Benzodiazepine addiction can develop from prolonged use, especially when mixed with alcohol or opioids. While effective in the short term, they lead to tolerance, dependence, and withdrawal. Prevention involves proper use, non-drug treatments, and stress management. Family support and community resources, including education and mental health services, play a key role in safe management.
Understanding Benzodiazepine Dependency: Risks, Signs, and Treatment
Benzodiazepine dependency, also known as benzodiazepine use disorder, occurs when a person becomes physically or psychologically reliant on benzodiazepines. These medications, commonly prescribed for anxiety, insomnia, and muscle relaxation, include diazepam (Valium), lorazepam (Ativan), and alprazolam (Xanax). While effective for short-term relief, long-term use can lead to dependency and withdrawal challenges.
Mechanisms of Dependency
Benzodiazepines enhance the effects of gamma-aminobutyric acid (GABA), a neurotransmitter that reduces brain activity and promotes relaxation. Over time, the body adapts to its presence, leading to tolerance—meaning higher doses are required to achieve the same effects. This escalation can result in physical dependence, where the body requires the drug to function normally, and psychological dependence, where individuals believe they cannot cope without it.
Signs of Benzodiazepine Dependency
Recognizing dependency is crucial for early intervention. Common signs include:
- Tolerance: Needing increasing doses to achieve the same effect.
- Withdrawal Symptoms: Anxiety, insomnia, irritability, sweating, tremors, and, in severe cases, seizures when the drug is reduced or stopped.
- Continued Use Despite Consequences: Taking benzodiazepines longer than prescribed or for non-medical reasons.
- Difficulty Stopping: Experiencing cravings or failed attempts to reduce or stop use.
- Interference with Daily Life: Prioritizing drug use over responsibilities, relationships, or work.
Understanding Withdrawal
Benzodiazepine withdrawal can be severe, with symptoms ranging from mild anxiety to life-threatening seizures. The severity depends on factors like the specific medication, dosage, and duration of use. Withdrawal symptoms can include:
- Heightened anxiety and agitation
- Sleep disturbances
- Muscle tremors and tension
- Hallucinations in severe cases
- Seizures (particularly with abrupt cessation)
Treatment and Recovery
Managing benzodiazepine dependency requires a structured approach to minimize withdrawal risks and address underlying issues.
1. Tapering Off
A gradual dose reduction, under medical supervision, helps prevent severe withdrawal symptoms and complications. This slow tapering allows the body to adjust to decreasing drug levels.
2. Therapy and Psychological Support
