Emotion-oriented coping styles like avoidance, self-blame, and suppression can increase the risk of addiction by encouraging emotional escape. Preventing addiction involves teaching self-management strategies such as mindfulness and healthy expression, while also strengthening family support through open communication and emotional validation. Community resources—like mental health services and peer networks—further support emotional resilience. Together, these strategies help individuals develop healthier ways to cope and reduce reliance on addictive behaviors.
How Emotion-Oriented Coping Styles Can Increase Addiction Risk
Emotion-oriented coping styles that focus on managing distress without addressing the root problem can increase the risk of addiction. These coping strategies often attempt to reduce negative emotions like anxiety, sadness, or anger, but in maladaptive ways. When such strategies become habitual, they can drive people toward substance use or behavioral addictions as a form of emotional escape or regulation.
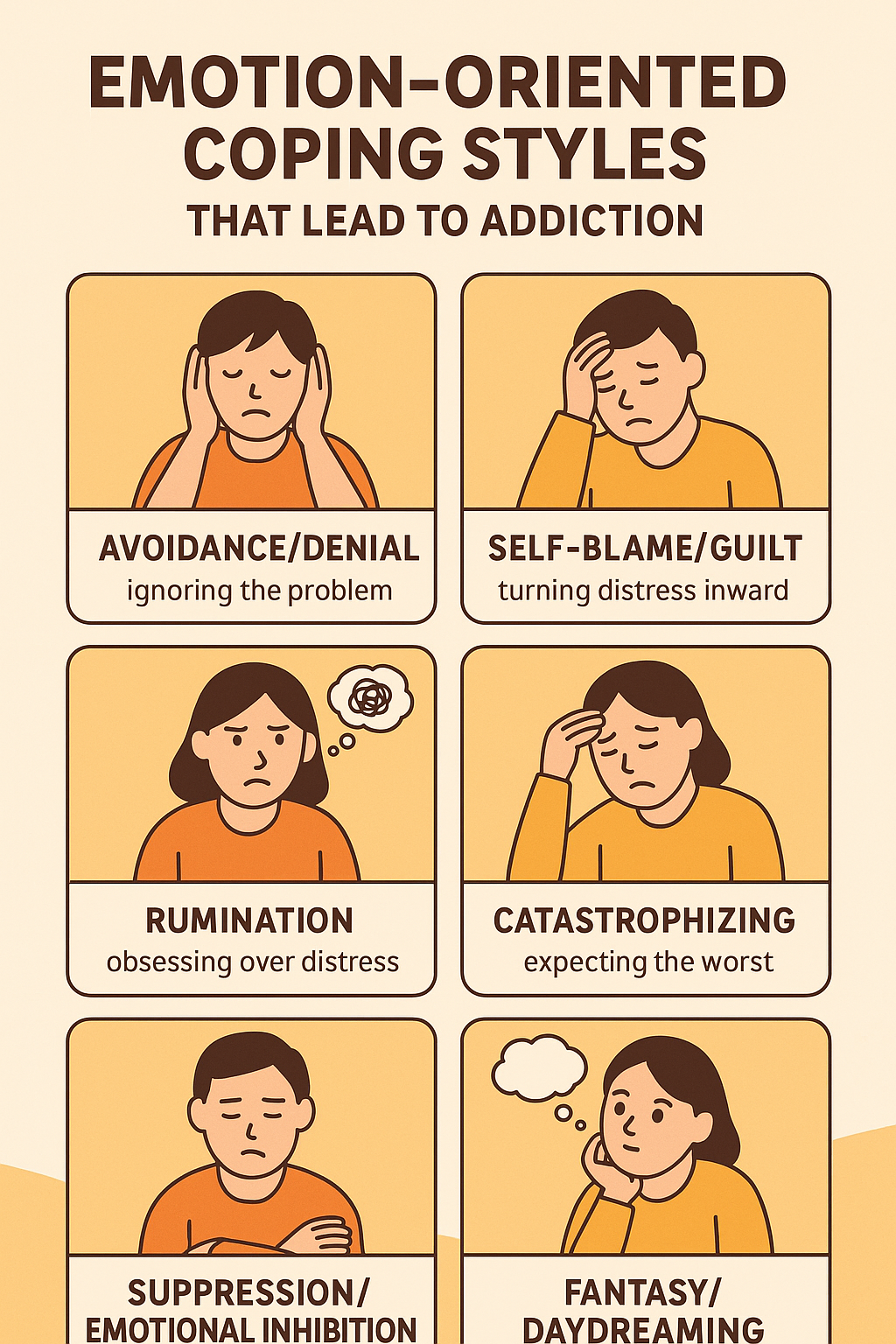
Here are key emotion-oriented coping styles linked to addiction:
1. Avoidance/Denial
- Definition: Ignoring the problem or pretending it doesn’t exist.
