Telehealth offers a modern solution for addiction cognitive behavioral therapy (CBT), enabling convenient and accessible treatment delivery through digital platforms. While advantageous for its convenience and expanded reach, telehealth also poses challenges, including technological limitations and ethical concerns. Integrating self-management, family support, and community resource strategies is essential to optimize its effectiveness.
Telehealth for Cognitive Behavioral Therapy (CBT)
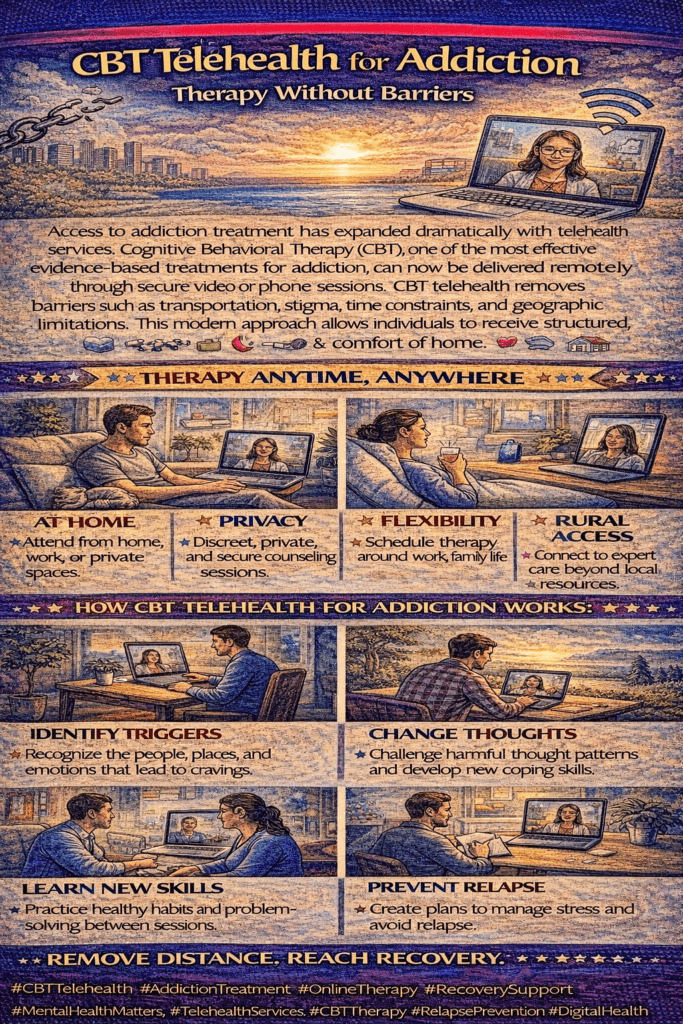
Telehealth for cognitive-behavioral therapy (CBT) leverages virtual platforms to deliver therapy sessions remotely, allowing therapists and clients to interact in real time via video conferencing software. This approach enables face-to-face interaction while offering several benefits:
- Accessibility: Clients can engage in therapy from the comfort of their own homes, eliminating travel barriers and enhancing access to mental health services. This is especially beneficial for individuals in rural areas or those with mobility challenges.
- Flexibility: Telehealth platforms offer flexible scheduling, allowing clients to arrange sessions at times that suit them. This adaptability can lead to improved adherence to treatment plans.
- Confidentiality: Telehealth maintains the confidentiality and privacy of therapy sessions, as communication occurs in a secure online environment. This reassurance can help clients feel more comfortable sharing their thoughts and feelings.
- Enhanced Resources: Therapists can utilize digital tools and resources during sessions to strengthen the effectiveness of CBT. This may include online worksheets, mood-tracking apps, and interactive exercises that can be easily shared and accessed.
- Effectiveness: Research indicates that telehealth CBT can be equally effective as traditional in-person therapy for treating various mental health concerns when delivered by trained professionals. The techniques used in CBT, such as identifying and challenging negative thought patterns, goal-setting, and developing coping strategies, can seamlessly translate to the online format.