Cognitive-behavioral therapy (CBT) is often used to address the psychological aspects of dependency. It helps individuals develop coping strategies for anxiety, stress, and insomnia without relying on medication.
3. Medication Management
In some cases, alternative medications such as antidepressants or non-addictive anxiolytics may be prescribed to manage underlying mental health conditions.
Benzodiazepines can be beneficial for short-term use, but long-term reliance carries significant risks. Awareness of dependency signs and early intervention can prevent severe withdrawal and complications. If you or a loved one is struggling with benzodiazepine dependency, seeking professional help is the first step toward recovery and long-term well-being.
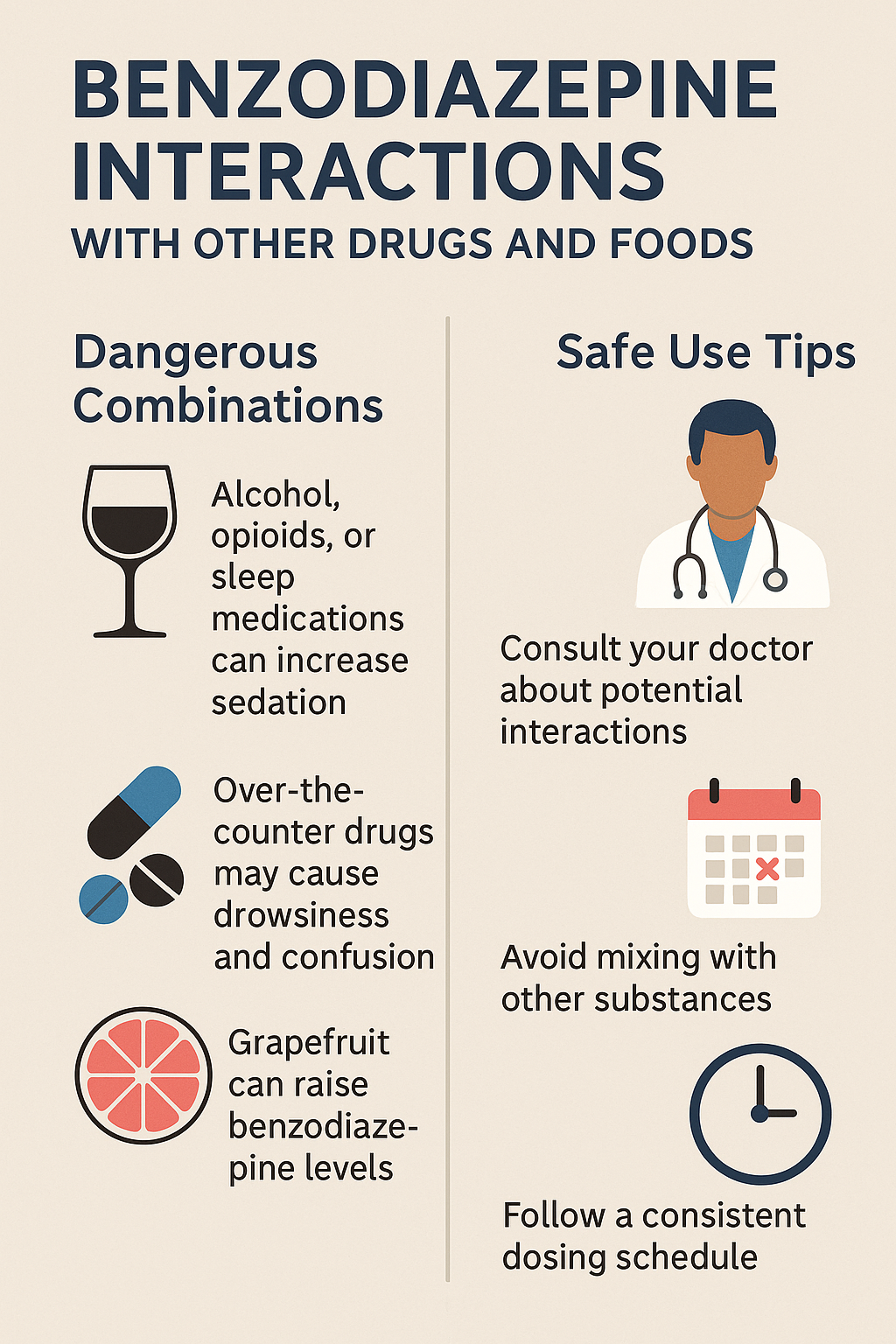
Understanding Benzodiazepine Interactions with Other Drugs and Foods
Benzodiazepines are widely prescribed for anxiety, insomnia, and muscle relaxation, but their interactions with other medications and substances can pose serious health risks. These interactions can lead to excessive sedation, respiratory depression, overdose, and even death. It’s crucial to be aware of potential interactions before combining benzodiazepines with other drugs or certain foods.
1. Central Nervous System (CNS) Depressants
- Opioids (e.g., morphine, oxycodone, fentanyl): Combining these with benzodiazepines significantly increases the risk of severe sedation, respiratory depression, coma, and death.
- Alcohol: A potent CNS depressant that, when mixed with benzodiazepines, can cause extreme drowsiness, impaired coordination, respiratory depression, and potentially fatal overdose.
- Antihistamines (e.g., diphenhydramine, chlorpheniramine): First-generation antihistamines can intensify benzodiazepine-induced sedation.
- Barbiturates: Another class of CNS depressants that can enhance the sedative and respiratory depressant effects of benzodiazepines, increasing overdose risk.
2. Antidepressants
- SSRIs and SNRIs (e.g., fluoxetine, sertraline, venlafaxine): These may heighten benzodiazepine sedation and influence metabolism, altering effectiveness and side effects.
- Tricyclic Antidepressants (e.g., amitriptyline, nortriptyline): Can increase sedation, confusion, and cognitive impairment when combined with benzodiazepines.
3. Antipsychotics
- Typical and Atypical Antipsychotics (e.g., haloperidol, olanzapine, quetiapine): Can amplify sedation and increase the risk of respiratory depression and low blood pressure.
4. Anticonvulsants (Seizure Medications)
- Phenytoin, carbamazepine: May alter benzodiazepine metabolism, either decreasing effectiveness or increasing sedative effects.
5. Antifungals
- Azole Antifungals (e.g., ketoconazole, itraconazole): These can inhibit liver enzymes responsible for metabolizing benzodiazepines, leading to higher drug levels and overdose risk.
