Stem cell research has long captured attention, especially in areas like injury repair, degenerative diseases, and regenerative medicine. Recently, the potential for stem cells to support addiction recovery is gaining traction among scientists, clinicians, and the general public. Addiction to drugs and alcohol is a complex challenge, and researchers are constantly exploring new ways to improve treatment outcomes. Stem cells may offer a novel approach by helping repair brain pathways affected by substance use, reducing cravings, or supporting neurological recovery. In this article, I’ll look at how stem cells could transform addiction treatment, summarize the latest research, discuss possible risks and limitations, and offer practical guidance for those curious about integrating these emerging options into recovery strategies. Understanding this evolving field is essential for anyone interested in cutting-edge approaches to addiction care.
Why Are People Talking About Stem Cells in Addiction Recovery?
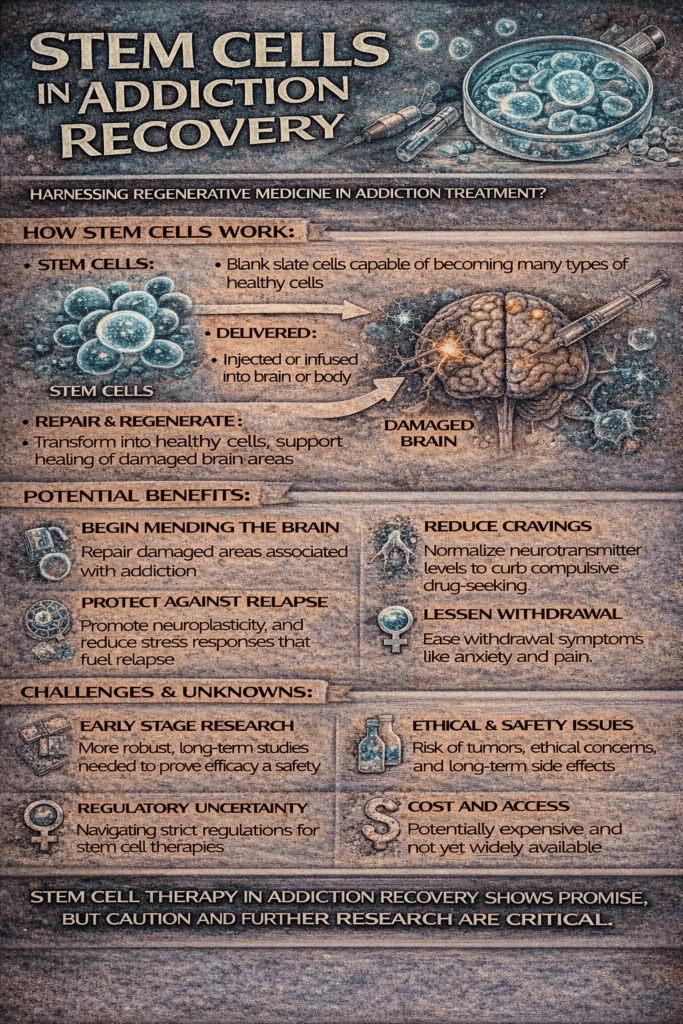
Addiction puts a lot of stress on the brain and body, often changing the way nerve cells communicate and work. Traditional treatment methods, such as therapy, medication, and community support, help. However, plenty of people still struggle with relapse and long-term recovery. This is where the concept of using stem cells comes in. Because stem cells have the power to repair or replace damaged cells, some scientists believe they might be able to mend or even rewire parts of the brain affected by addiction.
Interest in this idea is fueled by stem cells’ promise in treating conditions like spinal cord injuries, Parkinson’s disease, and even stroke. If these cells can repair nerves or rebuild brain pathways, they could reawaken areas harmed by years of substance use, potentially restoring function and hope where there was loss.
Some early studies suggest stem cells might help curb cravings or lessen withdrawal symptoms by restoring balance in the brain’s reward system. While the research is still in its early days, there’s real curiosity and excitement about what this could mean for people working to stay clean over the long haul.
How Could Stem Cells Help in Addiction?
Stem cells are unique because they can turn into many different types of cells. If some areas of the brain or nervous system are damaged by drugs, alcohol, or other addictive substances, stem cells might be able to help by rebuilding those parts. Here’s how they might fit in:
- Repairing Brain Circuits: Addiction usually disrupts nerves that release dopamine, the so-called “feel-good” chemical. Repeated substance use can damage these cells, making it challenging to feel pleasure without drugs or alcohol. If stem cells could replace or fix these damaged nerves, it’s possible that mood and motivation could bounce back, making recovery more possible.
- Reducing Inflammation: Addiction is linked to inflammation in the brain. While more well-known for helping with inflammation elsewhere, research shows that stem cells might also help ease inflammation related to addiction-induced brain injuries.
- Promoting New Growth: In preclinical trials mainly involving animal models, certain types of stem cells have sparked the growth of new nerve cells in brain reward centers. This could be essential in feeling less reliant on addictive substances.
While all these possibilities sound eye-catching, it’s crucial to remember that nearly all current research is still in the early stages. The effectiveness of these drugs in humans hasn’t yet been fully proven in large clinical trials.
What’s Going On With Current Stem Cell Research?
Most of our current knowledge comes from animal studies or basic science experiments, rather than large-scale human trials. For instance, in rats addicted to morphine, some stem cell treatments led to less intense withdrawal. Other research focuses on how stem cells could restore dopamine release or fix neural circuits usually impaired by drugs.
