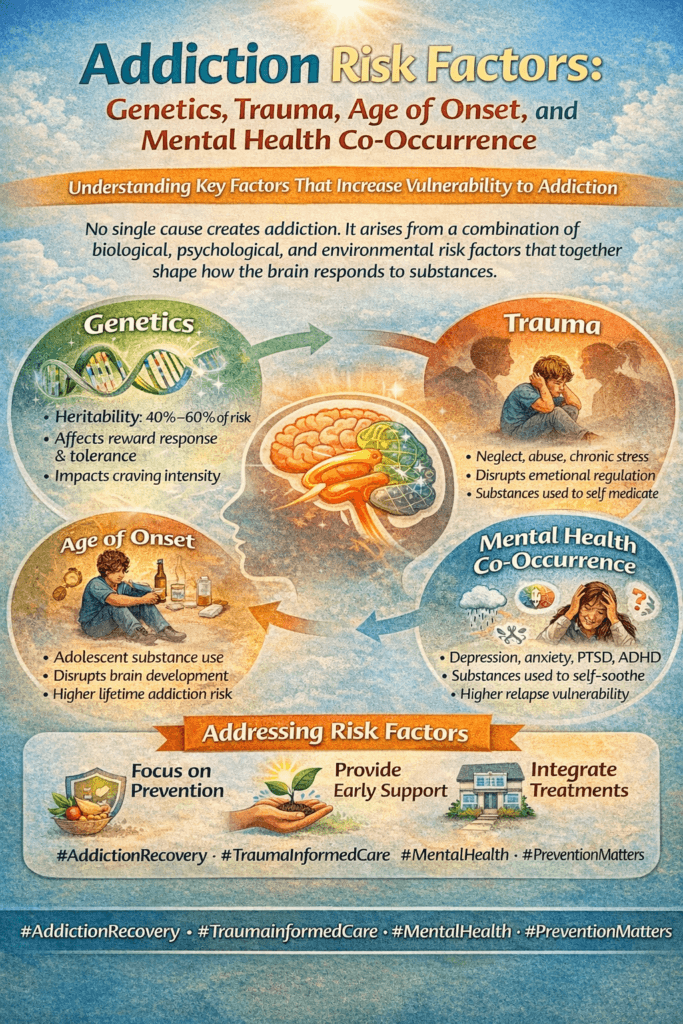
Addiction isn’t some random twist of fate. Plenty of research shows that certain risk factors make some people more likely to develop a substance use disorder. Genetics, experiences like childhood trauma, how early someone starts using a substance, and even co-occurring mental health issues all play a big part. Understanding these factors is really important if you’re hoping to prevent addiction or just trying to make sense of your own or a loved one’s struggles. Here’s a look at the main risk factors and what they might mean for you.
Genetic Risk Factors for Addiction
Plenty of people wonder, “Is addiction hereditary?” There’s a good reason for that. Studies have shown that genes can influence how the brain responds to substances like alcohol, nicotine, or opioids. If you have a parent or close blood relative who struggles with addiction, there’s a higher chance you might deal with similar issues yourself.
Genetics isn’t destiny, though. While research, like the studies from the National Institute on Drug Abuse, estimates inheritance might account for about 40-60% of the risk, there’s more to the story. Genes can raise your risk, but they usually interact with your environment and life experiences.
- Family History: If addiction runs in your family, it’s worth being extra aware of your own habits. Early prevention and support become really important here.
- How Genetics Influence Substance Response: Some people actually respond differently to substances at the biological level. For example, feeling less of an effect from alcohol can lead to drinking more for the same buzz.
- Epigenetics: This is a newer area of study showing how trauma and experiences can even change how your genes work, potentially passing risk down to future generations.
Having a genetic predisposition isn’t a guarantee you’ll develop an addiction. It just means you may need to watch your habits more closely and pay attention to early warning signs.
How Trauma Raises Addiction Risk
Experiencing trauma, especially as a young person, has a huge impact on addiction risk. Trauma can include physical, emotional, or sexual abuse, neglect, losing a parent, or growing up in a household with violence or unstable caregivers. All of these can raise the chances of misusing drugs or alcohol later in life.
What happens is, trauma can affect how the brain develops. It can increase stress, anxiety, and even change how someone handles emotions. Substances sometimes feel like a shortcut to relief, and, at least temporarily, they can numb pain, dull anxiety, or help someone fit in or escape. This is called self-medication.
- Adverse Childhood Experiences (ACEs): The more negative experiences someone has growing up, the higher their chance of developing an addiction as an adult. This is well documented in ACEs studies.
- Coping Mechanisms: If nobody taught healthy ways to deal with stress or emotions, drugs and alcohol can easily fill that gap. Learning better coping skills can make a real difference, which is why therapy is so often recommended.
Trauma is a risk factor that people can’t always control. Recognizing the impact of trauma is the first step toward finding healthier ways to heal and cope.
The Effect of Age of Onset on Addiction
The age when someone starts using alcohol, nicotine, or other drugs plays a big part in addiction risk. Early use, meaning during the teen years or even younger, can set the stage for bigger problems later.
The teenage brain is still developing, especially in areas that control self-discipline, planning, and impulse control. Substances can mess with this process, making young users more likely to develop both dependence and full-blown addiction.