While telehealth CBT sessions may differ slightly from face-to-face interactions, the overall effectiveness and convenience make them a valuable option for many individuals seeking mental health support. As telehealth evolves, it offers a promising solution for enhancing access to quality mental health care.
Telehealth in Addiction Treatment: Expanding Access and Support
Telehealth has significantly expanded access to various addiction treatment modalities, providing remote support and intervention for individuals struggling with substance use disorders. Here are some fundamental approaches that can be effectively delivered through telehealth:
- Therapy Sessions: Evidence-based therapies such as cognitive-behavioral therapy (CBT) and motivational interviewing can be conducted via video conferencing platforms. These sessions focus on identifying triggers, developing coping skills, and addressing underlying issues that contribute to addiction.
- Support Groups: Telehealth platforms facilitate virtual support groups, allowing individuals in recovery to connect with peers, share experiences, and receive encouragement from others who understand their struggles. This sense of community is essential for fostering recovery.
- Medication-Assisted Treatment (MAT) Management: Healthcare providers can remotely prescribe and monitor medications for addiction treatment, such as buprenorphine or naltrexone. Regular video check-ins enable effective medication management and adjustment as needed.
- Psychoeducation: Telehealth sessions can include educational components that cover addiction, relapse prevention strategies, stress management techniques, and healthy coping mechanisms. These resources empower individuals on their recovery journey.
- Case Management and Care Coordination: Telehealth platforms enhance communication among individuals in recovery, healthcare providers, therapists, and other members of the treatment team, ensuring comprehensive and coordinated care.
- Family Therapy: Telehealth allows family members to participate in therapy sessions remotely. These sessions address family dynamics, communication patterns, and support strategies to enhance the individual’s recovery.
- Peer Support and Coaching: Certified recovery coaches or peer support specialists can provide guidance, accountability, and encouragement through virtual sessions and check-ins, helping individuals navigate their recovery journeys.
Overall, telehealth offers a convenient, accessible, and effective means of delivering addiction treatment and support services, particularly in situations where in-person visits may be challenging or limited. This approach not only enhances access to care but also promotes a supportive environment for individuals seeking to overcome substance use disorders.
Advantages of Telehealth for Delivering Addiction Cognitive Behavioral Therapy (CBT)
Telehealth has transformed the delivery of addiction cognitive behavioral therapy (CBT), offering several advantages that enhance access and effectiveness for individuals seeking treatment. Here are some key benefits:
- Accessibility: Telehealth eliminates geographical barriers, allowing individuals to access CBT from the comfort of their homes or any location with internet access. This is particularly beneficial for those in rural or remote areas with limited access to addiction treatment services.
- Convenience: With flexible scheduling, telehealth reduces the need for travel to a physical location for therapy sessions. This convenience improves treatment adherence and engagement by accommodating busy schedules and minimizing logistical challenges.
- Privacy and Confidentiality: Telehealth sessions can be conducted in private settings chosen by the individual, promoting confidentiality and reducing the stigma associated with attending in-person therapy. This environment may encourage those hesitant about seeking treatment due to privacy concerns to take that step.
- Cost-Effectiveness: Telehealth makes addiction treatment more affordable and accessible to a broader range of individuals by eliminating transportation costs and the time off work or childcare arrangements required for in-person visits.
- Continuity of Care: Telehealth enables seamless continuity of care, allowing individuals to maintain regular therapy sessions despite travel restrictions, inclement weather, or other disruptions. This consistency supports ongoing progress and prevents treatment interruptions.
- Customization and Personalization: Telehealth platforms often offer features that enable therapists to customize treatment plans and deliver personalized interventions tailored to each individual’s unique needs and preferences. This individualized approach enhances treatment effectiveness and engagement.
