The biofeedback patch is an innovative tool in addiction therapy that uses wearable technology to monitor physiological signals like heart rate and skin response to detect early signs of stress and cravings. Providing real-time feedback helps individuals apply coping strategies before relapse risk increases, strengthening self-awareness and emotional regulation. While the patch offers non-invasive and measurable support, challenges such as cost, data privacy, and over-reliance on technology raise ethical concerns. Effective use depends on mindful self-management, clinical guidance, and family and community support to ensure technology enhances—rather than replaces—personal recovery skills.
Biofeedback Therapy and the Biofeedback Patch in Addiction Treatment
What It Is
- A “biofeedback patch” is a wearable sensor device (often worn on the chest, wrist, or skin surface) that monitors physiological indicators such as heart rate variability (HRV), breathing rate, muscle tension, or skin conductance.
- In the context of addiction therapy, the patch is used as part of a stress-/craving-management tool: it detects physiological signs of stress or craving (e.g., low HRV) and then prompts the user to use a coping strategy (e.g., a breathing exercise) via a connected app or device.
- For instance, one study found that participants wearing a smart HRV‐biofeedback patch plus an app had 64% fewer days of substance use compared with a control group, during the first year of recovery.
How It Works
- The patch continuously measures heart rate variability or other stress‐related physiological signs, or measures them at set times.
- When the patch/app detects signs of stress, arousal, or a craving state, it sends a prompt (vibration, alert, or app message) to the user to engage in a coping exercise.
- The user completes the exercise (e.g., controlled breathing, mindfulness, grounding) and, via the patch/app, receives feedback on their physiological state improvement (e.g., higher HRV, calmer state). Over time, the user learns to self-regulate these physiological triggers.
- The device is used as an adjunctive tool—not a replacement—for standard addiction treatment (therapy, support groups, possibly medication).
Why It May Be Valuable in Addiction Recovery
- Many people in early recovery struggle with low self-awareness of emotional/physiological states that precede relapse (stress → craving → use). The patch helps bring visibility to those precursors.
- By monitoring physiological stress indicators, the patch helps intervene before substance use occurs—effectively giving a “heads-up” when the user is entering a risky state.
- It offers a non-medication, technology-supported pathway to enhance emotional regulation, reduce craving intensity, and support relapse prevention.
Considerations and Cautions
- As with many emerging tools, long-term evidence is still developing. The patch works best when integrated into a broader recovery plan.
- Access and cost may be barriers depending on device cost, app subscriptions, and whether insurance covers such tools.
- Users must still engage in broader behavioral, psychological, and social interventions to support sustainable recovery—wearable patches alone are not sufficient.
Disadvantages of Biofeedback Patches in Addiction Therapy
Biofeedback patches—such as wearable heart-rate variability (HRV) or stress-monitoring devices—offer promising support for managing cravings and emotional regulation in addiction recovery. However, like all emerging treatment tools, they come with important limitations. Understanding these disadvantages helps individuals, families, and clinicians make informed decisions about whether this technology is appropriate for a recovery plan.
1. Cost and Accessibility
High-quality biofeedback patches and their connected apps can be expensive. Many clinics and individuals cannot afford the devices, and insurance coverage is often limited or nonexistent because the technology may be classified as experimental. When access is restricted to higher-resource programs, treatment inequities can grow—leaving underserved populations without the same opportunities for technological support.
2. Variable Effectiveness and Individual Response
Not everyone responds to biofeedback in the same way. Some individuals experience meaningful improvements in stress regulation and craving control, while others notice little change. Addiction is influenced by biological, psychological, social, and environmental factors—meaning a wearable patch cannot address all relapse risks. Additionally, long-term research on sustained outcomes is still developing, so lasting effectiveness remains under study.
3. Risk of Over-Reliance or False Security
There is a danger that users may place too much trust in the device, believing the patch will “manage” cravings for them. This can reduce motivation to build internal coping skills, attend therapy, or engage in peer support. If real-world emotional or social triggers arise that are not detected physiologically, individuals may underestimate relapse risk.
4. Technical Limitations and Usability Issues
Wearable devices depend on accurate detection and interpretation of physiological signals. False alerts or missed stress responses can reduce trust in the technology. Some users struggle with syncing apps, charging devices, correctly placing sensors, or understanding feedback prompts. Certain medical conditions, such as cardiac irregularities or skin sensitivities, may also interfere with accurate readings.
