Biological markers (biomarkers) offer a promising approach to addiction treatment by enabling personalized care through insights into genetic, biochemical, and neurological factors. They improve diagnosis and treatment monitoring but also pose challenges, including high costs, complexity, and potential over-reliance on biological data. Ethical concerns include privacy, discrimination, and stigmatization, especially for vulnerable groups. Community resource strategies, such as public education, ethical protections, and equitable access, are crucial for responsibly integrating biomarkers into addiction care.
How Biomarkers Are Revolutionizing Addiction Treatment: Tailoring Therapies for Better Outcomes
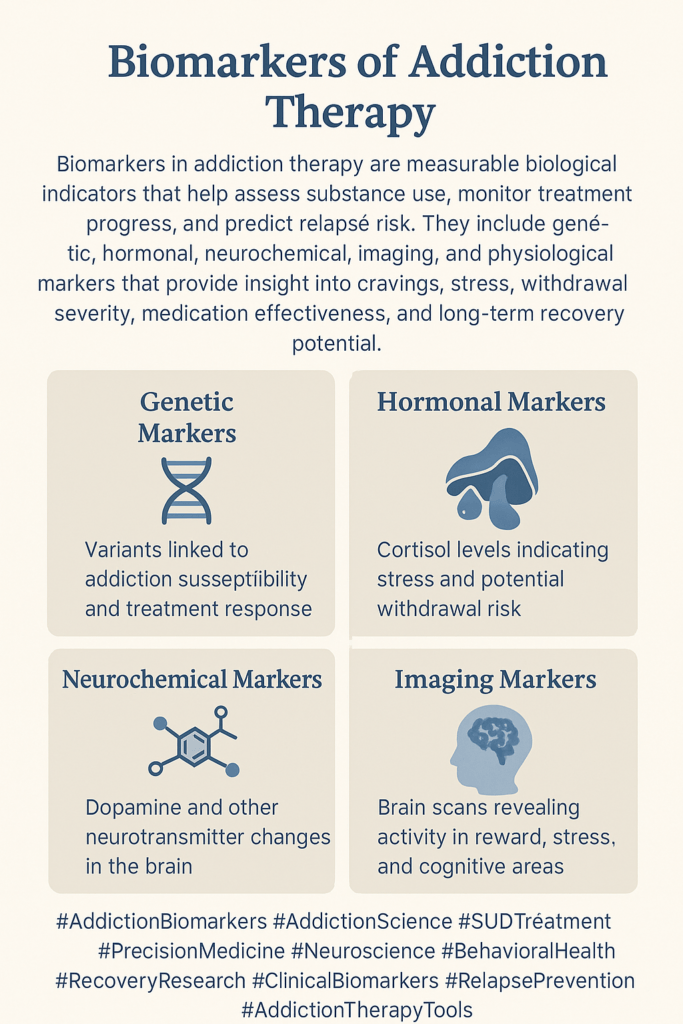
In recent years, the field of addiction treatment has evolved with the incorporation of biological markers or biomarkers, offering new hope for personalized care. Biomarkers provide objective measures of how a patient’s body responds to substances and treatments, helping to predict treatment outcomes, monitor progress, and assess the risk of relapse. By identifying the specific biological aspects of a patient’s addiction, healthcare providers can tailor therapies, leading to more effective results.
Here are some key categories of biomarkers used in addiction treatment:
1. Genetic Markers
Genetic Variants: Certain genes may predispose individuals to addiction or influence how they respond to treatment. Variations in genes like DRD2 and ANKK1 (related to dopamine receptors) can impact how a person reacts to alcohol or opioid treatments, providing clues for more targeted therapies.
Pharmacogenomics: This field focuses on tailoring treatment based on genetic differences. For instance, patients with specific opioid receptor gene variants may have better responses to medications such as naltrexone for opioid use disorder.