- Technology Integration: Many telehealth platforms integrate with mobile apps and digital tools, allowing for self-monitoring, homework assignments, and therapeutic exercises. This technology integration enhances treatment outcomes and empowers individuals to participate actively in their recovery.
Telehealth offers numerous advantages for delivering addiction CBT, including improved access, convenience, privacy, cost-effectiveness, continuity of care, customization, and technology integration. These benefits contribute to a more accessible, engaging, and effective addiction treatment experience for individuals on their path to recovery.
Disadvantages of Telehealth for Addiction Cognitive Behavioral Therapy (CBT)
While telehealth has transformed addiction cognitive behavioral therapy (CBT) by offering numerous advantages, it also presents several challenges that can impact the effectiveness of treatment. Here are some key disadvantages:
- Technology Barriers: Not everyone has access to the necessary technology or reliable internet connections for telehealth sessions. This can create disparities in access to care, particularly for individuals in rural areas, low-income communities, or those who lack technical skills.
- Digital Divide: Even if individuals can access technology, they may lack digital literacy skills or feel uncomfortable using telehealth platforms. This discomfort can hinder their ability to fully engage in therapy sessions and derive the maximum benefit from treatment.
- Lack of Nonverbal Cues: Telehealth sessions may miss nonverbal cues, such as body language and facial expressions, that are present in face-to-face interactions. This can make it more difficult for therapists to accurately assess clients’ emotional states and adjust their therapeutic approaches accordingly.
- Privacy Concerns: While telehealth platforms strive for confidentiality, clients may still worry about data security and the potential for breaches of sensitive information. This anxiety can discourage individuals from discussing personal matters openly during digital sessions.
- Technological Glitches: Technical issues, such as poor internet connectivity, audio/video lag, or platform malfunctions, can disrupt therapy sessions. These interruptions can frustrate clients and therapists, detracting from the therapeutic process and hindering progress.
- Limited Treatment Modalities: Some therapeutic interventions, particularly those that require experiential or hands-on techniques, may be difficult to replicate effectively in telehealth. This limitation can impact the range of treatment options available to clients and potentially influence treatment outcomes.
- Potential for Distractions: Conducting telehealth sessions from home or other non-clinical environments may expose clients to distractions, including household noise and interruptions from family members. These disruptions can interfere with the therapeutic process and diminish the quality of interactions.
- Loss of Personal Connection: Telehealth may lack the interpersonal connection and rapport that often develop more naturally in face-to-face settings. Some clients might find it challenging to establish trust and feel fully understood by their therapist through a digital platform.
Overall, while telehealth offers significant benefits for delivering addiction CBT, it also introduces challenges related to technology barriers, privacy concerns, limited treatment modalities, and potential disruptions. Addressing these disadvantages proactively is essential for optimizing the effectiveness of telehealth-based addiction treatment.
Ethical Dilemmas in Telehealth for Addiction Cognitive Behavioral Therapy (CBT)
Telehealth for addiction cognitive behavioral therapy (CBT) introduces a range of ethical dilemmas that both therapists and clients may encounter. Addressing these dilemmas is essential for providing effective and responsible care. Here are some key ethical considerations:
- Confidentiality and Privacy: Ensuring the confidentiality and privacy of client information during telehealth sessions can be challenging. Therapists must proactively secure electronic communications and protect sensitive data from unauthorized access or disclosure.
- Informed Consent: Obtaining informed consent for telehealth services involves explaining the potential risks and benefits of remote therapy and discussing alternative treatment options. Therapists must ensure that clients fully understand the nature of telehealth and provide consent voluntarily.
- Cultural Competence: Telehealth therapists must be culturally competent and sensitive to their clients’ diverse backgrounds and identities. Understanding how cultural factors shape clients’ experiences with telehealth is vital to providing effective, respectful care.
- Technological Competence: Therapists offering telehealth services must possess the necessary technological skills to navigate telehealth platforms effectively. Additionally, they should ensure that clients are comfortable using the technology and provide assistance as needed to overcome barriers to access.