6. Antibiotics
- Macrolide Antibiotics (e.g., erythromycin, clarithromycin): Can inhibit enzyme activity, increasing the effects and side effects of benzodiazepines.
7. HIV Medications
- Protease Inhibitors (e.g., ritonavir, lopinavir): These can inhibit liver enzymes, raising benzodiazepine levels and increasing overdose risks.
8. Cimetidine (and Other H2 Blockers)
- Cimetidine: This common acid-reducing medication can reduce benzodiazepine clearance, leading to enhanced sedative effects.
9. Grapefruit Juice
- Grapefruit juice: Contains compounds that inhibit liver enzymes (CYP3A4), slowing benzodiazepine metabolism and increasing drug levels in the body.
10. Other Metabolism-Affecting Drugs
- CYP3A4 Inhibitors (e.g., certain antidepressants, antifungals, antibiotics): Inhibiting this enzyme can enhance benzodiazepine effects and dangers.
Health Hazards of Benzodiazepine Interactions
- Respiratory Depression: Slowed or stopped breathing, especially when mixed with opioids or alcohol.
- Excessive Sedation: Impaired coordination, increased fall risk, and decision-making difficulties.
- Overdose Risk: Higher likelihood of overdose and coma when combined with CNS depressants.
- Cognitive and Motor Impairment: Memory, concentration, and motor skill disruptions that lead to accidents.
- Serotonin Syndrome: A rare but life-threatening condition when benzodiazepines are combined with serotonin-affecting drugs (e.g., SSRIs, SNRIs).
Key Safety Measures
- Always inform healthcare providers of all medications and supplements before starting benzodiazepines.
- Be cautious when combining benzodiazepines with CNS depressants.
- Follow prescribed guidelines for tapering off benzodiazepines to prevent withdrawal symptoms and complications.
Understanding the risks of benzodiazepine interactions can help prevent life-threatening complications. Always consult a healthcare professional before mixing medications or substances to ensure safe usage.
Recognizing the Physical Symptoms of Benzodiazepine Dependency
Benzodiazepine dependency or addiction manifests through a combination of physical and psychological symptoms. As the body adjusts to the drug, tolerance, dependence, and potential addiction develop. Below are key physical symptoms associated with benzodiazepine dependency.
1. Tolerance
- Increased Dosage Requirements: Individuals may need larger doses to achieve the same effects, such as relaxation or sleep.
- Diminished Effectiveness: The drug may no longer produce the desired effect, even at higher doses.
2. Withdrawal Symptoms
When benzodiazepine use is reduced or stopped, withdrawal symptoms can arise, varying in severity based on dosage, duration, and specific drug used.
- Tremors: Shaking hands or body tremors.
- Sweating: Increased perspiration, even in cool environments.
- Headaches: Persistent, intense headaches.
- Muscle Tension and Pain: Stiffness, soreness, or body aches.
- Insomnia: Difficulty falling or staying asleep.
- Nausea and Vomiting: Digestive distress as the body adjusts.
- Dizziness or Lightheadedness: Feelings of vertigo or imbalance.
- Heart Palpitations: Increased heart rate or irregular heartbeat.
- Seizures: A life-threatening withdrawal symptom in severe cases.
3. Physical Dependence
- Cravings: Intense desire to take the drug to relieve discomfort.
- Continued Use to Avoid Withdrawal: Using benzodiazepines solely to prevent withdrawal symptoms rather than for therapeutic purposes.
4. Sedation and Drowsiness
- Excessive Sleepiness: Overwhelming fatigue, impairing daily activities.
- Lethargy: Persistent lack of energy and motivation.
5. Coordination Problems
- Impaired Motor Skills: Increased risk of falls, stumbling, or unsteadiness.
- Slurred Speech: Slow or impaired speech, particularly at higher doses.
6. Memory and Cognitive Issues
- Short-Term Memory Impairment: Difficulty retaining new information or recalling recent events.
- Cognitive Slowing: Reduced ability to focus, think, or process information efficiently.
7. Changes in Appetite or Weight
- Increased Appetite and Weight Gain: Heightened food cravings, particularly during stress.
- Loss of Appetite and Weight Loss: Reduced food intake due to anxiety or discomfort.
8. Overdose Symptoms
In cases of excessive benzodiazepine use, overdose symptoms may include:
- Severe Drowsiness or Unresponsiveness: Difficulty staying awake or waking up.
- Slow or Difficult Breathing: Respiratory depression that can be life-threatening.
- Hypotension: Low blood pressure leading to dizziness or fainting.
- Cold or Clammy Skin: Indicating circulatory distress.