5. Privacy and Data Security Concerns
Biofeedback patches collect sensitive physiological and behavioral data. Without strong data protection practices, there is a risk of unauthorized access or misuse of personal health information. Users must be clearly informed about who owns the data, who can view it, how long it is stored, and whether it may be used for research or commercial purposes.
6. Not a Standalone Solution
Experts emphasize that biofeedback patches are designed to support—not replace—comprehensive addiction treatment. Therapy, peer support, behavioral interventions, and medication-assisted treatment (when appropriate) remain essential. If the patch is used alone, it cannot adequately address the cognitive, emotional, and social dimensions of addiction.
7. Ethical and Equity Issues
Limited access to advanced wearable technologies may create unequal opportunities for treatment. There is also the risk of technology hype driving adoption before sufficient clinical evidence is available. Ethical care requires ensuring that patient benefit—not novelty or marketing—guides treatment decisions.
Summary
Biofeedback patches can be valuable tools for strengthening self-regulation and detecting early physiological signs of stress and cravings. However, they also present meaningful disadvantages, including cost barriers, variable effectiveness, over-reliance risks, technical challenges, privacy concerns, and ethical equity issues. When used thoughtfully and combined with holistic addiction treatment, biofeedback technology can enhance recovery—but it should never replace human connection, therapy, and comprehensive care.
Ethical Dilemmas of Using Biofeedback Patches in Addiction Therapy
Biofeedback patches and other wearable physiological monitoring devices are becoming innovative tools in addiction treatment. By tracking heart-rate variability, stress responses, and other bodily signals, these devices help individuals recognize early warning signs of cravings and emotional distress. While promising, this technology also introduces important ethical dilemmas that clinicians, clients, and treatment programs must carefully consider. Responsible use requires balancing technological innovation with patient rights, dignity, and evidence-based care.
Informed Consent and Autonomy
Biofeedback patches continuously collect personal physiological data and often deliver prompts for coping exercises. This raises a critical ethical question: Does the individual fully understand what the device does, how the data are used, and the risks? Because people in early recovery may be emotionally vulnerable, ensuring voluntary and informed consent is essential. Ethical practice requires that clients clearly understand the device’s purpose, limitations, and optional nature, with full freedom to accept or decline its use without pressure.
Privacy, Confidentiality, and Data Security
Wearable biofeedback devices gather sensitive behavioral and physiological information that may reveal stress patterns, craving states, or relapse risk. If third-party technology companies store or manage this data, concerns arise about ownership, security, and potential misuse. Without strict protections, personal health data could be accessed improperly or used for marketing or profiling. Ethical care demands transparent data policies, encryption, confidentiality safeguards, and clear communication about who can view and store collected information.
Equity, Access, and Justice
Biofeedback patches can be costly, requiring device purchases, subscriptions, or specialized clinical supervision. This may limit access to individuals in well-funded programs or urban centers, leaving low-resource communities behind. The ethical dilemma lies in whether emerging technologies create “premium” treatment options only for those who can afford them. The principle of justice calls for fair access to effective care and attention to preventing widening treatment disparities.
Technology Reliance vs. Therapeutic Relationship
There is a risk that clients may view the patch as the primary solution to recovery challenges, reducing engagement in therapy, peer support, or personal skill-building. Likewise, programs may overemphasize device-based feedback at the expense of human connection. Ethical practice requires recognizing technology as an adjunct to treatment—not a replacement for the therapeutic alliance, community support, and personal growth central to recovery.
Evidence, Effectiveness, and Marketing Ethics
Many biofeedback devices are still emerging in addiction treatment research. Long-term outcomes, standardized protocols, and clear indications for use remain under study. If devices are marketed with exaggerated claims or without transparent discussion of limitations, clients may develop unrealistic expectations. Ethical responsibility requires that clinicians and programs rely on evidence-based practice, honest communication, and scientific integrity rather than technology hype.
Autonomy vs. Surveillance and Control
Because biofeedback patches monitor the body continuously and issue behavioral prompts, some individuals may feel watched or controlled. What begins as supportive guidance may feel like surveillance, potentially undermining personal agency. Ethical care must ensure that monitoring enhances self-awareness rather than replacing internal decision-making or creating dependence on external control.