- Boundaries and Dual Relationships: Maintaining appropriate boundaries in telehealth therapy sessions is crucial to upholding professional ethics and preventing potential dual relationships. Therapists must establish clear guidelines for communication and interaction with clients outside of scheduled sessions to avoid conflicts of interest or boundary violations.
- Emergency Situations: Addressing emergencies or crises during telehealth sessions can be challenging, primarily if therapists cannot assess clients or provide immediate physical assistance. Therapists must have protocols for managing emergencies remotely and collaborating with local resources to ensure clients receive timely and appropriate care.
- Equitable Access: Ensuring equitable access to telehealth services for all clients, regardless of socioeconomic status or geographic location, raises ethical considerations. Therapists should strive to minimize barriers to access and advocate for policies that promote affordable and inclusive telehealth options for underserved populations.
- Quality of Care: Maintaining the quality of care in telehealth settings requires therapists to adapt evidence-based treatment approaches effectively to the digital environment. They must continually assess the effectiveness of telehealth interventions and address any limitations or challenges that may impact treatment outcomes.
Navigating these ethical dilemmas requires therapists to adhere to professional codes of ethics, maintain ongoing training and education in telehealth practice, and prioritize their clients’ well-being and autonomy in all aspects of treatment delivery. By doing so, therapists can ensure that they provide ethical, effective, and compassionate care in the evolving landscape of telehealth.
Empowering Recovery: Self-Management Strategies for Telehealth Addiction Cognitive Behavioral Therapy (CBT)
Self-management strategies for telehealth addiction cognitive behavioral therapy (CBT) focus on empowering clients to take an active role in their recovery process. These strategies help individuals develop skills to manage their thoughts, emotions, and behaviors, ultimately enhancing their recovery journey. Here are several effective self-management strategies tailored for telehealth CBT:
- Goal Setting: Encourage clients to establish specific, measurable, achievable, relevant, and time-bound (SMART) goals for their recovery. Collaborate with them to identify short- and long-term objectives to reduce substance use, develop coping skills, and improve overall well-being.
- Coping Skills Practice: Teach clients various coping skills to manage cravings, stress, and triggers associated with addiction. Utilize telehealth sessions to demonstrate relaxation exercises, mindfulness meditation, and thought-restructuring techniques. Encourage clients to practice these skills between sessions to reinforce learning.
- Behavioral Activation: Help clients engage in meaningful, rewarding activities to improve their mood and reduce cravings for substances. Work together to identify enjoyable activities aligned with their values and interests and support them in scheduling them into their daily routines.
- Thought Monitoring and Reframing: Help clients recognize and challenge negative thought patterns and cognitive distortions that contribute to addictive behaviors. Encourage them to maintain thought records or journals to track their thoughts and associated emotions, and guide them in reframing unhelpful thoughts with more balanced, realistic perspectives.
- Relapse Prevention Planning: Collaborate with clients to develop personalized relapse prevention plans. Identify potential triggers and warning signs and discuss coping strategies to prevent relapse. Explore healthy mechanisms to manage cravings or setbacks, empowering clients to navigate high-risk situations effectively.
- Self-Care Practices: Emphasize the importance of self-care in maintaining overall well-being during addiction recovery. Encourage clients to prioritize activities that support physical, mental, and emotional well-being, including exercise, nutrition, sleep hygiene, social support, and leisure activities.
- Problem-Solving Skills: Teach clients effective problem-solving techniques to address challenges and obstacles they may encounter in their recovery journey. Guide them through a structured problem-solving process: define the problem, generate potential solutions, evaluate alternatives, implement a plan of action, and review outcomes.
- Mindfulness and Acceptance: Introduce mindfulness and acceptance-based strategies to help clients develop nonjudgmental awareness of their thoughts, feelings, and sensations. Guide clients in mindfulness exercises, such as mindful breathing or body scans, to increase present-moment awareness and reduce reactivity to cravings or distressing emotions.