- How it leads to addiction: Individuals may use substances to numb feelings or avoid confronting painful issues (e.g., trauma, relationship conflict).
Example: A person drinks alcohol nightly to avoid dealing with grief or loneliness.
2. Self-Blame/Guilt
- Definition: Turning distress inward, believing one is at fault for everything.
- How it leads to addiction: Chronic self-criticism can increase depression and drive compulsive behaviors like drinking, drug use, or binge eating to suppress these feelings.
Example: Someone with low self-worth might use stimulants to feel “good enough.”
3. Rumination
- Definition: Obsessively thinking about distressing situations or emotions.
- How it leads to addiction: Constant emotional recycling of past hurts or perceived failures can lead individuals to seek temporary mental relief through addictive behaviors.
Example: A person replays a breakup repeatedly and smokes weed to “shut their brain off.”
4. Catastrophizing
- Definition: Exaggerating the negative aspects of a situation, expecting the worst.
- How it leads to addiction: The overwhelming emotional responses may lead people to seek instant relief or escape through drugs, gambling, or other compulsive behaviors.
5. Suppression/Emotional Inhibition
- Definition: Bottling up emotions or trying not to feel.
- How it leads to addiction: Repressed emotions often seek an outlet, and substances can become a way to release or dull what’s not being processed consciously.
6. Emotional Venting Without Problem-Solving
- Definition: Expressing emotions excessively without trying to fix the problem.
- How it leads to addiction: While venting may feel good in the short term, if it’s not paired with action, the stress remains and may push a person toward addictive relief.
7. Fantasy/Daydreaming
- Definition: Escaping reality by imagining a different life or identity.
- How it leads to addiction: This style can pair with drug use or gaming, where the person feels more powerful, in control, or accepted in fantasy than in real life.
7 Self-Management Strategies to Improve Emotional Coping and Prevent Addiction
Unhealthy emotional coping styles—like avoidance, rumination, or denial—can drive people toward addiction as a form of escape. However, developing self-management strategies that build emotional awareness, resilience, and healthy regulation can turn those same emotional struggles into powerful opportunities for growth and prevention.
Here are effective self-management strategies to improve emotional coping styles and help prevent addiction. These focus on building emotional awareness, resilience, and healthy regulation, turning maladaptive emotional coping into constructive responses:
🧠 1. Build Emotional Awareness
- Why: You can’t manage what you don’t recognize.
- Strategies:
- Keep an emotion journal—track situations, triggers, and feelings.
- Practice naming emotions (“I feel overwhelmed” instead of “I’m bad”).
- Use apps like Moodfit, Daylio, or CBT Thought Diary.
🧘♀️ 2. Practice Mindfulness & Acceptance
- Why: Helps tolerate distress without acting on impulse.
- Strategies:
- Daily mindfulness meditation (10–15 minutes).
- Use grounding techniques (5-4-3-2-1 sensory awareness).
- Accept feelings without judgment (learn from them, don’t run from them).
🗣 3. Use Healthy Emotional Expression
- Why: Suppressed or poorly managed emotions drive unhealthy escape.
- Strategies:
- Practice assertive communication (use “I” statements).