9. Chronic Health Issues
Long-term benzodiazepine dependency can contribute to chronic health conditions:
- Liver Damage: Increased risk of liver toxicity or failure.
- Kidney Problems: Impaired renal function over time.
- Gastrointestinal Issues: Chronic nausea, digestive distress, or stomach discomfort.
Benzodiazepine dependency presents a range of physical symptoms, from tolerance and withdrawal to severe health complications. Withdrawal can be hazardous, highlighting the importance of medical supervision when discontinuing use. If you or someone you know is struggling with benzodiazepine dependency, seeking professional help is crucial for a safe recovery.
Self-Management Strategies for Benzodiazepine Dependency
Benzodiazepine dependency can develop due to prolonged use or misuse of these medications. While they are effective for treating anxiety, insomnia, and other conditions, careful management is essential to avoid addiction. This blog outlines key self-management strategies to prevent and address benzodiazepine dependency while promoting overall well-being.
1. Follow Prescription Guidelines Strictly
- Take benzodiazepines exactly as prescribed by your healthcare provider.
- Avoid increasing the dosage without consulting a doctor.
- Never use benzodiazepines for conditions outside their intended use.
- Be aware of potential interactions with other medications or substances.
2. Limit Duration of Use
- Benzodiazepines should generally be used for short-term relief (2-4 weeks) to minimize the risk of dependency.
- Work with your doctor to regularly assess whether continued use is necessary.
- Establish a clear treatment plan that includes alternative therapies if needed.
3. Gradual Tapering to Avoid Withdrawal
- Avoid abruptly stopping benzodiazepines, as this can lead to severe withdrawal symptoms.
- Follow a gradual tapering schedule under medical supervision.
- Monitor for withdrawal symptoms such as anxiety, tremors, insomnia, or nausea.
4. Non-Medication Strategies for Stress and Anxiety Management
- Relaxation Techniques: Practice deep breathing, meditation, and progressive muscle relaxation.
- Cognitive Behavioral Therapy (CBT): CBT is a proven method for managing anxiety and sleep disorders.
- Exercise: Regular physical activity helps reduce stress and improve mood.
- Healthy Routine: Maintain a structured daily schedule with proper sleep, nutrition, and hydration.
5. Monitor for Signs of Tolerance or Dependence
- Keep track of how often you take benzodiazepines.
- Be aware of increasing dosage needs or feeling reliant on the medication.
- Recognize psychological dependence, such as the fear of coping without the drug.
6. Avoid Alcohol and Other Depressants
- Alcohol and CNS depressants enhance the sedative effects of benzodiazepines, increasing overdose risk.
- Limit the use of over-the-counter sleep aids or antihistamines that can interact with benzodiazepines.
7. Seek Professional Support
- Engage in therapy, such as CBT, to manage anxiety without medication.
- Join support groups or counseling programs to gain insight from others with similar experiences.
- Consult a healthcare provider for alternative anxiety treatments if necessary.
8. Educate Yourself on Benzodiazepine Risks
- Learn about the dangers of long-term benzodiazepine use, including tolerance and withdrawal.
- Recognize warning signs of dependency, such as cravings, dosage escalation, or lack of control over usage.
9. Develop Healthy Coping Mechanisms
- Use mindfulness and meditation to manage stress.
- Engage in hobbies or social activities that provide emotional relief without medication.
- Maintain a strong support system with friends and family.
10. Regular Check-ins with Healthcare Providers
- Schedule routine medical appointments to review your medication use.
- Discuss concerns about dependency and explore alternative treatments.
- Work with a doctor to create a structured tapering plan for reducing benzodiazepine use.
Managing benzodiazepine use responsibly is crucial for preventing dependency. By following prescription guidelines, practicing healthy coping mechanisms, and seeking professional guidance, individuals can minimize risks while effectively managing anxiety and related conditions. If you suspect dependency, consult a healthcare provider to develop a safe and structured plan for recovery.
Family Support Strategies for Preventing Benzodiazepine Dependency
Benzodiazepine dependency is a significant concern for individuals prescribed these medications for anxiety, sleep disorders, or other conditions. Family support plays a crucial role in ensuring safe medication use and preventing dependency. By fostering open communication, monitoring medication use, and promoting healthy alternatives, families can help loved ones maintain control over their benzodiazepine use and overall well-being.
1. Encourage Open Communication
- Create a Safe Space for Discussion: Foster an environment where the person feels comfortable discussing their medication use without fear of judgment or criticism.
