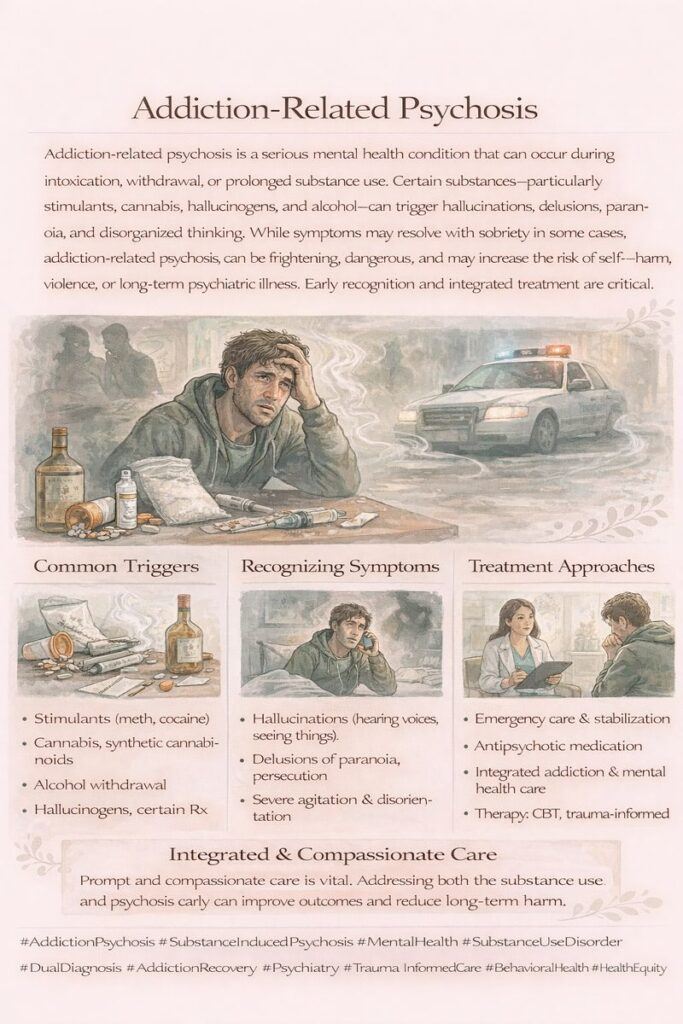
Addiction psychosis is a severe mental health condition arising from prolonged substance abuse, especially with drugs that have intense psychoactive effects. This condition is marked by a profound loss of contact with reality, manifesting in symptoms like hallucinations, delusions, paranoia, and disorganized thinking. It can occur during active substance use, during withdrawal, or even after the substance has been discontinued.
“Understanding Addiction Psychosis: Causes, Symptoms, and Management”
Addiction psychosis is a severe mental health condition typically associated with the abuse of certain substances, such as stimulants like cocaine and methamphetamine, hallucinogens like LSD and PCP, synthetic cannabinoids, and severe alcohol withdrawal scenarios like delirium tremens. Understanding the nature of addiction psychosis, its symptoms, and the necessary management strategies is essential for providing adequate care to affected individuals.
What is Addiction Psychosis?
Addiction psychosis refers to a state of altered mental functioning that arises in the context of substance abuse. Individuals experiencing this condition may encounter vivid and distressing hallucinations, which can involve seeing, hearing, or feeling things that aren’t there. Additionally, they may hold firmly to false beliefs or delusions that can distort their perception of reality.
Common Substances Linked to Addiction Psychosis
Certain substances are more commonly linked to the onset of addiction psychosis:
- Stimulants: Drugs like cocaine and methamphetamine can lead to intense paranoia and hallucinations, mainly when used in high doses or over prolonged periods.
- Hallucinogens: Substances such as LSD and PCP are notorious for causing perceptual distortions and altered realities, which can trigger psychotic symptoms.
- Synthetic Cannabinoids: Often marketed as “spice” or “K2,” these substances can produce unpredictable effects, including severe psychotic reactions.
- Alcohol: Severe alcohol withdrawal, particularly delirium tremens, can induce hallucinations and agitation, mimicking psychosis.
Symptoms of Addiction Psychosis
Individuals affected by addiction psychosis may exhibit a range of symptoms, including:
- Hallucinations: Experiencing vivid, often distressing sensory perceptions.
- Delusions: Firmly held false beliefs, such as the belief that others are plotting against them.
- Intense Paranoia: Heightened feelings of mistrust or suspicion towards others, which can lead to aggressive or violent behavior.