2. Neuroimaging Biomarkers
Structural and Functional MRI: Advanced imaging techniques, such as MRI and PET scans, can detect changes in brain regions affected by addiction, such as the prefrontal cortex and limbic system. For instance, reduced prefrontal cortex activity might indicate a higher risk of relapse.
Resting-State Connectivity: This measures how different brain areas communicate at rest, providing insight into relapse risk or treatment success.
3. Neurochemical Biomarkers
Dopamine: Central to the brain’s reward system, dopamine dysfunction is often linked to addiction. Monitoring dopamine levels or receptor sensitivity can guide treatments, especially for stimulant or alcohol addiction.
Glutamate and GABA: These neurotransmitters regulate excitatory and inhibitory signals in the brain. Abnormalities in their functioning are associated with addiction. Targeting these pathways, such as with medications like acamprosate for alcohol addiction, may improve outcomes.
4. Endocrine Biomarkers
Cortisol: Addiction frequently disrupts the hypothalamic-pituitary-adrenal (HPA) axis, which governs the body’s stress response. Abnormal cortisol levels may predict relapse risk or indicate the need for stress-related interventions in treatment.
Leptin and Ghrelin: These hunger-related hormones also play roles in reward processing. Monitoring their levels can offer insights into addiction, particularly with substances like alcohol and nicotine.
5. Inflammatory and Immune Markers
Cytokines: Chronic drug or alcohol use can trigger systemic inflammation. Elevated levels of pro-inflammatory cytokines like IL-6 and TNF-α have been linked to more severe addiction and poorer treatment responses.
Microglia Activation: In the brain, microglia act as immune cells that can become activated by substance use, contributing to neuroinflammation. This activation may predict how well a patient will respond to treatment.
6. Epigenetic Markers
DNA Methylation: Epigenetic modifications, such as adding methyl groups to DNA, can influence gene expression without changing the underlying genetic code. These changes, induced by drug use, could help predict treatment success.
Histone Modification: Drug exposure can alter histones, proteins that help regulate DNA. These modifications may play a role in the severity of addiction and how patients respond to therapy.
7. Proteomic and Metabolomic Markers
Proteins in Blood or Cerebrospinal Fluid: Levels of specific proteins, such as BDNF (Brain-Derived Neurotrophic Factor), may indicate brain plasticity and resilience during recovery from addiction.
Metabolite Profiles: Since substance use alters metabolism, specific metabolic changes may serve as biomarkers, helping clinicians track treatment progress or detect relapse early.
8. Behavioral and Physiological Markers
Heart Rate Variability (HRV): Disruptions in the autonomic nervous system due to substance use often show up as changes in HRV. Higher HRV during treatment is typically associated with better stress regulation and lower risk of relapse.
Pupillometry: Measuring changes in pupil size in response to stimuli provides insights into the brain’s reward system, making it helpful in assessing cravings or treatment responses.
Biomarkers are paving the way for more personalized and effective addiction treatments. By identifying the unique biological signatures of a patient’s addiction, clinicians can tailor therapies to their specific needs, enhancing the likelihood of success and reducing the chances of relapse. As research in this field progresses, biomarkers will likely play an increasingly pivotal role in shaping the future of addiction treatment.
The Benefits of Biomarkers in Addiction Treatment: A Path to Personalized and Effective Care
Biological markers, or biomarkers, are transforming the field of addiction treatment by providing measurable, objective indicators of how individuals respond to substances and therapies. These biomarkers can guide more precise and personalized treatment strategies, ultimately improving outcomes. Here are the key benefits of using biomarkers in addiction treatment:
1. Personalized Treatment Plans
Tailoring Interventions: Biomarkers allow customized treatment plans based on a person’s unique biological makeup, such as their genetic profile or neurochemical imbalances. This eliminates the need for a trial-and-error approach, enabling clinicians to select the most effective treatment.
Pharmacogenomics: Genetic markers can predict how patients metabolize and respond to specific medications. For example, individuals with certain genetic variants might respond better to naltrexone for alcohol use disorder or methadone for opioid addiction, leading to more targeted treatment options.