- Express Concerns with Care: If you notice signs of dependency, approach the topic calmly and empathetically, focusing on their well-being rather than assigning blame.
2. Monitor Medication Use
- Track Dosage and Frequency: Help ensure medications are taken exactly as prescribed by keeping a medication log.
- Establish Boundaries: Encourage the person to follow medical advice strictly and avoid any unauthorized dosage increases.
- Secure Medication Storage: Keep medications in a safe place to prevent misuse or accidental overuse.
3. Promote Medical Adherence
- Encourage Regular Doctor Visits: Ensure the person checks in with their healthcare provider to review their treatment plan.
- Support Tapering When Necessary: If long-term use is a concern, assist in discussing a gradual dose reduction plan with their doctor.
4. Provide Emotional and Practical Support
- Be Understanding: Acknowledge the person’s struggles and offer reassurance.
- Encourage Healthy Distractions: Engage in activities such as exercise, hobbies, or relaxation techniques to reduce reliance on medication.
5. Foster Healthy Lifestyle Choices
- Encourage Stress Management Techniques: Introduce mindfulness, meditation, and deep breathing exercises.
- Promote Physical Activity: Exercise is a natural way to improve mood and reduce anxiety.
- Support Healthy Sleep Hygiene: Help create a consistent sleep schedule and an environment conducive to rest without relying on medication.
6. Educate About Risks and Alternatives
- Provide Information on Dependency Risks: Awareness helps in recognizing early warning signs.
- Explore Alternative Treatments: Encourage therapy, non-addictive medications, or holistic approaches as substitutes for benzodiazepines.
7. Be Vigilant for Warning Signs
- Watch for Behavioral Changes: Signs such as increased use, doctor shopping, or secretive behavior may indicate dependence.
- Recognize Withdrawal Symptoms: Symptoms like anxiety, tremors, or insomnia may signal the need for professional support.
8. Encourage Therapy and Support Groups
- Suggest Therapy for Underlying Issues: Anxiety and insomnia can often be managed through Cognitive Behavioral Therapy (CBT) rather than medication.
- Recommend Support Groups: Groups like Narcotics Anonymous (NA) provide peer support and accountability.
9. Provide Positive Reinforcement
- Acknowledge Progress: Praise adherence to prescribed use and any positive steps taken toward reducing dependence.
- Celebrate Small Wins: Recognizing milestones, even minor ones, can boost confidence and motivation.
10. Seek Professional Family Counseling
- Consider Family Therapy: A therapist can help improve communication and family dynamics surrounding medication use.
- Get Guidance from Professionals: Addiction counselors and healthcare providers can offer tailored support strategies.
11. Be Patient and Non-Judgmental
- Avoid Blame or Shame: Dependency is complex, and shaming can deter someone from seeking help.
- Exercise Patience: Progress is often gradual, and setbacks may occur—continue offering support and encouragement.
Preventing benzodiazepine dependency within a family requires proactive involvement, education, and emotional support. By fostering open discussions, encouraging responsible medication use, and offering alternative coping mechanisms, families can play a crucial role in reducing the risk of dependency and promoting long-term well-being.
Community Resource Strategies for Preventing Benzodiazepine Dependency
Community resources play a crucial role in preventing benzodiazepine addiction or dependency by offering support, education, and access to alternative treatments. By leveraging local services and programs, individuals can better manage stress, anxiety, and other underlying conditions without relying solely on benzodiazepines. Here are effective community resource strategies to help prevent benzodiazepine addiction or dependency.
1. Public Awareness and Education Campaigns
- Promote Awareness of the Risks: Community organizations, healthcare providers, and local governments can run educational campaigns about the dangers of benzodiazepine misuse, dependency, and addiction.
- Offer Information on Alternatives: Provide information on non-addictive alternatives for managing anxiety, insomnia, and stress, such as cognitive behavioral therapy (CBT), relaxation techniques, and lifestyle changes.
- Host Workshops or Seminars: Organize workshops or public seminars led by healthcare professionals to educate the community about the safe use of benzodiazepines and available treatment options.
2. Access to Mental Health Services
- Community Mental Health Centers: Offer access to therapy, counseling, and psychiatric care for individuals struggling with conditions that may lead to benzodiazepine use.
- Sliding Scale Services: Provide income-based mental health services for individuals without private insurance or the financial means to afford treatment.
- Peer Support Groups: Facilitate support groups, such as those provided by Mental Health America, to offer a safe space for individuals dealing with anxiety, insomnia, or substance use concerns.