- Disorganized Thinking: Difficulty organizing thoughts, leading to incoherent speech or an inability to communicate effectively.
The Impact of Prolonged Substance Abuse
While some cases of addiction psychosis may resolve after the substance has cleared from the body, prolonged substance abuse can lead to persistent psychotic symptoms. These symptoms can resemble primary psychotic disorders, such as schizophrenia, necessitating a comprehensive psychiatric evaluation and treatment.
Management of Addiction Psychosis
Effective management of addiction psychosis generally requires a multifaceted approach that includes:
- Detoxification: Safely removing the substance from the body under medical supervision to manage withdrawal symptoms and stabilize the individual.
- Psychiatric Care: Comprehensive evaluation by mental health professionals to assess the severity of psychosis and develop an appropriate treatment plan.
- Long-Term Addiction Treatment: Engaging in structured addiction treatment programs to address the underlying substance use disorder.
- Antipsychotic Medications: Prescribing antipsychotic medications can help alleviate symptoms of psychosis and stabilize mood.
- Therapy: Incorporating therapeutic interventions, such as cognitive-behavioral therapy (CBT), to address thought patterns and behaviors associated with addiction and psychosis.
Risk Factors for Addiction Psychosis
Specific individuals are at a heightened risk for developing addiction psychosis, including those with:
- A history of mental illness.
- Heavy substance use or polysubstance abuse.
- A family history of psychiatric disorders.
Understanding addiction psychosis is crucial for effective intervention and support. By recognizing the signs and symptoms associated with this condition, healthcare providers can implement targeted strategies to manage and treat individuals affected by substance use disorders. Comprehensive care that includes detoxification, psychiatric evaluation, medication management, and ongoing support is essential for promoting recovery and preventing the recurrence of psychotic symptoms. As awareness of addiction psychosis grows, we can foster a more informed approach to addressing the complexities of addiction and its impact on mental health.
“Understanding the Factors that Elevate the Risk of Addiction Psychosis”
Addiction psychosis is a serious mental health issue that can arise from substance abuse, particularly among individuals with certain underlying health conditions. Understanding these contributing factors is crucial for preventing and managing addiction psychosis effectively. Several health conditions can exacerbate the risk of developing this complex disorder.
Pre-existing Mental Health Disorders
Individuals with pre-existing mental health disorders are at a significantly heightened risk for addiction psychosis. Conditions such as:
- Schizophrenia: Substance abuse can worsen the symptoms of schizophrenia, potentially triggering episodes of psychosis.
- Bipolar Disorder: The use of drugs or alcohol can destabilize mood and increase the risk of manic or depressive episodes, leading to psychotic symptoms.
- Major Depressive Disorder: Substance use can exacerbate depressive symptoms, potentially leading to hallucinations or delusions.
Personality Disorders
Personality disorders can also contribute to impulsive behaviors that elevate the risk of psychosis. Notable examples include:
- Borderline Personality Disorder (BPD): Individuals with BPD may engage in substance abuse as a means of coping with emotional distress, increasing their risk for addiction psychosis.
- Antisocial Personality Disorder: Impulsive behavior and disregard for consequences can lead to risky substance use, heightening the likelihood of developing psychotic symptoms.
Neurological Conditions
Certain neurological conditions can complicate the risk of addiction psychosis. For instance:
- Epilepsy: Individuals with epilepsy may experience psychotic symptoms during or after seizures, and substance abuse can trigger more severe episodes.
- Traumatic Brain Injury (TBI): A history of TBI can impact cognitive function and emotional regulation, increasing susceptibility to addiction and psychosis.
Genetic Predispositions
Genetic factors play a crucial role in determining an individual’s risk for both addiction and psychosis. A family history of mental illness can indicate a higher likelihood of developing similar disorders, especially when coupled with substance abuse.
Chronic Stress and Trauma
Chronic stress and traumatic experiences can significantly impact mental health. Conditions such as:
- Post-Traumatic Stress Disorder (PTSD): Individuals with PTSD may turn to substances as a form of self-medication, which can trigger or worsen psychotic symptoms.
- Chronic Stress: Prolonged exposure to stress can impair mental resilience and contribute to the onset of addiction psychosis.
Sleep Disorders
Sleep disorders, such as chronic insomnia, can further elevate the risk of developing addiction psychosis. Lack of sleep negatively affects cognitive function and emotional stability, making individuals more vulnerable to the effects of substance abuse.
Polysubstance Abuse
Engaging in polysubstance abuse or the use of multiple drugs simultaneously compounds the risk of addiction psychosis. The interaction between various substances can create unpredictable effects on the brain, leading to heightened chances of developing psychotic symptoms.