2. Objective Monitoring of Treatment Progress
Tracking Treatment Response: Biomarkers provide objective data on how well an individual responds to a treatment plan. For instance, changes in dopamine levels, cortisol, or brain function can serve as indicators of improvement, helping clinicians adjust treatments as needed.
Predicting Relapse: Biomarkers such as neuroimaging results, cortisol levels, and inflammatory markers can help identify patients at higher risk of relapse. Early identification allows for timely intervention, such as providing additional support or modifying treatment strategies to prevent relapse.
3. Early Detection of Relapse
Early Intervention: Biomarkers can detect subtle physiological changes before behavioral signs of relapse become evident. For example, a drop in heart rate variability or shifts in neurochemistry might indicate a heightened risk of relapse, allowing for intervention before the individual returns to substance use.
4. Greater Precision in Diagnosis
Improving Accuracy: Biomarkers can help diagnose addiction types and severities more accurately by analyzing neurochemical or genetic profiles. This is especially useful in complex cases involving multiple substances or co-occurring mental health conditions.
Standardization of Diagnosis: Using biological markers provides consistency in diagnosing addiction, reducing the variability of subjective assessments. This standardization can improve the comparison of treatment outcomes across different patients and settings.
5. Mechanistic Understanding of Addiction
Identifying Underlying Biological Pathways: Biomarkers shed light on the biological processes driving addiction, such as alterations in dopamine signaling or brain inflammation. This deeper understanding can help clinicians and researchers develop new, more effective treatments.
Improved Research and Development: Identifying biomarkers opens the door for more targeted research, leading to the development of innovative treatment strategies, including new medications or behavioral therapies.
6. Predictive Power
Risk Stratification: Biomarkers can identify individuals who are biologically predisposed to addiction or relapse. This enables clinicians to intervene early with more aggressive preventive measures for those at higher risk, such as people with reduced dopamine sensitivity.
Long-term Outcome Prediction: Biomarkers can help predict the likelihood of long-term recovery. For example, improvements in brain connectivity or reductions in inflammatory markers may indicate a higher probability of sustained sobriety after treatment.
7. Cost-Effectiveness in the Long Run
Reduced Costs from Trial-and-Error: By using biomarkers to match individuals with the best possible treatment, healthcare providers can avoid the time, effort, and costs associated with ineffective therapies. This leads to cost savings for both patients and the healthcare system.
Preventing Relapse-Related Costs: Early detection of relapse risk through biomarkers can reduce the financial burden associated with relapse, such as costs for hospitalizations, additional treatments, or continued healthcare needs due to substance use.
8. Improved Patient Engagement
Motivating Patients: Seeing objective, measurable improvements in their biological markers, such as brain function or neurochemical balance, can encourage patients to stay engaged with treatment. Objective progress reports can be more compelling than subjective assessments alone.
Reducing Stigma: Biomarkers help frame addiction as a medical condition with biological underpinnings, reducing the stigma often associated with addiction. This understanding may encourage more people to seek treatment without fear of judgment.
The use of biomarkers in addiction treatment offers numerous advantages, including personalizing care, objectively monitoring progress, detecting relapse early, and improving overall treatment outcomes. As research continues, biomarkers will play an increasingly critical role in shaping the future of addiction therapy, leading to more effective, tailored, and cost-efficient care.
The Limitations of Biomarkers in Addiction Treatment: Challenges and Considerations
While biomarkers hold great promise for enhancing addiction treatment by providing objective, measurable indicators of biological responses to substances and therapies, they also come with significant challenges. These limitations must be considered, from technical and ethical concerns to practical and financial barriers. Here are the key disadvantages of using biomarkers in addiction treatment:
1. Complexity and Interpretation Challenges
Variability in Biomarkers: Biological markers can differ significantly between individuals due to factors like genetics, environment, and lifestyle. This variability complicates the application of biomarkers across different populations, limiting their reliability and predictive power.