- Talk regularly with a trusted person or support group.
- Use creative outlets—art, music, writing.
🧩 4. Cognitive Restructuring
- Why: Reduces catastrophizing, rumination, and self-blame.
- Strategies:
- Identify and challenge irrational thoughts (“Is this really true?”).
- Replace them with balanced thoughts (“This is hard, but I can cope”).
- Try CBT self-help tools or therapy worksheets.
🏃♂️ 5. Engage in Behavioral Activation
- Why: Positive action can regulate mood better than avoidance.
- Strategies:
- Create a daily routine with small, enjoyable tasks.
- Include physical activity, social time, and hobbies.
- Use a habit tracker or rewards system to stay consistent.
🧩 6. Stress-Reduction Techniques
- Why: Lowers the emotional intensity that can drive substance use.
- Strategies:
- Use deep breathing, progressive muscle relaxation, or yoga.
- Practice time management to reduce overwhelm.
- Schedule regular self-care (even 15 minutes a day helps).
💬 7. Develop a Relapse Prevention Plan
- Why: Prepares you for emotional triggers before they escalate.
- Strategies:
- List high-risk emotional situations (e.g., loneliness, shame).
- Identify healthy alternatives (call someone, take a walk, journal).
- Use a “STOP” strategy: Stop, Take a breath, Observe, Proceed.
📌 Summary Table
| Maladaptive Coping | Healthy Replacement |
|---|---|
| Avoidance/Denial | Journaling, Reality checking |
| Self-Blame | Self-compassion, CBT reframes |
| Rumination | Distraction + Mindfulness |
| Catastrophizing | Thought-challenging |
| Suppression | Assertive communication |
| Fantasy/Daydreaming | Goal-setting + Hobbies |
8 Family Support Strategies to Strengthen Emotional Coping and Prevent Addiction
Families play a powerful role in shaping how individuals manage emotions—positively or negatively. When emotional expression is supported and healthy coping is modeled at home, the risk for addiction significantly decreases. These family support strategies help improve emotional coping styles, reduce maladaptive behaviors, and foster resilience.
🧠 1. Model Healthy Emotional Regulation
- Why: Children and adults alike learn emotional habits from their close family.
- How:
- Show calm during stress rather than panic or suppression.
- Verbally label your own emotions and coping actions (“I feel frustrated, so I’m going for a walk to cool off.”).
💬 2. Encourage Open Communication
- Why: Reduces emotional suppression and denial.
- How:
- Practice active listening without judgment.
- Set a family norm of expressing feelings (weekly check-ins or emotion cards).
- Avoid shaming or minimizing emotions (“Don’t cry” → “It’s okay to be upset.”).
👨👩👧👦 3. Foster a Safe, Supportive Environment
- Why: Emotional safety reduces the need to escape or fantasize.
- How:
- Maintain consistent routines, boundaries, and expectations.
- Show unconditional positive regard: “You’re loved, even when you’re struggling.”
- Make home a “no-shame zone.”
🧰 4. Teach and Practice Coping Skills Together
- Why: Builds family-wide emotional resilience.
- How:
- Learn and use mindfulness, journaling, or breathing exercises as a group.
- Role-play situations and rehearse calm responses.
- Reward healthy coping with family praise or shared activities.
🧭 5. Set Realistic Expectations and Goals
- Why: Prevents catastrophizing and perfectionism.
- How:
- Emphasize progress over perfection.
- Normalize failure as a learning opportunity.
- Help break large tasks into manageable steps.
💖 6. Validate Each Other’s Emotions
- Why: Counters self-blame and rumination.
- How:
- Respond to emotions with empathy: “That sounds really hard.”
- Avoid “fixing” right away; instead, say “I’m here with you.”
- Teach that all emotions are okay—it’s actions that matter.
🧑⚕️ 7. Seek Family Counseling When Needed
- Why: A trained therapist can guide healthier emotional patterns.
- How:
- Consider CBT-based or family systems therapy.