The relationship between underlying health conditions and addiction psychosis is complex and multifaceted. Individuals with pre-existing mental health disorders, personality disorders, neurological conditions, genetic predispositions, chronic stress, trauma, sleep disorders, and those engaging in polysubstance abuse are at a higher risk for developing this debilitating condition.
Understanding these risk factors can help healthcare professionals identify vulnerable individuals and implement targeted prevention and treatment strategies. By addressing these underlying issues, we can foster a more comprehensive approach to managing addiction psychosis and promote recovery for those affected. Awareness and education about the links between these health conditions and addiction psychosis are vital steps toward improving outcomes and reducing the stigma associated with these intertwined challenges.
“Proactive Strategies for Preventing Addiction Psychosis”
Preventing addiction psychosis requires a proactive and comprehensive approach that prioritizes mental health and well-being. Individuals can significantly reduce their risk of developing this serious condition by implementing key self-management strategies. Here are some essential steps to consider
1. Limit or Avoid Substance Use
The first line of defense against addiction psychosis is to avoid or limit the use of substances known to trigger psychotic symptoms. This includes stimulants like cocaine and methamphetamine, as well as hallucinogens such as LSD and PCP. For individuals in recovery or at risk, steering clear of these substances is crucial.
2. Seek Early Treatment for Mental Health Issues
Addressing mental health issues promptly can mitigate the risk of addiction psychosis. Individuals experiencing symptoms of anxiety, depression, or any other mental health disorder should seek professional help as early as possible. Early intervention can provide the necessary support and resources to manage symptoms effectively.
3. Build Healthy Coping Mechanisms
Developing healthy coping strategies is vital for managing stress and emotional challenges. Mindfulness, meditation, or yoga can enhance emotional regulation and resilience. Additionally, hobbies and activities that bring joy can serve as positive outlets for stress.
4. Educate Yourself About Risks
Understanding the risks associated with substance use is essential for making informed decisions. Education can empower individuals to recognize the potential consequences of substance abuse and encourage healthier lifestyle choices.
5. Strengthen Social Support Networks
Having a robust support network can make a significant difference in preventing addiction psychosis. Connecting with friends, family, or support groups provides emotional support and accountability. Engaging with others who understand the challenges of addiction can foster a sense of belonging and reduce feelings of isolation.
6. Avoid High-Risk Situations
Being mindful of environments and situations that may trigger substance use or stress is crucial. Avoiding high-risk settings, such as parties or gatherings where drug use is prevalent, can help reduce exposure to temptation and potential relapse.
7. Regular Monitoring of Mental Health
Ongoing mental health monitoring is essential for early identification of any changes or concerns. Regular check-ins with a mental health professional can help track progress and address any emerging issues promptly.
8. Adhere to Prescribed Medications
For those on medication for mental health conditions, adhering to prescribed treatment plans is essential. Consistent medication management can stabilize mood and reduce the risk of psychotic symptoms.
9. Engage in Healthy Hobbies and Activities
Participation in healthy hobbies, such as sports, art, or music, can provide a constructive outlet for emotions and reduce the likelihood of turning to substances for relief. Finding fulfillment in productive activities can boost self-esteem and overall well-being.
10. Maintain Physical Health
Physical health plays a crucial role in mental well-being. Regular exercise and a balanced diet can improve mood, enhance energy levels, and reduce stress. Prioritizing physical health contributes to a more resilient mindset and decreases vulnerability to addiction psychosis.
11. Seek Early Professional Help
For individuals identified as high-risk, seeking professional help early can prevent the escalation of conditions leading to addiction psychosis. Mental health professionals can provide tailored support, resources, and coping strategies to navigate challenges effectively.
Preventing addiction psychosis involves a multi-faceted approach that emphasizes self-management, education, and support. By taking proactive steps to limit substance use, seek early treatment, and develop healthy coping mechanisms, individuals can significantly reduce their risk of developing this serious condition. Building strong support networks, adhering to treatment plans, and maintaining physical health are essential to prevention.
Awareness of the factors contributing to addiction psychosis empowers individuals to make informed decisions about their health and well-being, fostering a proactive stance against the challenges of substance use and mental health. These strategies create a solid foundation for a healthier and more resilient future.
“The Crucial Role of Family Support in Preventing Addiction Psychosis”
Family support is an indispensable element in preventing addiction psychosis, playing a vital role in the mental and emotional well-being of individuals at risk. A supportive family environment can significantly influence recovery outcomes and help mitigate the risk of developing psychotic symptoms associated with substance abuse. Here are effective strategies for families to support their loved ones.