By encouraging clients to integrate these self-management strategies into their daily lives, therapists can enhance their sense of empowerment, self-efficacy, and resilience in overcoming the challenges of addiction. Regularly assessing clients’ progress and providing feedback will further reinforce their efforts toward positive change, fostering a supportive environment for recovery through telehealth CBT.
Strengthening Recovery: Family Support Strategies for Telehealth Addiction Cognitive Behavioral Therapy (CBT)
Family support is a crucial component of addiction recovery, particularly when utilizing telehealth cognitive behavioral therapy (CBT). Engaging family members in recovery can enhance communication and problem-solving skills and create a supportive home environment. Here are several family support strategies tailored for telehealth CBT:
- Psychoeducation: Begin by providing family members with information about addiction, the principles of CBT, and the vital role of family support in recovery. Educating them about the challenges their loved one may face helps foster understanding and reinforces the importance of their involvement in the treatment process.
- Family Therapy Sessions: Conduct telehealth sessions to address family dynamics, communication patterns, and relationship issues that may affect the individual’s recovery. These sessions provide a platform for family members to share their perspectives, concerns, and goals related to their loved one’s recovery journey.
- Setting Boundaries: Assist family members in establishing clear and healthy boundaries to protect their own well-being while supporting their loved ones in recovery. Discuss strategies for limiting enabling behaviors, managing conflicts, and fostering accountability within the family system.
- Communication Skills Training: Teach family members effective communication techniques, such as active listening, assertiveness, and empathy. These skills facilitate open and honest discussions about addiction-related issues, encouraging respectful dialogue and collaborative problem-solving to tackle challenges as a family unit.
- Emotional Support: Offer emotional support to family members who may experience stress, anxiety, or guilt related to their loved one’s addiction. Validate their feelings and provide a safe space to express their emotions without judgment. Encourage self-care practices and coping strategies to manage stress and maintain their well-being.
- Relapse Prevention Planning: Involve family members in developing personalized relapse prevention plans. Identify potential triggers and warning signs, and collaboratively create strategies to prevent relapse. This proactive approach fosters a supportive home environment that encourages healthy coping mechanisms.
- Encouraging Involvement in Support Groups: Participation in family support groups or mutual aid organizations, such as Al-Anon or Nar-Anon, is recommended. These groups allow family members to connect with others who understand their experiences and provide peer support and guidance.
- Celebrating Milestones and Progress: Acknowledge and celebrate the individual’s milestones and progress in recovery as a family. Recognizing achievements, no matter how small, helps reinforce positive behavior and fosters encouragement, pride, and support for their efforts toward change.
Implementing these family support strategies through telehealth platforms can help families play a vital role in enhancing their loved one’s motivation, accountability, and resilience in addiction recovery. Regular communication, collaboration, and support can strengthen family relationships and contribute to positive long-term recovery outcomes.
Enhancing Recovery: Community Resource Strategies for Telehealth Addiction Cognitive Behavioral Therapy (CBT)
Community resource strategies play a vital role in supplementing telehealth cognitive behavioral therapy (CBT) for individuals struggling with addiction. By connecting clients with external support services and resources available within their communities, these strategies can enhance the recovery journey and provide additional assistance beyond therapy sessions. Here are some effective community resource strategies tailored for telehealth CBT:
- Referrals to Local Support Groups: Provide clients with information and referrals to local support groups or peer-led recovery meetings, such as Alcoholics Anonymous (AA) or Narcotics Anonymous (NA). These groups offer vital peer support, encouragement, and a sense of belonging, which are essential for individuals struggling with addiction.
- Access to Virtual Support Networks: Connect individuals with online forums, chat rooms, or virtual support networks designed for addiction recovery. These platforms allow clients to interact with peers, share experiences, and access support resources from the comfort of their own homes, fostering a sense of community.
