Telemedicine has expanded access to opioid use disorder (OUD) treatment, but barriers remain, including technology gaps, regulatory hurdles, and stigma. Pharmacies pose challenges, including reluctance to dispense medications, limited stocking of buprenorphine, and insurance restrictions. Solutions like pharmacist training, stronger provider–pharmacy collaboration, and patient support networks can ease these barriers. Government efforts—through regulatory reforms, funding, insurance expansion, and anti-stigma campaigns—are shaping a more supportive system. Together, these measures strengthen telemedicine’s role in addressing the opioid crisis.
Barriers to Telemedicine in Addiction Treatment
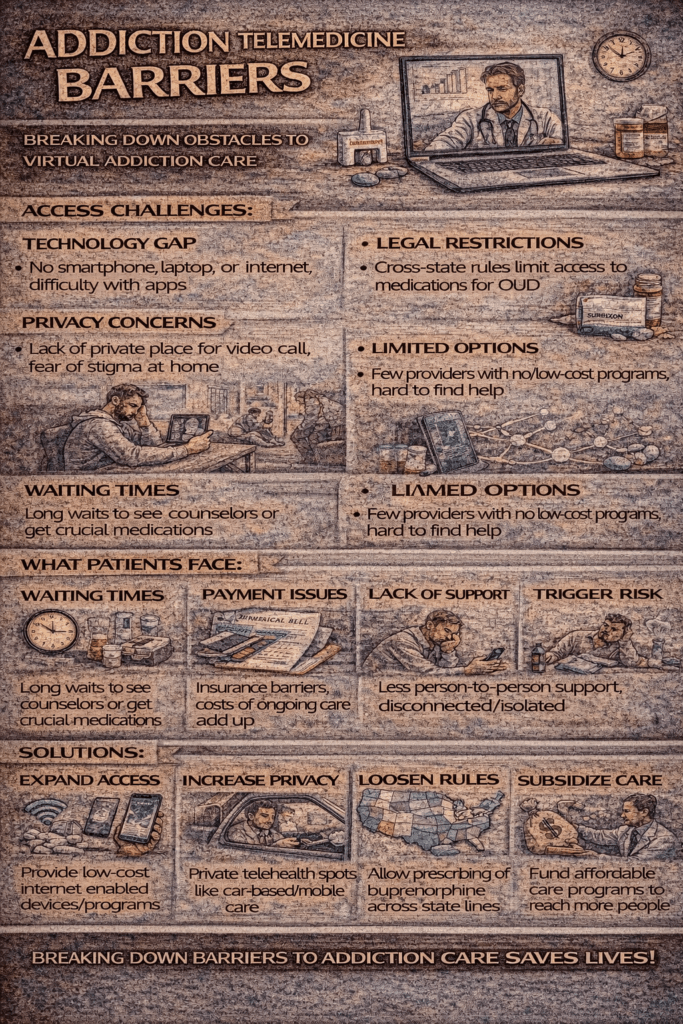
Telemedicine has emerged as a valuable tool for expanding access to addiction treatment, especially during and after the COVID-19 pandemic. It reduces travel burdens, improves access in underserved areas, and helps people connect with care more quickly. However, several barriers limit its effectiveness. These challenges fall into structural, technological, financial, and personal categories:
1. Technological Barriers
- Limited internet access or unreliable connectivity, especially in rural or low-income areas.
- Lack of access to smartphones, computers, or private spaces for virtual appointments.
- Older adults or those with limited digital literacy may struggle with telehealth platforms.
2. Regulatory and Policy Barriers
- Varying state and federal rules on prescribing controlled substances (like buprenorphine for opioid use disorder).
- Confusion as temporary COVID-19 telehealth policies are phased out or updated.
- Licensing restrictions that prevent providers from practicing across state lines.
3. Financial and Insurance Barriers
- Limited insurance coverage or lower reimbursement rates for telemedicine compared to in-person visits.
- Out-of-pocket costs for devices, internet, or data plans.