1. Foster Open Communication
Encouraging open dialogue within the family creates a safe space for discussing feelings, challenges, and concerns. By fostering an atmosphere where everyone feels heard, family members can better understand each other’s experiences and provide support when needed. Active listening and expressing empathy can strengthen bonds and promote a culture of openness.
2. Provide Emotional Support
Emotional support is crucial for individuals struggling with addiction or mental health issues. Family members should reassure their loved ones that they are not alone and that their feelings are valid. Offering encouragement during tough times and celebrating successes, no matter how small, can boost morale and resilience.
3. Monitor Mental Health for Early Signs
Keeping an eye on mental health is essential for early intervention. Family members should be aware of any changes in behavior, mood, or functioning that may signal the onset of mental health issues. By recognizing these signs early, families can encourage their loved ones to seek help before problems escalate.
4. Encourage Healthy Lifestyle Choices
Promoting healthy habits, such as regular exercise, a balanced diet, and sufficient sleep, can positively impact mental health. Families can engage in activities promoting well-being, such as cooking healthy meals, walking, or participating in group sports.
5. Set Clear Boundaries Regarding Substance Use
Establishing clear boundaries about substance use is crucial for creating a supportive environment. Families should communicate the importance of avoiding drugs and alcohol and discuss the potential consequences of substance abuse. Setting boundaries can help protect vulnerable family members from high-risk situations.
6. Create a Supportive, Substance-Free Environment
A substance-free home environment fosters safety and encourages recovery. Families can actively remove any drugs or alcohol from their homes and create spaces that promote positive activities, like reading, hobbies, or family games. This approach nurtures a supportive atmosphere that emphasizes health and well-being.
7. Educate Family Members About Addiction and Psychosis
Education is critical to understanding addiction and its effects. Family members should learn about the signs of addiction psychosis, the impact of substances, and the importance of treatment. This knowledge equips families to provide informed support and advocate for their loved ones effectively.
8. Support Treatment and Recovery Efforts
Encouraging participation in treatment programs and recovery efforts is vital. Families should support their loved ones in attending therapy sessions, support groups, or rehabilitation programs. Families can reinforce the importance of seeking help by showing commitment to recovery.
9. Spend Quality Time Together
Quality family time fosters solid relationships and a sense of belonging. Engaging in fun and meaningful activities can reduce stress and strengthen family bonds. These moments contribute to a supportive environment, whether it’s game nights, family outings, or simply spending time at home.
10. Seek External Support
Sometimes, external support can enhance family efforts. Seeking family counseling or joining support groups can provide additional resources and coping strategies for families dealing with addiction. These platforms offer a safe space to share experiences and learn from others facing similar challenges.
Family support is crucial in preventing addiction psychosis and promoting recovery. By fostering open communication, providing emotional support, and creating a healthy and substance-free environment, families can significantly reduce the risk of addiction-related issues. Educating family members about the complexities of addiction and actively supporting treatment efforts can empower individuals to make healthier choices and seek help when needed.
Families can build a robust support system that fosters resilience, understanding, and healing, creating a foundation for lasting recovery and well-being. In this journey, the collective efforts of family members can make a meaningful difference in preventing addiction psychosis and supporting loved ones on the path to recovery.
“The Role of Community Resources in Preventing Addiction Psychosis”
Community resources are instrumental in preventing addiction psychosis by providing education, support, and access to vital services. A collaborative effort between individuals, families, and local organizations can foster an environment that promotes mental health and well-being. Here are several ways community resources can play a significant role in prevention.
1. Community Education Events
Participating in community education events is essential for raising awareness about the risks of substance abuse and the potential for addiction psychosis. Workshops, seminars, and informational sessions can equip individuals with knowledge about the signs of addiction and psychosis, effective coping strategies, and the importance of seeking help. These events can also provide a platform for experts to share insights and foster discussions around mental health.
2. Local Support Groups
Accessing local support groups is crucial for individuals struggling with addiction or mental health issues. These groups offer a safe space for sharing experiences, receiving encouragement, and building connections with others facing similar challenges. Support groups can provide invaluable emotional support and practical advice, enhancing resilience and promoting recovery.
3. Mental Health Services
Engaging with local mental health services is vital for early intervention and effective treatment. Community mental health clinics can offer therapy, counseling, and medication management, addressing both addiction and underlying psychological issues. Access to these services can help individuals develop coping skills and strategies for managing stress and reducing the risk of psychosis.
