps demonstrate accountability. Open communication with caseworkers, legal representatives, and treatment providers builds trust and reduces misunderstandings.
Building a recovery-support network is also essential. Peer support groups, recovery coaching, faith communities, and family allies provide encouragement and accountability. Isolation increases vulnerability to relapse, while connection reinforces motivation and hope.
Parenting skill development is another important focus of self-management. Participating in evidence-based parenting programs and practicing these skills during supervised visits demonstrates a commitment to growth. Learning positive discipline, attachment-building techniques, and healthy communication strengthens both recovery and reunification potential.
Finally, self-compassion matters. Recovery within the foster care system can feel overwhelming, but sustained progress—not perfection—is the goal. Recognizing addiction as a treatable medical condition helps parents remain engaged in care rather than discouraged by setbacks.
Effective self-management in foster care opioid treatment is about stability, accountability, and resilience. With consistent effort, structured support, and proactive coping strategies, parents can strengthen recovery while working toward safe, sustainable family reunification.
Family Support Strategies in Foster Care Opioid Treatment: Strengthening Recovery and Reunification
When opioid use disorder (OUD) leads to foster care involvement, recovery is not just an individual process—it becomes a family-centered journey. Family support strategies play a crucial role in improving treatment engagement, emotional stability, and the likelihood of safe reunification. A coordinated, compassionate family response can significantly influence long-term outcomes for both parents and children.
One of the most powerful strategies is education. Families who understand opioid use disorder as a chronic medical condition—rather than a moral failing—are better equipped to provide constructive support. Learning about medication-assisted treatment (MAT), relapse prevention, and trauma-informed care reduces stigma and fosters realistic expectations about recovery timelines.
Stable communication is equally important. Encouraging open, nonjudgmental dialogue allows parents in treatment to express fears, setbacks, and progress honestly. Consistent communication between extended family members, foster caregivers, and treatment providers (when appropriate and legally permitted) helps align goals around child safety and parental recovery.
Kinship care arrangements—where children stay with relatives—can offer additional stability. Familiar family environments often reduce trauma for children while maintaining a connection to biological parents. However, boundaries must remain clear. Support should not cross into enabling behaviors. Structured expectations around sobriety, visitation, and accountability protect both recovery and child well-being.
Participation in family therapy can further strengthen outcomes. Therapy sessions provide a safe space to address trust, attachment disruptions, and communication breakdowns that often accompany addiction. Trauma-informed approaches help both parents and children process emotional distress related to separation and substance use.
Families can also reinforce recovery through practical support. Helping with transportation to treatment appointments, attending court hearings to encourage attendance, assisting with childcare during therapy sessions, and supporting parenting classes all contribute to consistent engagement in care. These tangible actions demonstrate commitment while reinforcing responsibility.
Equally important is self-care for family members. Supporting someone involved in foster care and opioid treatment can be emotionally taxing. Family support groups, counseling, and education programs help relatives manage stress, set healthy boundaries, and avoid burnout.
Ultimately, family support strategies in foster care opioid treatment centers on stability, education, accountability, and compassion. When families collaborate with treatment providers and child welfare systems, they help create an environment in which recovery and reunification become realistic, sustainable goals.
Community Resource Strategies in Foster Care Opioid Treatment: Coordinating Recovery and Child Welfare Support
The intersection of opioid use disorder (OUD) and foster care requires coordinated community-level responses. When parents enter treatment while involved in the child welfare system, recovery outcomes are heavily influenced by the strength and accessibility of local resources. Community strategies can bridge gaps between healthcare, legal systems, and social services to promote both child safety and parental recovery.
One of the most effective community strategies is the integration of treatment and child welfare systems. Family drug courts, for example, combine judicial oversight with structured treatment plans, frequent monitoring, and supportive services. These programs emphasize accountability while prioritizing rehabilitation rather than punishment alone. When courts collaborate with treatment providers, timelines and expectations become clearer and more recovery-focused.