3. Substance Use and Addiction Prevention Programs
- Substance Abuse Prevention Programs: Implement community-based programs that educate on prescription drug misuse and dependency risks.
- School and College Programs: Introduce initiatives in educational institutions to raise awareness about prescription drug risks and promote healthy coping mechanisms.
- Community Health Fairs: Organize events that provide information on substance use disorders, offer screenings for at-risk individuals, and offer free resources for those seeking help.
4. Access to Non-Pharmacological Treatments
- Cognitive Behavioral Therapy (CBT): Promote community clinics that offer CBT for anxiety and insomnia without medication.
- Mindfulness and Meditation: Provide mindfulness-based stress reduction (MBSR) classes or meditation sessions at wellness centers.
- Yoga and Exercise Programs: Offer community fitness programs that help manage stress and anxiety in a healthy, non-addictive manner.
5. Collaborative Care Networks
- Integrated Care Teams: Foster collaboration between primary care providers, mental health professionals, addiction specialists, and community outreach programs.
- Referral Networks: Ensure healthcare providers connect individuals struggling with benzodiazepine use to appropriate services, including addiction counseling and mental health care.
6. Support for Families and Caregivers
- Family Education Programs: Provide educational programs for families and caregivers to help them understand benzodiazepine dependency and recognize early warning signs.
- Family Support Groups: Establish local support groups to guide families in effectively supporting loved ones without enabling dependency.
- Caregiver Training: Offer community training for caregivers to develop skills in managing care for individuals with benzodiazepine dependency.
7. Public Health Initiatives
- Prescription Drug Monitoring Programs (PDMPs): Utilize tracking programs to identify patterns of overuse or misuse and detect potential dependency early.
- Naloxone and Harm Reduction Programs: While benzodiazepines are not opioid-based, harm reduction strategies like naloxone distribution and safe-use education can help foster awareness about substance use risks.
8. Access to Emergency and Crisis Intervention Services
- Crisis Hotlines: Establish hotlines to provide immediate support and resources for individuals experiencing a mental health or addiction crisis related to benzodiazepine use.
- Crisis Intervention Teams: Train healthcare providers and law enforcement in crisis intervention to safely connect individuals at risk with medical care or addiction treatment services.
9. Collaboration with Local Healthcare Providers
- Doctor and Pharmacist Partnerships: Encourage collaboration between healthcare professionals to ensure responsible benzodiazepine prescribing and monitoring.
- Patient Education at Pharmacies: Provide patient counseling on the proper use of benzodiazepines and safe tapering strategies.
10. Community-Based Rehabilitation and Recovery Programs
- Addiction Recovery Centers: Establish community-based programs offering detoxification, inpatient, and outpatient care for individuals with benzodiazepine dependency.
- Recovery Support Services: Provide aftercare programs, sober living homes, and job support to help individuals maintain recovery.
Community resources provide a wide range of support systems that can help prevent benzodiazepine dependency. By increasing public awareness, improving access to mental health services, offering alternative treatments, and fostering collaborative healthcare efforts, communities can play a pivotal role in reducing the risk of benzodiazepine addiction while promoting healthier approaches to managing anxiety and sleep disorders.
Frequently Asked Questions
Here are some common questions:
Question: Why is Benzodiazepine so easy to become dependent on and lead to addiction?
Answer: Benzodiazepines (benzos) are highly prone to dependency and addiction due to their effects on the brain and body. Several key factors contribute to this:
1. Rapid Action on the Brain
Benzos enhance the effect of gamma-aminobutyric acid (GABA), a neurotransmitter that slows brain activity. This results in immediate relaxation, sedation, and reduced anxiety. However, the brain quickly adapts to this artificial boost, making it harder to function without the drug.
2. Tolerance Develops Quickly
With repeated use, the brain becomes less responsive to the drug, meaning a person must take higher doses to achieve the same effect. This rapid tolerance leads to escalating use, increasing the risk of dependency.
3. Short-Term Relief, Long-Term Problem
Benzos are often prescribed for anxiety, panic disorders, or insomnia, conditions that require long-term management. Since benzos provide quick relief, people may rely on them instead of developing long-term coping skills, reinforcing dependency.
4. Rebound Anxiety & Withdrawal Symptoms
When someone tries to stop or reduce their dose, they often experience rebound symptoms, meaning their original anxiety or insomnia returns even worse than before. Withdrawal symptoms—such as panic attacks, tremors, and seizures—can be severe, making it difficult to quit without medical supervision.