- Address unresolved trauma, conflict, or communication breakdowns.
- Learn strategies to prevent co-dependency or enabling.
🔁 8. Break Intergenerational Emotional Patterns
- Why: Many families repeat emotional avoidance, shame, or blaming.
- How:
- Reflect on your own childhood coping messages.
- Create a family mantra (e.g., “We talk, we feel, we grow.”)
- Acknowledge past patterns without blame and commit to change.
✅ Summary Table
| Coping Risk Factor | Family Strategy to Prevent It |
|---|---|
| Avoidance/Denial | Normalize open discussion of emotions |
| Suppression | Validate feelings regularly |
| Self-blame | Provide unconditional support, not criticism |
| Catastrophizing | Promote flexible thinking and optimism |
| Rumination | Model problem-solving, not emotional dwelling |
| Fantasy/Escape | Build safe, engaging real-life relationships |
7 Community Strategies to Improve Emotional Coping and Prevent Addiction
Emotional resilience isn’t built in isolation—it flourishes when communities invest in resources that support emotional growth, connection, and healing. The following community-based strategies help individuals and families access environments and tools that strengthen emotional coping and reduce the risk of substance use and addiction:
🧑🏫 1. Offer Community-Based Psychoeducation
- Why: Educates people on emotional coping and addiction risks.
- How:
- Host workshops on stress management, trauma, and emotional regulation.
- Integrate coping-skills training in schools, churches, and libraries.
- Distribute flyers or infographics in public spaces.
🤝 2. Strengthen Peer Support Networks
- Why: Encourages shared emotional experiences without stigma.
- How:
- Promote peer-led support groups (e.g., SMART Recovery, Al-Anon, grief circles).
- Train peer mentors in emotional coaching and referral services.
- Create safe spaces for people to share feelings and solutions.
🧠 3. Expand Access to Mental Health Services
- Why: Provides professional help for emotional dysregulation.
- How:
- Offer affordable, sliding-scale therapy or counseling services.
- Set up mobile mental health clinics or telehealth services in underserved areas.
- Include emotional coping assessments in primary care settings.
🏫 4. Embed Coping Skills in Schools and Youth Programs
- Why: Teaches children and teens early emotional resilience.
- How:
- Introduce SEL (Social Emotional Learning) in classrooms.
- Train teachers and after-school staff in trauma-informed practices.
- Encourage expressive activities such as art, journaling, and guided group discussions.
🏘 5. Create Emotionally Supportive Community Spaces
- Why: Safe environments reduce emotional triggers and isolation.
- How:
- Support community centers that offer calming environments and skill-building classes.
- Develop recovery-friendly housing and substance-free recreation zones.
- Encourage “emotion-friendly” policies in shelters, jails, and clinics.
🧭 6. Promote Culturally-Affirming Healing Resources
- Why: Cultural identity and validation are vital for emotional safety.
- How:
- Partner with faith leaders, tribal elders, or cultural groups to blend tradition with evidence-based care.
- Offer storytelling, rituals, or community ceremonies that affirm identity and regulate emotion.
📱 7. Utilize Technology and Hotlines for Emotional Support
- Why: Fills gaps in moments of crisis or isolation.
- How:
- Promote 24/7 emotional support lines (e.g., 988, SAMHSA Helpline).
- Offer mobile apps with mindfulness, CBT tools, or journaling prompts.
- Build online communities for emotional check-ins and connection.