Complex Interpretation: Biomarkers often don’t provide straightforward results. For instance, changes in brain scans or cortisol levels don’t always directly correlate with addiction severity or recovery. Specialized training is needed to interpret these results, making it harder to implement biomarkers broadly.
2. Limited Availability of Validated Biomarkers
Lack of Standardization: Few biomarkers have undergone rigorous validation for clinical use in addiction treatment. This lack of standardization makes it difficult to rely on biomarkers as a primary tool for guiding treatment decisions.
Narrow Scope: Most existing biomarkers focus on specific substances, like alcohol or opioids, limiting their applicability across different types of addictions. This is particularly true for behavioral addictions, such as gambling or internet addiction, where biomarkers are mainly undeveloped.
3. High Costs and Accessibility Issues
Expensive Testing: The technologies required to measure biomarkers—such as genetic tests, neuroimaging, or advanced blood analyses—can be costly. Many addiction treatment settings, especially those in low-resource areas, may not be able to afford these tools.
Limited Access to Technology: High-tech tools like functional MRI or PET scans are often available only in specialized research centers, restricting their use in routine addiction treatment. This lack of access creates disparities in care.
4. Ethical and Privacy Concerns
Genetic Privacy: Genetic biomarkers raise concerns about the sensitivity of genetic data storage, sharing, and use. Patients may worry about the potential for discrimination by insurers or employers if their genetic predisposition to addiction becomes known.
Stigmatization and Labeling: Identifying individuals as genetically predisposed to addiction can unintentionally stigmatize or label them, even if they have never developed a substance use disorder. This can add psychological and social burdens.
5. Over-reliance on Biological Data
Neglect of Psychosocial Factors: While biomarkers offer valuable biological insights, addiction is a complex disorder influenced by psychological, social, and environmental factors. Overemphasizing biological data risks underplaying these crucial dimensions critical for comprehensive care.
Risk of Oversimplification: Biomarkers might oversimplify the complexity of addiction, reducing it to biological changes while ignoring other factors like behavior, emotion, and environment, which are equally crucial in treatment.
6. Potential for Misuse or Misinterpretation
False Positives or Negatives: Biomarkers are not foolproof and can yield inaccurate results. For instance, neuroimaging may show brain abnormalities in someone who doesn’t have an addiction or fail to detect relevant changes in someone who does. This can lead to incorrect treatment decisions.
Biomarker “Lock-in”: Once a biomarker is widely accepted, it is risky to become overly dependent on it, even as newer methods emerge. This could hinder innovation and keep the field locked into outdated or limited approaches.
7. Invasive or Uncomfortable Procedures
Invasive Testing: Some biomarkers require invasive methods, such as blood draws or cerebrospinal fluid collection. These procedures can be uncomfortable or distressing for patients, possibly reducing their willingness to undergo regular testing.
Patient Discomfort with Neuroimaging: Techniques like MRI or PET scans can be intimidating or uncomfortable. Repeated scanning to monitor progress might be burdensome, reducing compliance over time.
8. Limited Utility for Behavioral Addictions
Narrow Focus on Substance Use Disorders: Most biomarker research has focused on substance use disorders like alcohol or opioid addiction. Behavioral addictions, such as gambling or internet addiction, remain largely unexplored, limiting the applicability of biomarkers across the full spectrum of addiction.
9. Potential for Delayed or Inaccurate Diagnosis
Latency in Biomarker Changes: Biological markers often lag behind behavioral changes. Structural changes in the brain or shifts in genetic expression may take time to manifest, potentially delaying adjustments to treatment plans.
Inconsistent Response to Treatment: Improving a biomarker does not always translate to changes in behavior or cravings. Focusing solely on biological recovery risks missing critical aspects of the patient’s treatment progress.
While biomarkers offer valuable insights and the potential for personalized addiction treatment, their complexity, cost, ethical implications, and limited scope present significant challenges. To ensure adequate care, biomarkers should be used alongside a comprehensive approach that considers psychological, social, and environmental factors in addiction treatment.