- Insufficient funding for programs that build telehealth infrastructure.
4. Clinical and Privacy Concerns
- Harder to build therapeutic rapport or conduct complete assessments without in-person interaction.
- Challenges include monitoring withdrawal symptoms, medication use, or possible diversion.
- Privacy risks exist if patients lack a safe, confidential space at home.
5. Social and Personal Barriers
- Stigma around addiction treatment discourages people from seeking help, even virtually.
- Unstable housing or unsafe environments (like domestic violence) that make telehealth sessions difficult.
- Distrust of technology or discomfort with virtual communication.
In summary, telemedicine holds great promise in making addiction treatment more accessible, but these barriers highlight why a one-size-fits-all approach doesn’t work. Solutions require better access to technology, clearer regulations, fair insurance coverage, and stronger community support. By addressing these challenges, telemedicine can continue to evolve into a powerful tool for recovery.
Pharmacy Barriers in Telemedicine for Opioid Use Disorder
Telemedicine has made it easier for patients with opioid use disorder (OUD) to connect with prescribers and receive treatment, but accessing medication doesn’t end with a prescription. A significant challenge lies in pharmacy-related barriers, where stigma, regulations, and supply issues often limit care. Here are the key obstacles:
1. Stigma and Hesitancy
- Some pharmacists remain reluctant to dispense buprenorphine or other OUD medications due to misconceptions that it “just replaces one drug with another.”
- Patients may experience judgment or uncomfortable interactions when filling prescriptions, discouraging them from staying in treatment.
2. Regulatory and Legal Barriers
- Complex and evolving laws around prescribing controlled substances through telemedicine create confusion.
- Methadone is tightly restricted and cannot be dispensed at retail pharmacies, requiring patients to visit certified opioid treatment programs (OTPs).
- Some pharmacies impose their own internal policies that limit or reject prescriptions issued through telemedicine.
3. Supply and Stocking Issues
- Not all pharmacies carry buprenorphine, often due to perceived low demand, fear of regulatory scrutiny, or diversion concerns.
- Rural and smaller pharmacies may struggle to maintain adequate supplies, delaying patient access.
4. Coordination and Communication Gaps
- Telemedicine prescribers may lack established relationships with local pharmacists, leading to miscommunication or prescription delays.
- Pharmacists may hesitate to fill prescriptions from out-of-state or unfamiliar providers.
5. Insurance and Cost Barriers
- Insurance rules such as prior authorizations, step therapy, or quantity limits can slow down treatment.
- Some pharmacies may not accept insurance used by telemedicine patients, forcing them to travel farther.
6. Patient Access Challenges
- Rural patients may need to drive long distances to find a willing pharmacy.
- For individuals without transportation or stable housing, pharmacy access remains a barrier even when telemedicine makes prescribing easier.
In summary, telemedicine can make it easier to see a doctor, but getting medication in hand is another story. Pharmacy barriers—ranging from stigma to supply gaps—can undo the progress telehealth promises. Addressing these challenges will require stronger collaboration between prescribers, pharmacists, insurers, and policymakers to ensure that patients can access the full benefits of OUD treatment.
Government Interventions to Expand Telemedicine for Opioid Use Disorder
Government policies have played—and continue to play—a critical role in making telemedicine for opioid use disorder (OUD) more accessible. By adjusting regulations, expanding funding, and reducing barriers, policymakers are helping telehealth become a lasting part of addiction treatment. Here are the main areas of intervention:
1. Regulatory Flexibility for Prescribing
- Ryan Haight Act Adjustments: During COVID-19, waivers allowed clinicians to start buprenorphine treatment via telemedicine without an initial in-person exam. The DEA and HHS are now working on making parts of this flexibility permanent.
- Cross-State Licensing Initiatives: Some states participate in compacts or offer emergency waivers to allow providers to treat patients across state lines.
- Relaxed Take-Home Rules for Methadone: SAMHSA expanded take-home privileges for methadone, reducing daily clinic visits.