Accessible medication-assisted treatment (MAT) is another essential component. Communities must ensure that parents involved in foster care cases can obtain timely access to buprenorphine or methadone, along with counseling and behavioral health services. Delays in treatment can prolong foster placements and increase relapse risk. Integrated care models that combine addiction treatment, mental health support, and primary care reduce fragmentation.
Trauma-informed services for children are equally important. Community mental health programs, early childhood intervention services, school-based counseling, and developmental screenings help address the emotional and psychological impact of parental substance use. Stabilizing children’s mental health strengthens long-term family resilience.
Housing and employment programs also play a major role. Stable housing reduces environmental stressors that contribute to relapse and demonstrates readiness for reunification. Recovery-friendly workplaces, vocational training, and job placement services support financial stability—often a requirement in child welfare case plans.
Peer recovery support services provide an additional layer of strength. Recovery coaches, parent mentors who have successfully navigated foster care involvement, and community recovery centers provide guidance, accountability, and hope. Shared lived experience helps reduce stigma and isolation.
Finally, cross-sector collaboration is key. Healthcare providers, child welfare agencies, legal systems, schools, and community organizations must communicate consistently. Coordinated case management ensures that treatment progress aligns with permanency planning for children.
Community resource strategies in foster care opioid treatment are about integration, accessibility, and sustainability. When systems work together, they not only protect vulnerable children but also provide parents with a structured pathway to recovery and safe reunification.
Frequently Asked Questions
Here are some common questions:
1. What is a Foster Care Opioid Treatment program?
It is a coordinated program designed for parents with opioid use disorder (OUD) whose children are involved in the foster care system. It combines medication-assisted treatment (MAT), counseling, parenting support, case management, and court coordination to promote recovery and safe reunification.
2. What is Medication-Assisted Treatment (MAT)?
MAT uses FDA-approved medications such as buprenorphine or methadone, combined with counseling and behavioral therapies, to reduce cravings, prevent withdrawal, and stabilize recovery.
3. Can I regain custody of my child while in treatment?
Possibly. Courts and child welfare agencies evaluate progress individually. Consistent treatment engagement, negative drug screens, stable housing, and compliance with case plans improve the likelihood of reunification.
4. Will I be allowed visitation during treatment?
In many cases, yes. Supervised visitation is often permitted when parents demonstrate compliance with treatment and court requirements.
5. How long does the program last?
Program length varies depending on recovery progress, court timelines, and child welfare requirements. It may range from several months to over a year.
6. Can my family be involved in my recovery process?
Yes. Family therapy, kinship care options, parenting classes, and support programs may be available to strengthen family stability and support reunification efforts.
7. What role do family drug courts play?
Family drug courts provide structured oversight, accountability, and coordinated case management while prioritizing treatment over punishment.
8. What services are typically included?
Services may include MAT, individual counseling, trauma-informed therapy, parenting education, peer recovery support, housing assistance, job training, and case management.
9. Are there financial resources available?
Many parents qualify for Medicaid or state-funded treatment programs. Housing assistance, transportation services, and recovery grants may also be available depending on location.
10. What happens if I relapse?
Relapse does not automatically constitute program failure; however, it is taken seriously. Courts and treatment teams often reassess the care plan and increase support or supervision rather than immediately ending services.
11. How does this program benefit my child?
The goal is child safety and emotional stability while supporting parental recovery. Coordinated treatment improves the chances of safe, stable reunification and reduces long-term trauma.
12. Is recovery possible while involved in foster care?
Yes. With consistent engagement, structured support, and accountability, many parents successfully achieve recovery and reunify with their children.
Conclusion
Successful outcomes in Foster Care Opioid Treatment depend on collaboration across individual, family, and community levels. Parents who practice consistent self-management—engaging in treatment, regulating stress, and demonstrating accountability—build the foundation for reunification. Families who provide education, boundaries, encouragement, and structured support reinforce recovery stability. Communities that integrate healthcare, legal systems, housing, mental health services, and peer support create sustainable pathways for healing. When these strategies align, they not only protect children but also interrupt cycles of intergenerational addiction, offering families a realistic opportunity for restoration, resilience, and long-term stability.
Video: Foster Care Opioid Treatment Supporting Recovery and Safe Reunification