The biopsychosocial assessment of chronic pain syndrome (CPS) evaluates the complex interplay of biological, psychological, and social factors affecting a patient’s experience. This approach offers advantages such as personalized treatment plans and improved patient outcomes, but it also presents challenges, including time constraints and potential patient resistance. Ethical dilemmas can arise around informed consent, privacy, and stigmatization. Effective implementation requires community resource strategies, including provider training, interdisciplinary collaboration, and patient support networks. These elements emphasize the importance of a holistic approach to chronic pain management that prioritizes patient well-being and equitable care.
Biopsychosocial Assessment of Chronic Pain Syndrome (CPS): A Comprehensive Approach to Pain Management
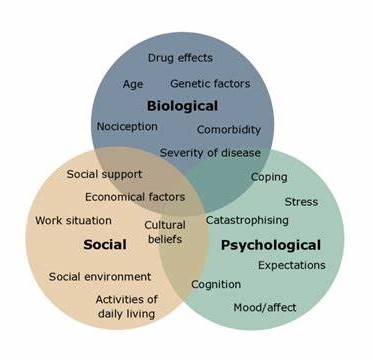
The biopsychosocial assessment of chronic pain syndrome (CPS) is an integrative evaluation that considers the biological, psychological, and social factors shaping an individual’s pain experience. This approach acknowledges that chronic pain is not solely a physical issue but is influenced by a complex web of factors. Here’s a closer look at each component:
1. Biological Factors
- Medical History: Review past and present conditions, injuries, and treatments.
- Pain Physiology: Assessment of pain characteristics—type, location, intensity, duration—and underlying conditions like arthritis.
- Medication Use: Evaluation of current medications, their efficacy, and potential side effects.
- Physical Health: Overall health overview, including comorbidities and lifestyle factors like diet and exercise.
2. Psychological Factors
- Mental Health Status: Screening for conditions such as depression and anxiety, which can influence pain perception and coping.
- Cognitive Patterns: Assessment of beliefs about pain, fear-avoidance, and any catastrophic thinking.
- Emotional Response: Exploration of pain’s impact on mood, motivation, and mental well-being.
- Coping Mechanisms: Evaluation of the patient’s pain management strategies and effectiveness.
3. Social Factors
- Support Systems: Assessment of support from family, friends, and community resources.
- Work and Occupational Impact: Consider how chronic pain affects work life and disability status.
- Socioeconomic Status: Evaluation of financial resources, healthcare access, and barriers to treatment.
- Cultural Influences: Exploration of cultural beliefs and attitudes toward pain may shape treatment decisions.
Importance of the Biopsychosocial Assessment
- Holistic Understanding: Provides a comprehensive view of the patient’s experience, allowing for tailored, multidimensional treatment plans.
- Improved Outcomes: By addressing pain from various angles, interventions can be more effective, leading to better management and quality of life.
- Patient-Centered Care: This approach engages patients in discussions about their pain from diverse perspectives, fostering collaborative care and enhancing patient satisfaction.
A biopsychosocial assessment of chronic pain offers an invaluable framework for understanding and treating pain by integrating biological, psychological, and social dimensions. This holistic approach leads to more personalized and effective pain management strategies, ultimately improving patient outcomes.
Why Conducting a Biopsychosocial Assessment is Essential for Chronic Pain Syndrome (CPS)
A biopsychosocial assessment for chronic pain syndrome (CPS) is critical for understanding and managing pain comprehensively. Here are some key reasons why this approach enhances patient care:
1. Holistic Understanding
- Comprehensive View: This assessment provides a complete picture of the patient’s pain by considering physical symptoms and psychological and social influences.
2. Tailored Treatment Plans
- Personalized Care: By identifying unique biological, psychological, and social factors, providers can create individualized treatment plans, increasing the likelihood of effective pain management.
3. Identifying Underlying Issues
- Root Causes: This approach helps uncover the underlying conditions or issues contributing to chronic pain, enabling more targeted and appropriate interventions.
4. Improved Patient Outcomes
- Enhanced Effectiveness: Addressing all aspects of pain often leads to better outcomes, as treatments that account for psychological and social factors are more likely to reduce pain and improve quality of life.
5. Enhanced Patient Engagement
- Collaboration in Care: Actively involving patients in discussions about their pain experience fosters collaboration and makes them more engaged in their treatment journey.
6. Effective Coping Strategies
- Coping Mechanisms: Assessing psychological factors can help identify effective coping strategies that reduce helplessness and improve resilience.