4. Collaborating with Healthcare Providers
Community collaboration with local healthcare providers ensures a holistic approach to prevention. Healthcare professionals can offer screenings, assessments, and resources for individuals at risk of addiction psychosis. Community organizations and healthcare providers can work together to create tailored programs that address specific community needs.
5. Promoting Healthy Lifestyles
Promoting healthy lifestyles through community programs is essential in preventing addiction psychosis. Initiatives such as exercise classes, nutrition workshops, and wellness programs can encourage individuals to adopt healthier habits. Communities prioritizing physical and mental health create an environment conducive to well-being.
6. Leveraging Faith-Based Resources
Faith-based organizations often provide valuable support and resources for individuals struggling with addiction and mental health issues. These groups can offer spiritual guidance, counseling, and community support, fostering a sense of belonging and purpose. Collaborating with faith-based organizations can expand the reach of prevention efforts.
7. Advocating for Policy and Community Changes
Advocating for policy and community changes is crucial for creating an environment that supports mental health and addiction recovery. By engaging with local leaders and policymakers, community members can push for improved access to treatment services, harm reduction initiatives, and prevention resources. Collective advocacy can lead to meaningful changes in how addiction and mental health are addressed.
8. Utilizing Public Health Resources
Public health resources provide essential information and services for preventing addiction psychosis. Community health departments can offer educational materials, screening programs, and referrals to treatment services. Leveraging these resources can enhance community efforts to combat addiction and promote mental wellness.
9. Building Strong Social Networks
Strong social networks are vital for prevention and recovery. Engaging with neighbors, friends, and community members fosters a sense of connection and support. Social networks can provide encouragement, accountability, and a platform for sharing resources, making it easier for individuals to seek help when needed.
10. Online and Telehealth Resources
In an increasingly digital world, utilizing online and telehealth resources can significantly enhance access to support and treatment. Virtual support groups, online therapy sessions, and educational webinars can reach individuals facing barriers to in-person services. Telehealth options expand the availability of mental health services, making it easier for individuals to access help from the comfort of their homes.
Community resources play a vital role in preventing addiction psychosis by providing education, support, and essential services. By actively engaging with local organizations, participating in education events, and accessing mental health services, individuals can build a strong foundation for prevention and early intervention. Collaborating with healthcare providers, promoting healthy lifestyles, and advocating for policy changes create a supportive environment that fosters recovery and mental well-being.
Together, communities can empower individuals to seek help, reduce the stigma surrounding addiction and mental health, and ultimately prevent the onset of addiction psychosis. We can create a healthier, more informed society that prioritizes mental health and recovery through a comprehensive approach that leverages community resources.
Frequently Asked Questions
Here are some common questions:
Which substances most commonly cause psychosis?
Stimulants such as methamphetamine and cocaine are most strongly associated, but alcohol, cannabis (especially high-THC products), hallucinogens, synthetic drugs, and some prescription medications can also trigger psychosis.
Can psychosis happen during withdrawal?
Yes. Psychosis can occur during withdrawal, particularly with alcohol or sedative withdrawal, and may include hallucinations, agitation, and confusion.
How is addiction psychosis different from schizophrenia?
Addiction psychosis is directly linked to substance use and often improves with sobriety. Schizophrenia is a primary psychiatric disorder that persists independent of substance use, though substances can worsen symptoms.
Can addiction psychosis happen without a prior mental illness?
Yes. Many people experience substance-induced psychosis without any previous psychiatric diagnosis.
Are the hallucinations and delusions real to the person?
Yes. The experiences feel completely real and can be frightening or distressing, even if they are not based in reality.
Is addiction-related psychosis dangerous?
It can be. Psychosis increases the risk of self-harm, accidental injury, aggression, overdose, and involvement with emergency services.
Does addiction psychosis go away on its own?
Sometimes. Symptoms may resolve once the substance leaves the body, but in some cases, psychosis persists and requires ongoing treatment.
Can addiction psychosis become permanent?
Repeated episodes or prolonged substance use may increase the risk of developing chronic psychotic disorders in vulnerable individuals.
How is addiction psychosis treated in the short term?
Treatment focuses on safety and stabilization, which may include hospitalization, antipsychotic medications, sedation, hydration, and supportive care.
What is long-term treatment for addiction psychosis?
Long-term care includes treating the substance use disorder, managing psychotic symptoms, therapy, trauma-informed care, and relapse prevention strategies.
Conclusion
Addressing addiction psychosis requires a comprehensive approach that integrates self-management strategies, family support, and community resources. By implementing these measures, individuals can significantly reduce the risk of addiction psychosis and foster long-term mental health and recovery.