The Ethical Dilemmas of Biomarkers in Addiction Treatment: Balancing Privacy, Fairness, and Autonomy
The introduction of biological markers (biomarkers) into addiction treatment holds great promise for personalized care, but it also raises a host of ethical concerns. These dilemmas revolve around privacy, fairness, stigmatization, and the broader implications of relying on biological data. Below are some of the key ethical issues associated with biomarkers in addiction treatment:
1. Privacy and Confidentiality
Genetic Privacy: Biomarkers often involve genetic testing, which creates significant privacy concerns. The fear of misuse by insurance companies, employers, or law enforcement is real, with individuals facing potential discrimination if their genetic predisposition to addiction becomes public.
Data Security: Safeguarding sensitive biological data—such as neuroimaging results or genetic markers—is critical. Data security breaches could lead to unauthorized access, resulting in the misuse of personal information and compromising an individual’s privacy.
2. Stigmatization and Labeling
Genetic Determinism: When individuals are identified as having a genetic predisposition to addiction, they may face stigmatization or labeling. This can lead to a deterministic view of their future, making them or society feel that addiction is unavoidable, thereby reinforcing negative stereotypes.
Social and Psychological Impact: Learning that one is biologically predisposed to addiction may cause psychological distress, increase stigma, or lead to changes in self-perception. Individuals could feel a loss of control over their lives, even if they do not engage in substance use.
3. Discrimination and Fairness
Insurance Discrimination: If insurers gain access to biomarker data, individuals might face higher premiums or even denial of coverage based on their biological risk for addiction. This creates a significant ethical dilemma in protecting people from discrimination based on their genetic makeup.
Employment Discrimination: Employers may seek access to biomarker information, especially for jobs requiring high cognitive or emotional functioning. Individuals could be unjustly denied job opportunities if they are flagged as being at risk for addiction, even if they have no history of substance use.
4. Informed Consent and Autonomy
Complexity of Information: Biomarkers and their implications can be difficult for patients to understand fully. This makes obtaining accurate informed consent challenging, as patients may not completely grasp the consequences of having specific biomarkers or how their data will be used.
Pressure to Consent: Individuals undergoing addiction treatment might feel pressured to consent to biomarker testing, even if they are uncomfortable with it. This pressure undermines their autonomy, which is essential for making informed decisions about their health and treatment.
5. Equity and Access
Unequal Access to Biomarker Testing: Biomarker-based treatments are often expensive, limiting access for individuals in low-income settings. This could exacerbate healthcare inequalities, with wealthier individuals gaining access to more personalized therapies while others are left with less effective options.
Resource Allocation: As resources are directed toward biomarker testing, funding for other essential treatment options such as counseling, peer support, or harm-reduction programs may be reduced. This raises ethical questions about how to distribute healthcare resources fairly and equitably.
6. Genetic Modification or Intervention
Ethical Limits of Genetic Intervention: Identifying genetic markers for addiction raises questions about whether society should intervene to modify these genes. Genetic modification brings up ethical concerns about eugenics and whether we should alter the genetic makeup of future generations.
Long-term Implications: Using biomarkers to predict addiction risk could lead to early intervention in individuals who may never develop the condition. This medicalization of people based on risk alone could lead to psychological and social consequences, making early intervention a double-edged sword.
7. Reductionism and Oversimplification
Biological Determinism: Focusing too heavily on biomarkers risks reducing addiction to a purely biological phenomenon. This narrow view could downplay the importance of environmental, psychological, and social factors in both the development and treatment of addiction, leading to less holistic care.
Neglect of Psychosocial Factors: Over-reliance on biomarkers may shift the focus away from critical psychosocial interventions, such as cognitive-behavioral therapy, social support, or addressing social determinants of addiction like poverty and trauma.
8. False Positives and Negatives
Risk of Misdiagnosis: Biomarkers are not always accurate, and false positives or negatives can occur. A false positive could lead to unnecessary medicalization of someone who is not at risk, while a false negative might prevent someone from receiving the help they need.