5. Psychological Dependence
Beyond physical dependence, benzos can create a psychological reliance. People may feel they cannot function without them, leading to compulsive use even when they know the risks.
6. Long Half-Life & Accumulation
Some benzos have a long half-life, meaning they stay in the system for an extended period. Regular use leads to drug accumulation in the body, increasing the risk of sedation, memory issues, and dependency.
7. Misuse & Overprescription
Benzos are commonly prescribed, and many users are unaware of their addictive potential. Some people take higher doses than prescribed or mix them with alcohol or opioids, significantly increasing the risk of overdose and addiction.
How to Prevent Dependency?
Gradual tapering instead of sudden stopping to avoid severe withdrawal.
Use for short periods only (preferably under four weeks).
Follow medical guidelines strictly—never self-adjust dosage.
Explore alternatives like Cognitive Behavioral Therapy (CBT), mindfulness, or lifestyle changes for anxiety or insomnia.
Question: How to safely taper off benzodiazepines or alternative treatments?
Answer: How to Safely Taper Off Benzodiazepines
Tapering off benzodiazepines (benzos) should always be done gradually and under medical supervision to prevent withdrawal symptoms, which can be severe or even life-threatening. Here’s how to safely taper:
1. Consult a Doctor First
- Never stop benzos suddenly (“cold turkey”), as this can cause seizures, panic attacks, and severe withdrawal symptoms.
- A healthcare provider can help create a personalized tapering schedule based on:
- The type of benzo taken (short-acting like Xanax vs. long-acting like Valium)
- Dosage and duration of use
- Individual health and risk factors
2. Gradual Dose Reduction (Slow Tapering)
- General rule: Reduce the dose by 5-10% every 2-4 weeks, depending on tolerance.
- For long-term users, the taper may need to be even slower (e.g., 2.5% reductions).
- If withdrawal symptoms are severe, the dose can be held stable before making further reductions.
Example Taper for Xanax (Alprazolam) 1 mg per day:
- Week 1-2: Reduce to 0.75 mg/day
- Week 3-4: Reduce to 0.5 mg/day
- Week 5-6: Reduce to 0.25 mg/day
- Week 7-8: Reduce to 0.125 mg/day
- Stop completely
Note: Some doctors may switch short-acting benzos (Xanax, Ativan) to a long-acting one like Valium (Diazepam) for an easier taper.
3. Monitor and Manage Withdrawal Symptoms
Common withdrawal symptoms include:
✔ Anxiety, panic attacks
✔ Insomnia, restlessness
✔ Muscle pain, tremors
✔ Sweating, nausea
✔ Seizures (in severe cases)
Ways to manage withdrawal:
- Stay hydrated and eat nutritious foods
- Practice deep breathing, meditation, or yoga
- Engage in mild exercise to reduce stress
- Use melatonin or magnesium for sleep support
- Avoid alcohol, caffeine, or stimulants
- Consider therapy or counseling for anxiety
4. Consider Alternative Treatments for Anxiety & Insomnia
Instead of benzodiazepines, the following options can be used:
Behavioral & Psychological Approaches
✔ Cognitive Behavioral Therapy (CBT) – Proven effective for anxiety and insomnia.
✔ Mindfulness & Meditation – Helps retrain the brain to manage stress without medication.
✔ Progressive Muscle Relaxation – Reduces tension and calms the nervous system.
✔ Biofeedback Therapy – Helps control stress responses.
Non-Benzodiazepine Medications
✔ Antidepressants (SSRIs/SNRIs) – Like Prozac or Lexapro for anxiety disorders.
✔ Buspirone (Buspar) – A non-addictive anxiety medication.
✔ Hydroxyzine (Vistaril) – An antihistamine with anxiety-relief effects.
✔ Gabapentin or Pregabalin – Sometimes used for withdrawal symptoms.
Lifestyle Changes & Natural Remedies
✔ Regular Exercise – Boosts natural anti-anxiety brain chemicals.
✔ Dietary Adjustments – Avoid processed foods, sugar, and caffeine.
✔ Herbal Supplements – (Under doctor guidance)
- Ashwagandha – Reduces stress
- L-theanine – Calming effect
- Passionflower or Valerian Root – Helps with sleep
5. Seek Support (Don’t Do It Alone!)
- Therapy & Support Groups: Consider joining Benzodiazepine Withdrawal Support Groups.
- Family & Friends: Let them know about the taper to encourage.
- Medical Supervision: Regular check-ins with a doctor ensure safe progress.
Tapering off benzodiazepines is a gradual process that requires patience, medical guidance, and lifestyle adjustments. By replacing benzos with healthier coping strategies and alternative treatments, long-term recovery and anxiety management are achievable.