2. Funding and Infrastructure Support
- Grants & Federal Funding: Agencies like HRSA and SAMHSA support telehealth programs in rural and underserved areas.
- Broadband Expansion: Federal programs, including the FCC’s Rural Digital Opportunity Fund and the Broadband Equity Access and Deployment program, aim to close the digital divide.
- Telehealth Resource Centers: Regional centers funded by government grants provide training and technical support.
3. Insurance and Reimbursement Policies
- Medicaid Expansion for Telehealth: Many states require Medicaid to cover OUD telehealth treatment at the same level as in-person care.
- Medicare Coverage: Expanded to include OUD counseling and therapy delivered virtually.
- Private Insurance Parity Laws: Some states mandate equal reimbursement for telehealth and in-person care.
4. Training and Workforce Development
- Telehealth Training Programs: SAMHSA funds provider education on virtual addiction care.
- Expanding Waivered Providers: The removal of the X-waiver in 2023 allows more clinicians to prescribe buprenorphine, including via telehealth.
5. Public Health & Anti-Stigma Campaigns
- Awareness Campaigns: Governments highlight telehealth as a legitimate, safe way to receive treatment, helping reduce stigma.
- Integration with Harm Reduction Services: Federal support encourages linking telehealth with syringe services, naloxone distribution, and mobile outreach.
In summary, government interventions are central to making telemedicine a permanent, practical pathway for OUD treatment. By loosening prescribing rules, expanding funding, improving insurance coverage, supporting providers, and reducing stigma, these policies help patients—especially those in rural or underserved communities—gain reliable access to lifesaving care.
Frequently Asked Questions
Here are some common questions:
Question: What are solutions or best practices (for providers, pharmacies, and patients) to overcome these pharmacy barriers in telemedicine OUD treatment?
Answer: Solutions and best practices that can help overcome pharmacy barriers in telemedicine OUD (Opioid Use Disorder) treatment. I’ve grouped them by pharmacy level, provider level, and patient/community level so you can see where improvements can be made:
🔹 1. Pharmacy-Level Solutions
- Education & Training: Offer pharmacists continuing education on OUD, the safety of buprenorphine, and how telemedicine prescribing works to reduce stigma and misconceptions.
- Expand Stocking Practices: Encourage pharmacies to maintain consistent supplies of buprenorphine and naloxone. Chain pharmacies could create corporate-level policies to standardize this.
- Clear Guidelines: Provide pharmacists with state and federal updates on telemedicine rules so they feel confident filling prescriptions without fear of regulatory action.
- Confidentiality Practices: Train staff on how to handle OUD prescriptions discreetly, reducing stigma at the counter.
🔹 2. Provider-Level Solutions (Telemedicine Clinics & Prescribers)
- Pharmacy Partnerships: Build relationships with local and regional pharmacies to create a “trusted network” that reliably fills OUD prescriptions.
- Communication Channels: Set up direct lines (fax, secure email, phone) for pharmacists to verify telemedicine prescriptions quickly and reduce delays.
- Prescription Clarity: Ensure prescriptions are written with accurate DEA numbers, dosage clarity, and compliance with state rules to prevent rejections.
- Collaborative Care: Encourage regular case coordination between prescribers and pharmacists, especially for patients with complex needs.
🔹 3. Patient & Community-Level Solutions
- Pharmacy Navigation Support: Provide patients with a list of “OUD-friendly” pharmacies that stock buprenorphine and are comfortable with telemedicine prescriptions.
- Medication Delivery: Use mail-order or delivery pharmacies when local options are limited, especially for rural patients.
- Patient Education: Teach patients how to advocate for themselves at the pharmacy counter and provide them with documentation (such as prescriber contact information) in case of issues.
- Community Pharmacy Engagement: Partner with local organizations, public health departments, or recovery programs to normalize pharmacies as part of the treatment team.
🔹 4. Policy & System-Level Solutions
- Insurance Reform: Simplify prior authorization processes and remove unnecessary restrictions for OUD medications.