✅ Summary Table
| Emotional Challenge | Community Strategy |
|---|---|
| Avoidance/Denial | Peer support and education groups |
| Rumination | Counseling access and journaling apps |
| Suppression | Safe expressive community outlets |
| Self-blame | Group validation and affirming mentors |
| Catastrophizing | Skill-based psychoeducation |
| Emotional isolation | Connection to peer and cultural networks |
Frequently Asked Questions
Here are some common questions:
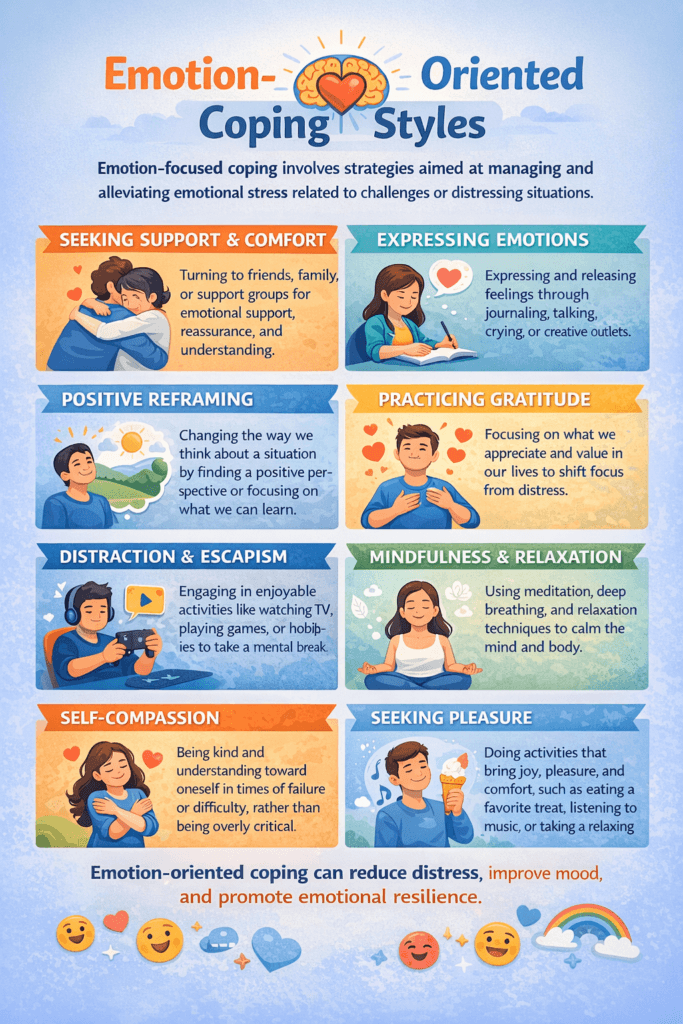
Question: Provide an infographic flyer on emotion-coping styles.
Answer:
Question: How can you help someone manage their emotional coping skills and prevent addiction?
Answer: Helping someone manage their emotional coping skills and prevent addiction involves a mix of empathy, practical support, and guiding them toward healthier ways of handling emotions. Here’s a straightforward, actionable approach you can take—whether you’re a loved one, peer, or professional:
🔍 1. Recognize Warning Signs
Be aware of emotional behaviors that may lead to unhealthy coping:
- Avoidance or emotional shutdown
- Mood swings or irritability
- Self-medicating with substances
- Isolating from others
- Negative self-talk or hopelessness
🫱🏽🫲🏽 2. Build a Supportive Relationship
- Be present and nonjudgmental.
- Validate their emotions: “It’s okay to feel overwhelmed.”
- Encourage open dialogue about stress, fear, or sadness.
Tip: Avoid trying to “fix” their emotions. Focus on listening and being trustworthy.
🧘🏽 3. Encourage Healthy Coping Skills
Introduce or model emotional regulation tools:
- Deep breathing, grounding exercises, or mindfulness
- Journaling thoughts and triggers
- Talking to a peer or support person
- Physical activity or creative expression (art, music, etc.)
Example: Say, “When I’m anxious, I take 5 slow breaths or go for a walk—want to try it with me?”
🎯 4. Set Small, Achievable Goals
Help them identify what they can control:
- Get 7–8 hours of sleep
- Eat one nutritious meal a day
- Limit screen time or news consumption
- Replace negative habits with one positive action
🧑⚕️ 5. Connect to Resources
- Offer help finding a therapist, counselor, or support group
- Share hotlines like 988 or the SAMHSA Helpline (1-800-662-HELP)
- Suggest mobile apps for mindfulness or journaling (e.g., Calm, Headspace, Moodpath)
If you’re unsure how to help, just offering to make the first call or attend a support group with them can be powerful.