Summary
Biofeedback patches offer exciting possibilities for identifying physiological stress patterns, strengthening emotional regulation, and supporting relapse prevention. Yet they raise ethical dilemmas involving informed consent, privacy, equitable access, evidence standards, therapeutic balance, and autonomy. When integrated thoughtfully and transparently, alongside human-centered care, biofeedback technology can enhance addiction recovery. When used without ethical safeguards, it risks undermining trust, fairness, and self-empowerment.
Self-Management Strategies for Deciding if a Biofeedback Patch Is Right for Addiction Recovery
Biofeedback patches are wearable devices that track physiological signals, such as heart rate variability, breathing patterns, and stress responses. In addiction therapy, they can help individuals recognize early warning signs of cravings and emotional distress. However, this technology is not a one-size-fits-all solution. Effective use begins with self-management — the ability to reflect, evaluate, and decide whether a biofeedback patch truly supports personal recovery goals.
Evaluate Your Recovery Stage and Readiness
Before committing to a biofeedback patch, it is important to assess emotional stability and recovery. These devices work best when a person has completed detox and reached a level of psychological grounding. Individuals should reflect on what drives their cravings — physical stress, emotional overload, or social triggers — since biofeedback is most effective for regulating physiological stress. Discussing readiness with a therapist ensures the timing is appropriate and supportive rather than overwhelming.
Goal: Align biofeedback use with current recovery needs and emotional capacity.
Research Device Credibility and Evidence
Not all biofeedback patches are clinically validated. Some are medical-grade devices supported by research, while others are general wellness products with limited evidence. Reviewing FDA clearance, clinical studies, or professional endorsements helps distinguish credible tools from exaggerated marketing claims. Consulting healthcare providers before choosing a device protects against investing in ineffective or unreliable technology.
Goal: Select a device grounded in science and transparent data practices.
Clarify Treatment Goals and Integration
Biofeedback works best when paired with clear recovery objectives. Individuals benefit from identifying specific goals such as reducing craving intensity, improving sleep, or strengthening stress regulation. Discussing how the patch integrates with Cognitive Behavioral Therapy, medication-assisted treatment, mindfulness practice, or counseling ensures the device enhances — rather than replaces — existing therapy.
Goal: Treat the patch as one supportive element in a complete recovery plan.
Practice Emotional Regulation Skills
A biofeedback patch provides alerts, but personal coping skills create change. Learning breathing techniques, grounding exercises, and relaxation strategies ensures individuals can respond effectively when stress signals arise. Journaling emotional reactions alongside physiological feedback builds insight into trigger patterns and progress over time.
Goal: Strengthen internal coping skills rather than relying solely on the device.
Build a Support System
Recovery is not meant to happen alone. Sharing experiences with therapists, sponsors, family members, or recovery peers creates accountability and perspective. Trusted supporters can help interpret progress, reduce frustration with technology, and reinforce that the patch is a tool — not a cure.
Goal: Combine technology with human connection and encouragement.
Monitor Progress and Adjust
Self-management means regularly evaluating whether the device is helping. After several weeks, individuals should review changes in stress awareness, craving control, and emotional stability. If the patch causes discomfort, anxiety, or distraction, discussing adjustments or discontinuation with a clinician ensures treatment remains beneficial.
Goal: Maintain flexibility and prevent over-dependence on technology.
Understand Data Privacy and Consent
Because biofeedback patches collect sensitive physiological data, individuals must understand who owns the information, how it is stored, and who can access it. Reading consent forms carefully, opting out of unnecessary data sharing, and confirming that systems are HIPAA-compliant protect privacy and personal autonomy.
Goal: Safeguard trust and control over personal health information.
Summary
Deciding whether a biofeedback patch belongs in addiction treatment requires self-reflection, informed research, emotional readiness, and professional guidance. When used thoughtfully, biofeedback technology can strengthen self-awareness and stress regulation. But lasting recovery still depends on therapy, community, and personal growth. The best outcomes occur when technology supports — not substitutes — the human work of healing.