- Collaboration with Community Health Centers: Partner with local community health centers or clinics to facilitate access to medical services, medication-assisted treatment (MAT), and primary care for individuals with co-occurring medical conditions or complex healthcare needs. This collaboration ensures comprehensive support for clients.
- Psychoeducation Workshops: Offer virtual workshops or seminars covering addiction-related topics, coping skills, relapse-prevention strategies, and mental health wellness. These educational sessions empower individuals with essential knowledge and skills to support their recovery journey.
- Access to Teletherapy Apps and Platforms: Recommend teletherapy apps or online counseling platforms that offer convenient, affordable access to licensed therapists, counselors, or peer support specialists. These digital resources offer additional avenues for therapeutic support and guidance.
- Online Recovery Resources: Direct clients to reputable websites, online resources, and educational materials related to addiction recovery, mental health, and overall well-being. These resources may include articles, videos, self-help tools, and recovery-focused apps designed to support individuals in their journey to sobriety.
- Community-Based Wellness Activities: Encourage participation in community-based wellness activities such as virtual fitness classes, mindfulness meditation sessions, art therapy workshops, or recreational programs. Engaging in positive and enriching activities can promote holistic well-being and reduce the risk of relapse.
- Collaboration with Peer Recovery Coaches: Facilitate connections with peer recovery coaches or mentors who have lived experience with addiction recovery. These specialists offer empathy, guidance, and practical advice drawn from their recovery journeys, serving as role models and sources of inspiration for clients.
By leveraging these community resource strategies alongside telehealth addiction CBT, individuals can access a comprehensive network of support and resources to facilitate their recovery. These community-based initiatives complement therapeutic interventions, empowering individuals to achieve sustained sobriety and well-being. Engaging with community resources can significantly enhance the effectiveness of telehealth services, making the recovery journey more supportive and enriching.
Frequently Asked Questions
Here are some common questions:
What is CBT telehealth for addiction?
CBT telehealth provides Cognitive Behavioral Therapy for addiction through secure video or phone sessions instead of in-person office visits.
Is CBT effective for treating addiction?
Yes. CBT is one of the most evidence-based therapies for addiction, helping individuals change harmful thought patterns and behaviors.
Can CBT really work through telehealth?
Yes. Research shows CBT delivered through telehealth is just as effective as in-person therapy for many individuals.
What happens during a CBT telehealth session?
A therapist helps identify triggers, challenge negative thinking, develop coping strategies, and build relapse-prevention skills.
Do I need special technology for CBT telehealth?
Only a phone, tablet, or computer with internet access and a private space for sessions.
Is CBT telehealth private and confidential?
Yes. Sessions use secure, HIPAA-compliant platforms to protect confidentiality.
Who benefits most from CBT telehealth?
People with transportation barriers, busy schedules, rural locations, mobility limitations, or concerns about stigma benefit greatly.
Can CBT telehealth help with cravings?
Yes. CBT teaches practical tools to manage cravings and respond to triggers effectively.
Does CBT telehealth replace medication-assisted treatment?
No. It works best when combined with medical care or medication when appropriate.
How do I start CBT telehealth for addiction?
Contact a licensed therapist, addiction clinic, or telehealth provider to schedule an initial assessment.
Conclusion
Telehealth presents a promising avenue for addiction cognitive behavioral therapy, offering convenience and accessibility to individuals seeking treatment. Despite its advantages, telehealth has its share of challenges, including technological limitations and ethical dilemmas. However, by integrating self-management techniques, leveraging family support, and utilizing community resources, the potential of telehealth in delivering effective addiction CBT can be maximized. With careful consideration of its benefits and limitations and proactive strategies, telehealth stands poised to play a crucial role in expanding access to addiction treatment and improving outcomes for individuals in need.
Video: How to Break Addiction Without Leaving Home #OnlineTherapy #DigitalHealth