🌱 6. Reinforce Progress, Not Perfection
- Celebrate small wins (like expressing a feeling instead of avoiding it).
- Be patient with relapses or setbacks.
- Remind them: learning to cope is a process, not a switch.
🏘️ 7. Create a Healthy Environment
- Limit exposure to substances or toxic influences
- Encourage positive peer connections
- Suggest involvement in faith groups, volunteering, or local clubs
📌 Summary
To help someone manage emotional coping and prevent addiction:
Celebrate progress and encourage consistency
Be a safe, nonjudgmental listener
Model and teach practical emotion regulation strategies
Connect them to mental health and community resources
Question: What are the warning signs that a person’s coping style can be dangerous to themselves?
Answer: Certain coping styles—mainly when used consistently—can become emotionally or physically dangerous to the person using them. Here are key warning signs that someone’s coping mechanisms may be harmful and potentially linked to addiction or mental health risks:
🚨 1. Emotional Numbing or Suppression
Signs:
- Appears “cold” or detached from emotions
- Avoids talking about feelings entirely
- Uses substances, overeating, or overworking to block emotions
📍Why it’s dangerous: Suppressed emotions often resurface in unhealthy ways—like sudden rage, panic attacks, or addiction.
🌀 2. Constant Rumination or Overthinking
Signs:
- Replays the same negative thoughts or past mistakes
- Has trouble sleeping due to worry
- Often says “I can’t stop thinking about it.”
📍Why it’s dangerous: Increases anxiety, depression, and self-doubt—can lead to hopelessness or suicidal thoughts.
💣 3. Aggression or Outbursts
Signs:
- Explosive reactions to minor problems
- Verbal abuse or threats
- Breaking objects or physical fights
📍Why it’s dangerous: Hurts relationships, increases shame, and can escalate to legal or safety consequences.
🌫 4. Escape or Avoidance Behaviors
Signs:
- Sleeps excessively, binge-watches shows, or isolates for days
- Avoids responsibilities, conversations, or emotions
- Relies heavily on drugs, alcohol, gambling, or sex to cope
📍Why it’s dangerous: Doesn’t resolve underlying problems and increases risk of addiction and long-term dysfunction.
🔒 5. Withdrawal and Isolation
Signs:
- Stops answering calls or texts
- Pulls away from social or family activities
- Claims “I’m fine” but appears sad or flat
📍Why it’s dangerous: Isolation intensifies mental health symptoms and removes protective support systems.
❌ 6. Self-Blame or Worthlessness
Signs:
- Frequent self-criticism or guilt
- Says “It’s all my fault” or “I deserve this.”
- Engages in self-sabotaging behavior
📍Why it’s dangerous: Fuels depression, self-harm, or accepting abusive situations.
🧨 7. Risk-Taking or Self-Harm
Signs:
- Reckless driving, unsafe sex, or risky drug use
- Expresses thoughts of wanting to hurt themselves
- Physical signs of cutting, bruising, or burns
📍Why it’s dangerous: Immediate danger to life and a red flag for crisis intervention.
📞 When to Take Action
If someone shows any of the above warning signs consistently or severely, it’s critical to:
Remove means of harm if they’re at immediate risk (e.g., sharp objects, medications)
Start a nonjudgmental conversation: “I’m worried about you. You don’t seem like yourself lately.”
Encourage professional help: therapist, primary care, crisis text line (741741), or call/text 988
Conclusion
Addressing emotion-oriented coping styles is essential in preventing addiction, as unhealthy emotional responses can lead to harmful escape behaviors. By promoting self-management strategies, individuals can learn to regulate emotions in healthy ways. Family support creates a foundation of trust and openness, while community resources offer accessible tools and environments for healing. Together, these approaches foster emotional resilience and reduce the need for substances or behaviors to cope with distress.