7. Better Resource Allocation
- Resource Identification: This assessment highlights the need for additional support resources, such as counseling or support groups, to ensure patients have comprehensive care.
8. Addressing Stigma and Misunderstanding
- Informed Perspectives: Recognizing the complex nature of chronic pain helps reduce stigma and misconceptions, fostering more empathetic and supportive care.
9. Facilitating Communication
- Interdisciplinary Collaboration: A biopsychosocial approach encourages communication among healthcare providers, leading to a more integrated treatment strategy that spans multiple specialties.
10. Long-Term Management
- Sustainable Strategies: By understanding the full scope of factors impacting chronic pain, providers can develop long-term management plans that minimize relapse and enhance overall well-being.
Conducting a biopsychosocial assessment for chronic pain allows providers to develop a nuanced understanding of pain, supporting personalized treatment strategies that address all aspects of the patient’s experience. This approach improves outcomes, empowers patients, reduces stigma, and promotes sustainable, compassionate care.
Challenges and Disadvantages of the Biopsychosocial Assessment for Chronic Pain Syndrome (CPS)
While the biopsychosocial assessment is a valuable tool for understanding and managing chronic pain syndrome (CPS), it comes with several challenges and potential disadvantages that healthcare providers should consider:
1. Time-Consuming Process
- Lengthy Consultations: A thorough biopsychosocial assessment requires extended time, which may be challenging in busy clinical environments.
2. Complexity of Assessment
- Multifaceted Nature: The assessment covers biological, psychological, and social domains, which can make it complex and sometimes make it difficult to interpret all aspects cohesively.
3. Need for Specialized Training
- Training Requirements: Conducting these assessments effectively often requires additional training, which may create implementation barriers in some healthcare settings.
4. Patient Engagement Challenges
- Varied Willingness: Some patients may be reluctant to discuss psychological or social factors, limiting the assessment’s effectiveness and scope.
5. Subjectivity in Responses
- Inconsistent Reporting: Self-reported data on psychological and social factors can be subjective, leading to inconsistencies or inaccuracies.
6. Resource Intensive
- Referral Needs: This assessment may necessitate referrals to mental health or social support services, which might not always be available or accessible.
7. Risk of Overwhelming Patients
- Information Overload: The assessment’s comprehensiveness may overwhelm some patients, especially if they feel pressured to address many areas simultaneously.
8. Measurement Difficulties
- Quantifying Psychological and Social Factors: Measuring these factors can be challenging, and the lack of standardized tools may reduce assessment reliability.
9. Risk of Over-Pathologizing
- Potential for Misinterpretation: There’s a risk of interpreting normal responses to pain as pathological, potentially leading to unnecessary treatments or increased patient anxiety.
10. Insurance and Reimbursement Issues
- Coverage Limitations: Some insurers may not cover the costs of a comprehensive biopsychosocial assessment, creating financial barriers for patients.
The biopsychosocial assessment for chronic pain provides a nuanced, comprehensive view of a patient’s pain experience, yet it requires careful consideration of these challenges. Balancing the benefits with these potential drawbacks can help optimize pain management while providing compassionate, effective care tailored to each individual’s unique needs. Addressing these challenges can ultimately improve patient engagement, assessment accuracy, and overall outcomes in chronic pain management.
Ethical Dilemmas in the Biopsychosocial Assessment of Chronic Pain Syndrome (CPS)
The biopsychosocial assessment of chronic pain syndrome (CPS) provides a well-rounded view of pain, but it also presents several ethical challenges that healthcare providers must navigate. Here are some of the critical ethical dilemmas:
1. Informed Consent
- Understanding the Assessment: Ensuring patients fully grasp the purpose and implications of the assessment can be challenging, raising concerns about genuinely informed consent.
2. Privacy and Confidentiality
- Sensitive Information: The assessment often involves personal discussions about mental health and social circumstances, underscoring the importance of maintaining strict confidentiality.
3. Risk of Stigmatization
- Judgment and Bias: Psychological and social factors might lead to unintentional stigma, potentially influencing treatment decisions or patient perceptions.
4. Overemphasis on Psychological Factors
- Balancing Perspectives: There’s a risk of focusing too much on psychological aspects, which can sometimes overshadow biological factors essential to effective pain management.
5. Patient Autonomy
- Respecting Choices: Some patients may wish to focus solely on physical symptoms, so they should not feel pressured into discussing other areas if it’s against their preferences.