- Regulatory Clarity: Ensure the DEA and state boards issue clear, updated guidance on telemedicine prescribing rules to reduce uncertainty.
- Incentives for Pharmacies: Provide reimbursement or grants for rural pharmacies that stock and dispense OUD medications.
- Anti-Stigma Campaigns: Launch public health efforts to reduce stigma in pharmacies and highlight their role in recovery support.
In summary, by combining education, communication, stocking policies, patient support, and systemic reforms, pharmacy barriers in telemedicine OUD treatment can be significantly reduced. This ensures that telemedicine not only improves access to prescribing but also guarantees that patients can actually receive their life-saving medications.
Question: Compare U.S. and international government approaches (e.g., Canada, UK, Australia) to see how different governments promote telemedicine for OUD treatment.
Answer: Governments in the U.S., Canada, the U.K., and Australia have approached promoting telemedicine for opioid use disorder (OUD) treatment.
United States
- Permanent Flexibilities for Telehealth Prescribing
The Substance Abuse and Mental Health Services Administration (SAMHSA) has made permanent the COVID-era policy allowing telemedicine initiation of both methadone (via audiovisual tech) and buprenorphine (via audio-only or audiovisual) without an initial in-person visit. It also expanded take-home doses and removed stigmatizing language in regulations from the American Medical Association. - Extended Telemedicine Flexibility Window
Under current DEA and HHS regulations, controlled substances (like buprenorphine) can be prescribed via telemedicine without in-person evaluation through December 31, 2025, although a delayed permanent rule is expected p2p.uky.edu. - Demonstrated Positive Patient Outcomes
Medicaid-based studies in Kentucky and Ohio found that patients initiated on buprenorphine via telehealth had significantly higher odds of 90-day treatment retention compared to traditional in-person starts (e.g., Kentucky: OR 1.13; Ohio: OR 1.19) NCBIccts.uky.edu.
Canada
- Rapid Regulatory Adaptations During COVID-19
In response to the pandemic, Canada issued emergency exemptions that enabled verbal prescriptions for controlled substances and authorized pharmacists to extend and renew OUD medications. Multiple provinces, including Quebec, issued national and regional guidelines to adopt telemedicine for opioid agonist therapy (OAT), support unsupervised dosing, and facilitate prescribing during self-isolation PubMed Central. - Broad Uptake by OAT Clinics
By mid-2020, more than half of the surveyed OAT clinics in Canada had adopted telemedicine for prescribing, showing swift integration into practice PubMed Central.
United Kingdom
- Evidence Supporting Telehealth Retention
A University of Kentucky study, though U.S.–based, underscores retention benefits of telehealth for OUD treatment and may inform UK policy discussions at UKNowccts.uky.edu. - No Governmental Telemedicine-Specific Policy Identified
While UK healthcare does offer telemedicine services, there’s no publicly documented national policy specifically promoting telemedicine for OUD treatment—at least not within the available sources.
Australia
- Telehealth Integrated into Mental Health Services
Since around 2017, Australians in rural and remote areas with a Mental Health Treatment Plan have been able to access rebated video-consultation services via Medicare for psychological care, according to Wikipedia. - Telehealth Growth for OUD During COVID-19
The pandemic accelerated telehealth adoption in OUD treatment, particularly telephone support—a modality preferred by some patients because it does not require internet access. Telehealth-delivered opioid agonist therapy (OAT) showed promising retention, with one study reporting 50%–year retention versus 39% with traditional models Frontiers. - Structural Challenges to Sustainability
A regional Victoria telehealth-based opioid substitution clinic demonstrated effectiveness, but lacked financial viability under the current Medicare Benefits Schedule (MBS). The study called for increased telehealth rebates or external funding to sustain such models, RACGP. - Digital Infrastructure Support
The Australian Digital Health Agency supports telemedicine through systems like digital prescriptions and My Health Record. Since May 2020, over 115 million digital prescriptions have been issued, facilitating streamlined medication delivery through telehealth platforms, according to Wikipedia. - Methadone Delivery Through Primary Care and Pharmacies
In contrast to the U.S., Australia allows GPs to prescribe methadone and community pharmacies to dispense it, though regulations and training differ by state. This model supports easier integration with telehealth when prescriptions are provided remotely by the Pew Charitable Trusts.