- Earlier Start, Higher Risk: People who start drinking, smoking, or using drugs regularly before age 18 are much more likely to develop substance use disorders as adults.
- Brain Development: Because the brain doesn’t fully mature until the mid-20s, exposure to substances during this time disrupts the brain’s natural wiring.
- Peer Pressure: Teens are naturally drawn to risk-taking and to fitting in, which can heighten vulnerability during these years.
This is a big reason schools, parents, and communities work hard on prevention programs that delay the first use of substances. The later someone starts, the lower their risk.
Mental Health Disorders and Addiction (Co-Occurrence)
Mental health and substance use often go hand in hand. When someone has both a mental health disorder (like depression, anxiety, PTSD, or bipolar disorder) and a substance use disorder, it’s called a dual diagnosis or co-occurring disorder.
It’s not always clear which comes first, the mental health issue or the addiction, but they often feed off each other. Someone struggling with anxiety might drink to feel less tense; someone with depression may use stimulants to perk up. Over time, substance use can make the mental health issue worse, creating a complicated cycle.
- Depression and Anxiety: Treating only one part of the issue usually doesn’t work. Recovery goes much better with support for both mental health and substance use.
- Self-Medication: Turning to substances as a way to “fix” mood or stress can backfire, leading to dependence or addiction.
- Access to Treatment: Proper diagnosis and coordinated care for both conditions can be a game-changer. Integrated dual diagnosis treatment programs are proven to be more effective than treating each problem separately.
Support from trained professionals, therapy, and safe social circles makes a real difference for anyone dealing with both addiction and mental health challenges.
Common Challenges When Addressing Addiction Risk Factors
Knowing about risk factors is great, but actually facing them is another story. People often struggle with stigma, limited access to care, and not knowing where to start. Sometimes, families might even ignore warning signs because they hope the problem will solve itself.
- Stigma: People might avoid getting help because they feel ashamed or worry about being judged. This adds another barrier to recovery.
- Limited Resources: Access to good mental health or substance use services can be tough, especially in rural areas or for people without insurance.
- Family Dynamics: Sometimes families don’t want to admit a problem exists, making it harder for someone to reach out for help.
Being open to honest talks about addiction, reducing shame, and connecting to trustworthy resources can make real progress possible. Plus, it helps to remember that seeking help is a sign of strength—not weakness—so don’t hesitate to check in with support if things get tough.
Why Addressing Risk Factors Early Helps
Catching risk factors before they turn into serious problems can change lives. For example, early intervention in schools or routine mental health screenings at the doctor’s office can catch warning signs that might otherwise be missed.
- Education: Sharing facts reduces fear and misinformation. Teaching kids and teens both the risks and the reality is proven to help prevent early use.
- Better Support Systems: Building strong family ties and safe community spaces provides healthier ways for people to handle stress and tough times.
Getting ahead of the risk factors with real info and support makes prevention more doable than most people think. Empowering people with knowledge boosts their confidence to act on their own behalf or for their loved ones.
Actionable Steps for Lowering Your Own or a Loved One’s Addiction Risk
If you know you’ve got one or more risk factors, it isn’t something to panic over. It’s just a good reason to pay extra attention. There are plenty of things you or your family can do to reduce the risk and encourage healthy habits.
- Learn Your Family History: Ask about addiction or mental health struggles in your extended family. Knowing the history helps you spot risk sooner.
- Reach Out for Help Early: If stress, trauma, or persistent low mood feels overwhelming, connect with a counselor, doctor, or mental health support line sooner rather than later.
- Create a Supportive Environment: Surround yourself with friends and family who encourage healthy choices and support your mental well-being. Positive influences can go a long way.
- Limit Access and Temptation: Especially with teens, keeping alcohol or prescription medication locked up and being clear about boundaries works better than you might expect.
- Practice Coping Skills: Learn and practice healthy ways to manage stress, including exercise, mindfulness, journaling, and creative outlets. Even regular walks can make a difference.
Taking these steps doesn’t guarantee immunity from addiction, but they can tip the odds in a healthier direction. Open communication and ongoing support are key to prevention and real change.
Frequently Asked Questions About Addiction Risk Factors
Here are some questions people ask all the time about addiction risk:
Question: Can someone with no family history still develop addiction?
Answer: Absolutely. Environment, trauma, and mental health can all play a major role, even for people without a family history of addiction.
Question: Is addiction always about “bad choices”?
Answer: Not at all. Addiction is usually a mix of biology, environment, life experiences, and mental health. Having risk factors doesn’t mean someone is weak or making bad decisions.
Question: Can someone ever “age out” of high addiction risk?
Answer: Getting older does lower some risks, since the brain matures over time. But genetics and mental health issues can still play a part at any age.
Wrapping Up
The risk factors for addiction highlight how complex and personal this topic is. From your genes to your experiences, the influences stack up differently for everyone. Knowing about these risks is really helpful because it lets you make better choices, look out for yourself and your loved ones, and seek help sooner when needed. If you’re interested in more super-detailed info about addiction risk and prevention, SAMHSA and the National Institute on Drug Abuse have lots of easy-to-read resources with science-backed advice.
Video: This is How Addiction Actually Happens #BrainScience #RecoveryMatters