A significant focus is on mesenchymal stem cells (MSCs), which are found in bone marrow, fat, or umbilical cords, and are good at repairing tissues and calming immune responses. Early evidence suggests that MSCs could help reverse some damage done by substances like opioids or alcohol. A study published in Scientific Reports reported that MSCs could cut the severity of opioid withdrawal in animal models. But to see these results make sense in the real world for people, more thorough testing is needed.
Another fundamental question concerns the best source of stem cells—should they be taken from the person receiving treatment, a donor, or grown in a lab? Also, deciding whether to inject, implant, or use other methods is an ongoing debate. These details matter, and researchers are still sorting them out.
Besides opioids and alcohol, some early research is starting to branch out to examine substance-related damage from drugs like methamphetamine and cocaine. Because these substances affect the brain in different ways, stem cell research in addiction is becoming more nuanced, exploring not just general brain repair but how specific drugs affect distinct neural networks. Researchers are also looking into how stem cells interact with genetics, age, and overall health to determine who might benefit most from these therapies.
What to Know Before Considering Stem Cell Therapy for Addiction
The idea of stem cells as a way to give addiction recovery a boost sounds tempting, but there are essential factors to consider:
- Evidence Is Still Limited: There aren’t many widely accepted, peer-reviewed studies showing that stem cell therapies work for addiction. Most treatments are viewed as experimental, with insurance rarely covering them.
- Regulation and Safety: In many countries, stem cell clinics are sometimes underregulated. This can lead to clinics offering treatments that lack thorough studies or safety guarantees—research carefully (and talk with your doctor) before considering this option. The FDA has warned against untested stem cell options in the US, so watch out for questionable clinics or bold promises without research backing.
- Costs: Because they are experimental, these treatments are not mainstream and can come with a hefty price tag—sometimes thousands out of pocket.
- Not a Standalone Fix: Even if stem cell therapies show promise, most experts believe they should be paired with established approaches, such as behavioral therapy, medication-assisted treatment, and counseling.
If interested, it’s best to check in on legitimate clinical trials. Sites like clinicaltrials.gov provide up-to-date registries about what’s being tried, who’s running studies, and what researchers hope to learn.
Challenges and Potential Drawbacks
- Long-Term Effects Unknown: It’s still unclear how people might respond five or ten years after getting stem cell therapy for addiction. Since medicine often means waiting for data over time, patience is necessary as science continues.
- Possible Side Effects: Any new or experimental therapy has risks, such as immune responses or infection. Different people can react differently, and these unknowns add a layer of uncertainty.
- Misleading Claims: Some clinics and websites push big promises without enough, if any, evidence. Always look for endorsements from trusted health authorities and double-check for findings in peer-reviewed medical journals.
Counting on stem cells as a “magic bullet” isn’t realistic. Addiction recovery blends biology with social, emotional, and behavioral factors. Even modern treatments work best with a strong support network and regular counseling or group meetings.
Where Do I See Stem Cells Fitting into the Future of Addiction Recovery?
Right now, stem cells are shaping up to be a possible bonus tool in the broader toolkit of addiction recovery—not a replacement for proven methods. In a few years, with more insights from research, some rehab centers may start weaving stem cell-based strategies into their recovery programs. Until then, therapy, medication, and a supportive community remain the main ingredients for successful recovery.
Practical uses down the line could include support for people experiencing chronic relapse or for those who haven’t seen results from traditional methods—but any broad use depends on big clinical studies confirming their effectiveness and safety first.
Additionally, some folks deal with liver or heart issues from long-term substance use. As stem cell therapy has helped restore tissue in other conditions, it could one day help those healing from physical damage caused by addiction, beyond supporting new habits or dampening cravings.
Scientists are also examining the potential for personalized or targeted treatments. Future stem cell therapies might one day be matched to a person’s genetic makeup, drug history, or brain scans, giving an individually tailored approach. This personalized medicine could be a game-changer, especially for those who don’t respond to broad treatments. However, this approach is still a few steps away and would need thorough testing and ethical oversight.
Frequently Asked Questions
Wondering how stem cells could shake up addiction recovery? Here are some questions people ask a lot:
Q: Are stem cell therapies for addiction available now?
A: For most people, well-tested stem cell treatments for addiction aren’t available outside proper clinical trials. Be wary of clinics offering quick and guaranteed outcomes.
Q: How is stem cell therapy different from traditional treatment?
A: Stem cell therapy aims to rebuild or fix damaged cells, while traditional approaches focus on behavior, medication, and treatment. Likely, both will give their best results when combined, not by replacing each other.
Q: How do I get involved in a stem cell clinical trial?
A: The best next move is to check public clinical trial registries and speak with a doctor, addiction specialist, or psychiatrist who keeps up-to-date with ongoing research.
Final Thoughts on Stem Cells and Addiction Recovery
The big picture is this: stem cell therapies hold some next-level cool potential to benefit addiction recovery, but we’re still a few steps away from their mainstream use. The science is promising, but far from settled. Sticking with proven treatments for now, staying interested in new developments, and having open conversations with your medical providers is the most innovative course for anyone eyeing the next phase of addiction recovery.
Addiction recovery is a marathon, not a sprint. While new tech, such as stem cells, may offer a fresh boost in the future, I recommend using a balanced approach—mixing the latest science with traditional support—for most people.
Video: Stem Cells in Addiction Recovery