Comparative Table
| Medicare-supported tele-mental health, tele-OUD trial pilots with funding gaps, robust digital prescribing infrastructure, primary care/pharmacy methadone model | Key Government Interventions for Tele-OUD |
|---|---|
| U.S. | Permanent telehealth prescribing flexibilities (SAMHSA), extended regulatory window, improved retention outcomes |
| Canada | Emergency telemedicine adoption, flexible OAT guidelines, widespread clinic uptake |
| U.K. | Evidence supports telehealth benefits, but no national policy explicitly targeting tele-OUD treatment available |
| Australia | Medicare-supported tele mental health, tele-OUD trial pilots with funding gaps, robust digital prescribing infrastructure, primary care/pharmacy methadone model |
Summary
The U.K., while showing interest via clinical research, appears not to have a distinct national-level telemedicine policy for OUD in published material.
The U.S. and Canada have implemented rapid regulatory changes to enable telemedicine for the initiation and continuation of OUD treatment—the U.S. aiming for permanence, Canada enabling it via emergency and consultative frameworks.
Australia supports telehealth through existing mental health funding and digital infrastructure, though sustainable reimbursement for OUD-specific services is a work in progress.
Question: What are the telemedicine barriers to individuals with addiction?
Answer: For individuals with addiction, telemedicine can be life-saving, but they often face unique barriers that limit its effectiveness. These can be grouped into several categories:
1. Technological Barriers
- Lack of reliable internet or devices (smartphone, computer, webcam).
- Difficulty finding a private space for appointments (especially for those in unstable housing).
- Limited digital literacy, particularly among older adults or individuals new to technology.
2. Financial Barriers
- Out-of-pocket costs for internet/data plans or devices.
- Limited insurance coverage or reimbursement gaps for telemedicine visits.
- Difficulty affording medications if telehealth providers do not accept insurance.
3. Regulatory & Pharmacy Barriers
- Restrictions on prescribing controlled substances (like buprenorphine or methadone) via telemedicine.
- Pharmacies are refusing to stock or dispense OUD medications due to stigma or internal policies.
- Confusion over evolving federal/state laws since COVID-19 waivers.
4. Clinical & Privacy Concerns
- Harder for providers to build trust, monitor withdrawal symptoms, or check for medication diversion virtually.
- Risk of breaches of confidentiality if patients can’t find a safe, private place for visits.
- Reduced ability to perform physical exams or urgent interventions.
5. Social & Personal Barriers
- Stigma: Fear of being judged by family, pharmacists, or even providers discourages use of telehealth.
- Unstable housing or unsafe environments: Individuals experiencing homelessness or domestic violence may struggle to engage in telemedicine.
- Distrust of technology: Some patients feel uncomfortable with virtual communication or worry about surveillance.
In summary, Telemedicine can expand access, but for people with addiction, barriers like stigma, unstable housing, limited technology, unclear policies, and pharmacy restrictions often prevent them from fully benefiting from this care model.
Conclusion
While telemedicine has opened critical pathways for opioid use disorder (OUD) treatment, persistent barriers—ranging from technology limitations to pharmacy hesitancy—continue to hinder its effectiveness. Addressing these challenges requires coordinated solutions, including better pharmacist training, improved communication between providers and pharmacies, and stronger patient support systems. Government interventions, through regulatory reforms, expanded funding, and insurance coverage, further reinforce these efforts by reducing structural and financial obstacles. By aligning pharmacy practices, healthcare providers, and policy initiatives, telemedicine can more effectively deliver life-saving OUD care and help close treatment gaps in communities most affected by the opioid crisis.
Video: 5 Surprising Ways Telemedicine Helps Recovery