Family Support Strategies for Deciding if a Biofeedback Patch Is Right for Addiction Recovery
Biofeedback patches are wearable devices that monitor physiological signals, such as heart rate variability, breathing patterns, and stress responses. In addiction therapy, they help individuals recognize early signs of emotional distress and cravings. While this technology can be a powerful recovery aid, deciding whether it is the best and safest option should never rest solely on the individual. Family support plays a vital role in ensuring decisions are informed, ethical, and emotionally safe.
Start with Family Education and Shared Understanding
Before agreeing to use a biofeedback patch, families should learn how the technology works, what data it collects, and how it supports emotional regulation. Attending informational sessions with treatment providers, reviewing reputable research together, and openly discussing data privacy policies help separate evidence-based practice from marketing claims.
Goal: Build a shared and factual understanding before committing to the technology.
Encourage Open, Non-Judgmental Communication
Conversations about biofeedback should be rooted in empathy and curiosity rather than pressure or doubt. Asking reflective questions about expectations, concerns, and comfort with body-monitoring technology fosters trust. Families should emphasize that the final decision belongs to the loved one in recovery.
Goal: Maintain trust and respect personal autonomy.
Assess Emotional Readiness Together
Because biofeedback increases self-awareness of physiological stress, it can sometimes feel intense or frustrating. Families are often the first to notice whether a loved one feels stable, confident, and emotionally prepared for technology-assisted therapy. Practicing grounding or relaxation techniques together before beginning use can strengthen readiness.
Goal: Ensure emotional safety and confidence before starting.
Integrate Family Support into the Treatment Plan
Biofeedback works best when paired with therapy and social support. Families can coordinate with clinicians to understand how the patch fits into the recovery plan, schedule regular check-ins to discuss progress, and reinforce healthy coping strategies learned through feedback.
Goal: Connect technology-based insights to real-world relationship support.
Discuss Ethical and Privacy Boundaries
Because biofeedback patches collect sensitive health data, families should understand who can access the information and how it is protected. Loved ones must retain control over their data, and family members should respect privacy unless information is voluntarily shared.
Goal: Uphold trust, transparency, and ethical boundaries.
Promote Encouragement and Balanced Expectations
Families can help frame the biofeedback patch as a learning tool rather than a cure. Celebrating emotional growth, stress-management improvements, and consistent effort prevents over-focus on numerical data or device metrics.
Goal: Support progress without creating pressure or dependence.
Collaborate with Professional and Community Resources
Consulting addiction counselors, recovery coaches, peer-support groups, or family therapists helps families make evidence-informed decisions. Community feedback can also reveal whether biofeedback options are clinically recommended, affordable, or appropriate for specific recovery needs.
Goal: Ensure decisions are supported by professional and community guidance.
Summary
Family involvement is key in determining whether a biofeedback patch is appropriate for addiction recovery. Through education, empathy, ethical awareness, and collaboration, families help ensure that technology is introduced safely and effectively. The strongest support balances encouragement with respect for autonomy—so the biofeedback patch becomes a bridge toward healing rather than a substitute for human connection.