Impact on Treatment Pathways: If a patient receives an inaccurate biomarker result, it could lead to inappropriate treatment choices or missed opportunities for intervention. Misdiagnosis based on biomarkers could have severe consequences for patient outcomes.
9. Impact on Vulnerable Populations
Exacerbating Inequities: Vulnerable populations, including minorities and those with mental health issues, may face a greater risk of being labeled “high risk” based on biomarkers. This could reinforce existing inequalities and further marginalize these groups.
Increased Surveillance: Using biomarkers may lead to heightened monitoring of vulnerable groups, potentially resulting in greater involvement with the criminal justice system. Individuals identified as “at risk” could face increased scrutiny or mandatory treatments, even if they have not engaged in substance use.
Biomarkers offer exciting possibilities for personalized addiction treatment, but their use comes with significant ethical challenges. Privacy, discrimination, fairness, and reducing complex human behaviors to biological data must be addressed carefully. By establishing clear regulations, robust data protection, and a commitment to holistic care, the ethical concerns surrounding biomarkers can be managed while ensuring that biomarkers enhance treatment without infringing on individual rights.
Strategies for Integrating Biological Markers into Community-Based Addiction Treatment: Enhancing Access, Education, and Equity
Biological markers (biomarkers) offer significant potential in personalizing addiction treatment, but their integration into community settings requires thoughtful strategies to ensure accessibility, ethical use, and equitable care. Communities, particularly those serving vulnerable populations, must improve education, foster collaboration, and maintain ethical standards. Here are key strategies for successfully integrating biomarkers into addiction treatment:
1. Public Education and Awareness Campaigns
Raising Awareness: Community organizations should work with healthcare providers to educate the public about how biomarkers can improve addiction treatment. By framing addiction as a medical condition, they can help reduce stigma and foster a better understanding of the role biomarkers play in personalized care.
Addressing Misinformation: Clear, evidence-based communication is crucial. Public forums, social media, and educational materials can help the public understand the benefits and limitations of this emerging technology by dispelling myths and managing expectations around biomarkers.
2. Training for Healthcare and Social Service Providers
Professional Development: Local clinics should offer healthcare providers and addiction counselors training in interpreting biomarker data and incorporating it into treatment plans. This will ensure that biomarker-based interventions are applied effectively within community addiction programs.
Ethical and Cultural Competency: Training should emphasize ethical standards, including privacy, informed consent, and cultural sensitivity. This is particularly important in diverse communities, where there may be heightened concerns about the use of personal health information.
3. Collaboration Between Healthcare Providers and Community Organizations
Integrated Care Models: Collaboration between healthcare providers and community organizations can ensure that biomarker data is part of a holistic treatment approach. Combining biomarker-based insights with traditional psychosocial interventions will help provide more comprehensive care.
Referral Networks: Establishing strong referral networks between medical facilities that offer biomarker testing and local addiction programs can bridge the gap between diagnosis and treatment, ensuring patients receive the care they need based on biomarker data.
4. Access and Equity Initiatives
Subsidized Biomarker Testing: To address the high costs associated with biomarker testing, communities should explore partnerships with hospitals, nonprofits, and public health departments to subsidize or offer low-cost testing options, particularly for underserved populations.
Mobile Health Units: Deploying mobile clinics to provide biomarker testing in rural or underserved areas can significantly improve access to advanced diagnostics, helping ensure that everyone can benefit from personalized addiction care.
5. Ethical and Legal Safeguards
Data Privacy Protections: Communities must advocate for strict data privacy protocols to protect individuals undergoing biomarker testing. This includes ensuring that third parties, such as employers or insurance companies, do not misuse personal health data.
Advocacy for Anti-Discrimination Policies: Community groups should collaborate with legal aid organizations to promote policies that prevent discrimination based on genetic or biomarker data, safeguarding individuals’ rights and protections.