Question: What is the brain interaction that can interact with Benzodiazepine and opioids and lead to death?
Answer: How Benzodiazepines and Opioids Interact in the Brain and Lead to Death
When benzodiazepines (e.g., Xanax, Valium, Ativan) and opioids (e.g., oxycodone, heroin, fentanyl) are taken together, they create a deadly synergy that dramatically increases the risk of overdose and death. This occurs due to their combined effects on the central nervous system (CNS), particularly in brain regions that control breathing and consciousness.
1. Depressing the Central Nervous System (CNS)
Both benzodiazepines and opioids are CNS depressants, meaning they slow down brain activity, breathing, and heart rate. Their combined effects multiply, leading to:
✔ Profound sedation (extreme drowsiness, unconsciousness)
✔ Severe respiratory depression (slow or stopped breathing)
✔ Decreased heart rate and blood pressure
✔ Loss of airway control (choking or aspiration)
Because of this synergistic effect, people can stop breathing in their sleep without realizing it—leading to overdose and death.
2. Brain Receptors Involved in the Deadly Interaction
Opioids: Mu-Opioid Receptors (MOR) → Respiratory Depression
Opioids (like heroin, fentanyl, oxycodone) bind to mu-opioid receptors (MOR) in the brainstem (medulla), which:
✔ Blocks pain signals (analgesia)
✔ Produces euphoria (pleasure/reward system)
❌ Suppresses the brain’s drive to breathe
When opioids bind to these receptors too strongly, the brainstem stops sending signals for breathing, leading to respiratory failure.
Benzodiazepines: GABA-A Receptors → Enhanced Sedation
Benzodiazepines bind to GABA-A receptors, enhancing the effects of gamma-aminobutyric acid (GABA), the brain’s primary inhibitory neurotransmitter. This results in:
✔ Increased sedation and muscle relaxation
✔ Reduced anxiety
✔ Suppressed brain activity
Usually, benzodiazepines don’t cause fatal overdoses alone because they don’t directly suppress breathing. However, when taken with opioids, they enhance the brain’s suppression of breathing and unconsciousness—leading to a high risk of overdose.
3. The Deadly Synergy: How Benzos + Opioids Cause Fatal Overdose
- Opioids weaken the brain’s breathing reflex by suppressing the brainstem.
- Benzodiazepines amplify sedation, making the person less responsive.
- The person stops breathing due to combined CNS depression.
- Lack of oxygen (hypoxia) leads to brain damage, coma, or death.
Even therapeutic doses of benzos and opioids can be lethal in some individuals due to their potentiating effects.
4. Risk Factors That Increase Overdose Deaths
🚨 Mixing high doses – Even low doses combined can be fatal.
🚨 Taking both drugs recreationally – Higher risk of overdose.
🚨 Using alcohol or other depressants – Further slows breathing.
🚨 Pre-existing conditions – Sleep apnea, lung disease, or heart conditions increase risk.
🚨 Fentanyl contamination – Many street opioids are laced with fentanyl, which is 50-100x stronger than morphine.
5. Preventing Overdose & Harm Reduction
✔ Avoid Mixing Benzos and Opioids – Unless necessary under strict medical supervision.
✔ Use Naloxone (Narcan) – An opioid overdose reversal drug that can help restore breathing if opioids are involved.
✔ Gradually Reduce Dependence – If prescribed both, discuss tapering with a doctor.
✔ Supervised Use (If Necessary) – Some harm reduction programs provide safer-use spaces.
The interaction between benzodiazepines and opioids is hazardous, primarily because they both depress the central nervous system and shut down breathing. Even when prescribed, their combination should be closely monitored, and alternatives should be considered whenever possible.
Conclusion
While benzodiazepines are valuable tools for managing anxiety, insomnia, and other mental health conditions, their potential for addiction and dependency when misused or overused is a significant concern. The risk of dangerous interactions with substances like alcohol and opioids, coupled with physical symptoms such as increased tolerance and withdrawal, makes careful monitoring essential. Effective prevention strategies involve self-management through responsible use, exploring non-addictive treatment options, and maintaining healthy lifestyle practices. Family support, with open communication and positive coping mechanisms, plays a crucial role in helping individuals navigate the risks of dependency. Additionally, community resources, including education, mental health services, and addiction support programs, are vital in providing individuals with the necessary tools and support to manage their health and reduce the risk of addiction safely.
Video: Why You Should Never Mix These Medicines