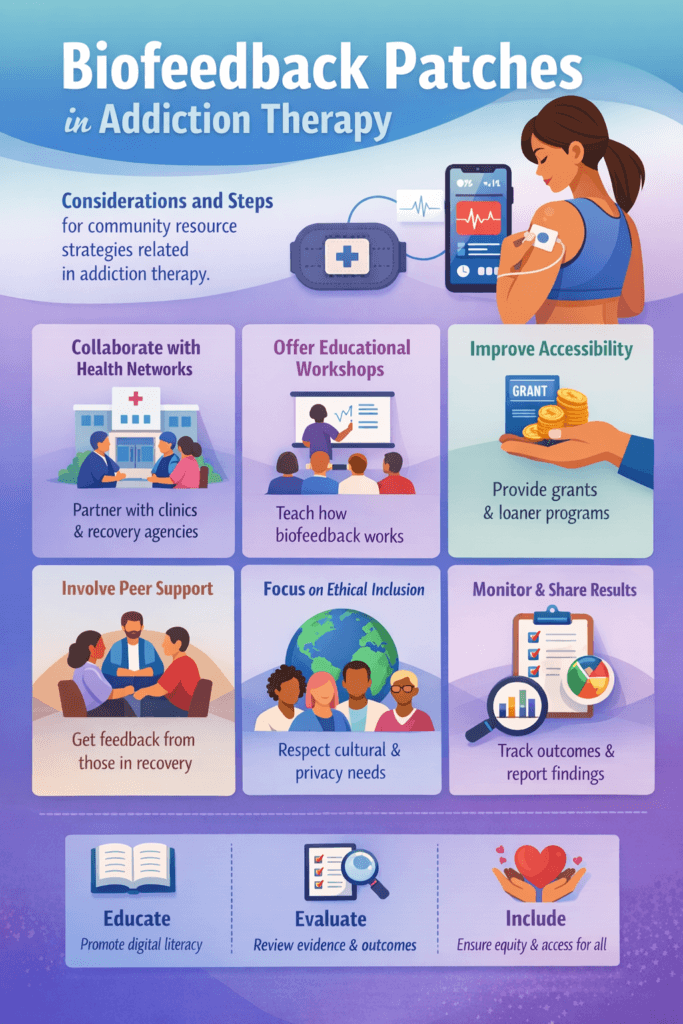
Community Resource Strategies for Evaluating Biofeedback Patches in Addiction Treatment
Biofeedback patches and other wearable stress-monitoring devices are emerging tools in addiction therapy, helping individuals recognize physiological signs of stress and craving before relapse occurs. However, deciding whether these devices are appropriate and effective cannot rest solely on individuals or clinics. Communities play a vital role in evaluating new recovery technologies to ensure they are ethical, evidence-based, accessible, and inclusive. Strong community resource strategies help guide responsible adoption and protect against unequal or premature implementation.
Collaborate with Local Health Networks and Recovery Agencies
Community health centers, behavioral health agencies, and recovery organizations are often the first point of contact for individuals seeking treatment. These institutions can help assess whether biofeedback technology aligns with clinical standards and individual recovery needs. Encouraging clinical screening before device use ensures the patch is introduced at the appropriate recovery stage and for the intended therapeutic purpose. Community oversight committees can also review wearable technologies for ethical practice, privacy safeguards, and accessibility before local rollout.
Goal: Establish clinical and ethical guidance before recommending biofeedback as a community-supported tool.
Offer Education and Technology Awareness Programs
Many individuals and families are unfamiliar with biofeedback technology or uncertain about its limitations. Public workshops, demonstrations, and Q&A sessions led by clinicians help explain how biofeedback works and what realistic outcomes look like. Partnerships with universities, libraries, or wellness centers can improve digital health literacy and reduce stigma around technology-based therapy.
Goal: Ensure community members make informed and confident treatment decisions.
Improve Accessibility and Funding Opportunities
Cost remains one of the largest barriers to wearable recovery technology. Communities can collaborate with nonprofits, public health departments, and recovery foundations to secure grants, pilot programs, or device loan initiatives. Clinics can share equipment across programs, and community leaders can advocate for insurance coverage or sliding-scale pricing models.
Goal: Promote fair access regardless of income or location.
Encourage Peer-Led and Lived Experience Input
People in recovery offer essential insight into whether a biofeedback patch feels supportive or intrusive in real-world use. Peer recovery specialists and focus groups can test devices, provide usability feedback, and share experiences at recovery meetings. This ensures recommendations are shaped by lived experience rather than theory alone.
Goal: Ground community decisions in real recovery perspectives.
Create Cross-Disciplinary Partnerships
Effective oversight of wearable health technology requires collaboration between healthcare professionals, technology experts, and ethical advisors. Public health officials, addiction specialists, cybersecurity professionals, and research institutions can work together to establish guidelines for safe data handling, ethical monitoring, and evidence-based use of biofeedback devices.
Goal: Balance innovation with safety, accountability, and ethical responsibility.
Address Cultural and Ethical Inclusion
Community planning must ensure biofeedback programs respect cultural values, trauma sensitivity, and privacy expectations. Engaging faith-based organizations, cultural councils, and disability advocates helps ensure materials are inclusive, accessible, and respectful. Translated resources and culturally adapted guidance further promote equity in recovery support.
Goal: Provide technology that respects diverse community needs.