6. Resource Allocation and Equity
- Access to Resources: Not all patients have equal access to mental health services or social support, raising ethical concerns about the fairness of comprehensive assessments.
7. Misinterpretation of Results
- Subjectivity in Data: Self-reported information can be open to interpretation, and misinterpretation may lead to clinical decisions that do not align with the patient’s actual needs.
8. Responsibility for Follow-Up Care
- Continuity of Care: Identifying additional issues, such as social or psychological needs, raises the question of the provider’s responsibility for ensuring appropriate follow-up.
9. Economic Considerations
- Costs of Assessment: Comprehensive assessments may be unaffordable for some, raising ethical concerns about financial accessibility and equitable care.
10. Impact on Therapeutic Relationship
- Trust and Rapport: If patients view the assessment as intrusive, it could impact their trust in their healthcare provider, potentially weakening the therapeutic relationship.
Addressing these ethical dilemmas requires transparent communication, respect for patient autonomy, and a patient-centered approach. Providers should aim to balance thorough assessments with sensitivity to each individual’s values, preferences, and unique needs. By navigating these ethical concerns thoughtfully, healthcare providers can foster a supportive environment that prioritizes patient well-being and equitable care in chronic pain management.
Enhancing Biopsychosocial Assessments of Chronic Pain Syndrome (CPS) Through Community Resource Strategies
Conducting practical biopsychosocial assessments for chronic pain syndrome (CPS) is crucial for understanding and managing pain holistically. To enhance the effectiveness and accessibility of these evaluations, communities can implement several key resource strategies:
1. Training and Education Programs
- Provider Workshops: Organize training sessions focused on the biopsychosocial model and assessment techniques for healthcare providers. This will improve their skills and confidence in conducting thorough evaluations.
2. Interdisciplinary Collaboration
- Team-Based Approach: Foster collaboration among healthcare professionals, including physicians, psychologists, and social workers, to ensure comprehensive assessments that address all dimensions of pain.
3. Community Health Fairs
- Outreach Initiatives: Host health fairs where community members can learn about chronic pain, the biopsychosocial model, and available resources, including screenings and assessments.
4. Support Groups and Peer Networks
- Shared Experiences: Create support groups for individuals with chronic pain to provide a space to discuss experiences, share coping strategies, and understand the importance of a holistic pain management approach.
5. Accessible Assessment Tools
- Standardized Instruments: Develop and distribute standardized questionnaires and assessment tools that healthcare providers can easily administer in various settings.
6. Online Resources and Telehealth
- Virtual Assessments: Utilizing telehealth platforms to conduct biopsychosocial assessments remotely makes it easier for patients to participate and access care from the comfort of their homes.
7. Community Education Campaigns
- Awareness Initiatives: Launch campaigns to educate the community about chronic pain and the biopsychosocial approach, highlighting the benefits of comprehensive assessments.
8. Resource Referral Networks
- Connecting Patients: Establish networks that connect patients with local resources, such as mental health services, physical therapy, and social support organizations, based on assessment findings.
9. Data Collection and Feedback
- Community Needs Assessment: Conduct surveys and collect data to understand better community needs related to chronic pain management, informing the development of targeted resources and programs.
10. Cultural Competency Training
- Inclusive Practices: Provide training for healthcare providers on cultural competence to ensure assessments are respectful and relevant to diverse patient populations.
11. Follow-Up Services
- Continuity of Care: Develop protocols for follow-up services and referrals based on assessment results, ensuring that patients receive comprehensive care beyond the initial assessment.
12. Advocacy for Policy Changes
- Improving Access: Advocate for policies that support funding and access to comprehensive pain management services, including biopsychosocial assessments.
Implementing these community resource strategies will create a supportive environment for conducting biopsychosocial assessments, ultimately leading to improved patient outcomes and enhanced chronic pain management. By prioritizing education, collaboration, and accessibility, communities can significantly impact the quality of care for those with chronic pain.
Conclusion
The biopsychosocial assessment of chronic pain is vital for understanding and addressing the multifaceted nature of pain. Its advantages, including personalized treatment and improved outcomes, underscore its importance in effective pain management. However, challenges such as time demands, potential patient resistance, and ethical dilemmas related to privacy and consent must be carefully navigated. Community resource strategies, such as training programs and interdisciplinary collaboration, are essential for facilitating this comprehensive assessment. By embracing a holistic approach, healthcare providers can enhance patient care, promote well-being, and ensure equitable access to effective pain management solutions.
Video: What’s REALLY Behind Your Chronic Pain?