6. Support for Vulnerable Populations
Tailored Outreach for At-Risk Groups: Special attention should be given to reaching vulnerable populations disproportionately affected by addiction, such as racial minorities or individuals experiencing homelessness. Tailored outreach ensures these groups can access biomarker-based treatments.
Culturally Competent Care: Culturally sensitive approaches should be integrated into biomarker-based treatments. Different communities may have varying views on addiction and genetic testing, so it’s crucial to align care and education with these cultural perspectives.
7. Patient Empowerment and Support Groups
Patient Education Programs: Empowering patients with knowledge about biomarkers, what the testing entails, and how it can impact their treatment outcomes enables them to participate in their recovery and make informed decisions actively.
Peer Support Networks: Peer-led support groups can help patients process their biomarker data in the context of their broader addiction recovery. Discussions around how biomarkers influence treatment plans can foster a sense of shared experience and understanding.
8. Public-Private Partnerships
Collaboration with Research Institutions: Community health centers can partner with research universities to ensure the latest biomarker innovations are applied in local settings. Including diverse populations in research studies also helps ensure that biomarker technologies are relevant and accessible to all.
Engagement with the Private Sector: Collaborations with biotechnology and pharmaceutical companies can help bring cost-effective biomarker testing to community clinics, increasing access to cutting-edge diagnostic tools.
9. Evaluation and Feedback Mechanisms
Continuous Monitoring and Evaluation: Community organizations should establish systems to monitor the outcomes of biomarker-based treatments and collect patient feedback. Regular evaluations ensure that biomarker integration leads to improved addiction care.
Community Input in Policy Development: Involving local communities in policy-making ensures that their needs, values, and concerns are reflected in how biomarkers are used and regulated.
10. Holistic Approaches to Treatment
Combining Biomarker-Based and Traditional Therapies: Biomarkers should be viewed as one tool in a broader addiction treatment strategy. By combining biomarker data with traditional therapies—such as counseling, behavioral therapy, and social support services—communities can offer well-rounded care that addresses the biological, psychological, and social dimensions of addiction.
Holistic Health Programs: Integrating biomarker data into comprehensive wellness programs that include mental health counseling, physical wellness, and stress management ensures that individuals receive all-encompassing support throughout their recovery journey.
Community strategies for incorporating biomarkers into addiction treatment should focus on enhancing accessibility, fostering education, and ensuring ethical practices. Through collaboration, privacy protections, and equitable access, communities can leverage biomarkers to improve treatment outcomes while maintaining a holistic and culturally sensitive approach. This will ensure personalized care is available to all, particularly vulnerable and underserved populations.
Frequently Asked Questions
Here are some common questions:
How are biomarkers different from self-reported substance use?
Self-report relies on patient recall and honesty, while biomarkers provide objective data. Both are important, but biomarkers can validate usage patterns and detect changes that may not yet be clinically noticeable.
Can biomarkers predict relapse?
Some biomarkers may indicate increased relapse risk, such as elevated stress hormones, altered brain activity, or physiological signs of craving. However, no biomarker can predict relapse with certainty.
Do biomarkers replace clinical assessment?
No. Biomarkers are tools that complement clinical interviews, behavioral assessments, and patient-reported outcomes. Addiction treatment still requires clinical judgment and individualized care.
Conclusion
Biological markers hold significant promise for advancing addiction treatment by enabling more personalized and precise interventions. Their advantages include improved diagnosis, tailored care, and better tracking of recovery progress. However, challenges such as high costs, complex data interpretation, and potential over-reliance on biological factors must be addressed. Ethical dilemmas, particularly privacy, discrimination, and stigmatization, further complicate their use. Community resource strategies focused on education, ethical safeguards, and equitable access must ensure these biomarkers are used responsibly. By balancing the benefits against the challenges, biomarkers can contribute to more effective and comprehensive addiction treatment.
Video: The Addiction Marker Doctors Wish You Knew About #health #treatment #awareness