Monitor Outcomes and Share Transparent Data
Communities should track real-world outcomes of biofeedback use, including improvements in stress regulation, reduced craving, and increased engagement in treatment. Anonymous feedback systems and partnerships with universities for outcome studies help determine whether the technology truly benefits recovery. Sharing results through community networks maintains transparency and guides future policy decisions.
Goal: Use data-driven evaluation for continuous improvement.
Summary
Community resource strategies ensure that biofeedback patches in addiction therapy are introduced thoughtfully, ethically, and equitably. Through collaboration, education, funding support, peer involvement, cultural inclusion, and outcome monitoring, communities can determine whether wearable biofeedback technology enhances recovery safely and effectively. When guided by shared responsibility and compassion, technology becomes a supportive bridge to healing—not a barrier to trust or access.
Frequently Asked Questions
Here are some common questions:
1. What is a biofeedback patch?
A biofeedback patch is a wearable sensor placed on the skin (often on the chest or wrist) that monitors physiological signals, such as heart rate variability, breathing rate, muscle tension, or skin conductance. It provides real-time feedback to help users recognize stress and craving responses.
2. How does a biofeedback patch help in addiction recovery?
The patch detects early physiological signs of stress or emotional arousal that often precede cravings. When these signals appear, the connected app alerts the user to practice coping strategies like deep breathing or grounding, helping prevent relapse before it occurs.
3. Is a biofeedback patch a replacement for therapy?
No. Biofeedback patches are designed to support addiction treatment, not replace counseling, group therapy, or medication-assisted treatment. They work best as an additional self-regulation tool.
4. Who is a good candidate for using a biofeedback patch?
Individuals who have completed detox, have basic emotional stability, and are willing to use wearable technology often benefit most. A clinician should assess readiness before starting.
5. Can biofeedback patches reduce cravings?
They can help reduce the intensity of cravings by increasing awareness of stress responses and prompting early coping. However, results vary by individual, and patches work best alongside traditional therapy.
6. Are biofeedback patches safe to use?
Yes, they are non-invasive and generally safe. Some users may experience mild frustration or anxiety from frequent alerts, which can be managed with therapist guidance.
7. Do biofeedback patches collect personal data?
Yes. They collect physiological data such as heart rate or stress levels. Ethical programs use encrypted, HIPAA-compliant systems. Users should always understand who can access and store their data.
8. Are these patches covered by insurance?
Coverage varies. Some programs include biofeedback within therapy billing, while others require out-of-pocket payment. Many insurers still classify them as emerging or investigational tools.
9. Can someone become dependent on the patch?
There is a risk of over-reliance if users trust the device more than their own coping abilities. That’s why clinicians emphasize pairing the patch with skill-building therapy.
10. How long does someone need to use a biofeedback patch?
There is no universal standard. Some programs use patches for several weeks to months, depending on recovery goals and progress.
11. What if the patch doesn’t seem helpful?
Not everyone responds the same way. If the patch causes stress, frustration, or shows no benefit, users should discuss adjusting or discontinuing it with their clinician.
12. Does the patch work for all types of addiction?
Biofeedback has been studied most in substance-use disorders such as alcohol, opioids, and nicotine. Research is growing for behavioral addictions like gambling or gaming.
13. Can biofeedback be used at home?
Yes. Many patches are designed for home use with mobile apps, often combined with telehealth check-ins for clinician support.
14. Are there privacy risks?
As with any wearable health device, data privacy is an important concern. Users should review consent forms, understand data-sharing policies, and choose programs with strong security protections.
15. What is the main benefit of biofeedback in recovery?
The greatest benefit is turning invisible stress responses into visible feedback, helping individuals build self-awareness, emotional regulation, and early intervention skills for relapse prevention.
Conclusion
Biofeedback patches offer a promising bridge between technology and behavioral recovery, transforming the way addiction therapy supports self-regulation and relapse prevention. Yet their success depends on responsible implementation—guided by transparency, human connection, and ethical safeguards. Individuals must use biofeedback as a supplement, not a substitute, for holistic therapy; families should encourage emotional balance and informed decision-making; and communities must ensure equitable access, cultural inclusion, and accountability. When applied thoughtfully, biofeedback patches can enhance recovery outcomes—empowering individuals to translate data into awareness, and awareness into lasting change.
Video: