Understanding the brain mechanism of addiction is critical to developing effective treatments by the brain’s reward systems and neurotransmitter pathways. Medications and psychological therapies target these mechanisms: medications alter receptor activity and neurotransmitter levels, while therapies address cognitive and emotional processes. Despite their benefits, these treatments have disadvantages, including variable effectiveness, side effects, and high costs. Ethical dilemmas such as ensuring informed consent, protecting privacy, and avoiding stigmatization also arise. A balanced approach is needed to address these issues while effectively treating addiction.
Understanding the Brain Mechanisms Behind Opioid Addiction
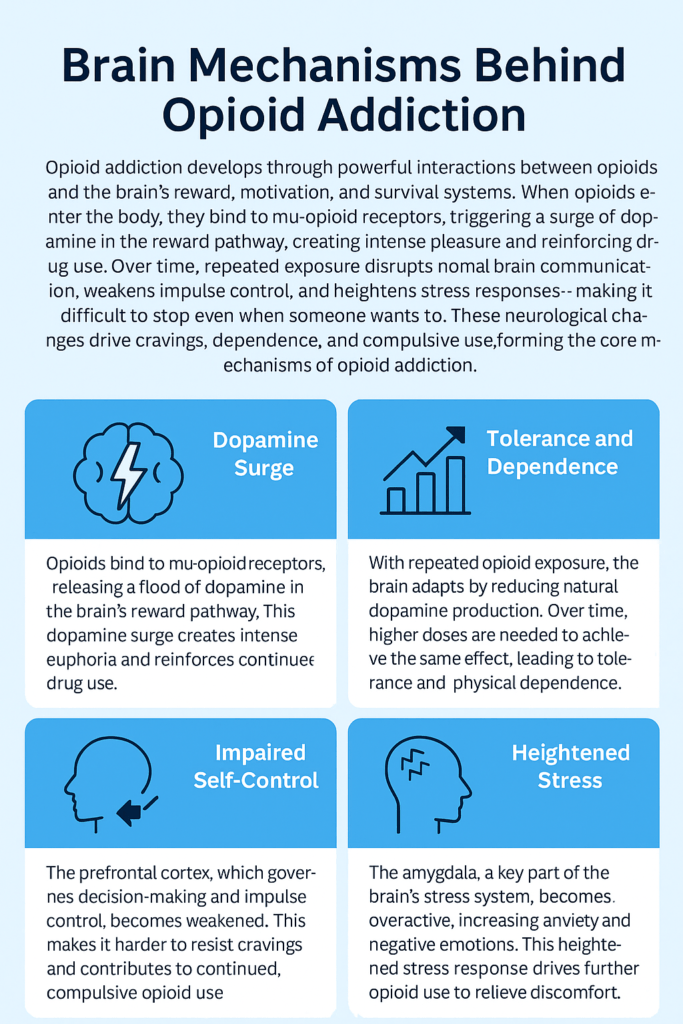
Opioid addiction is a complex and devastating condition that involves intricate changes in the brain’s reward system, neurotransmitters, and neural circuits. To help make sense of this, here’s a simplified overview of the core mechanisms behind opioid addiction:
1. Opioid Receptor Activation
Receptor Types: Opioids exert their effects primarily through three types of receptors: mu (μ), delta (δ), and kappa (κ). The mu-opioid receptors are the main targets of most opioid drugs.
Mechanism: When opioids bind to mu-opioid receptors, they trigger a series of biochemical changes. This leads to the inhibition of neurotransmitters such as gamma-aminobutyric acid (GABA), which usually prevents dopamine release.
2. Dopamine Release
Reward Pathway: Opioid activation reduces GABA inhibition, causing an increase in dopamine release in the brain’s reward system, particularly in the nucleus accumbens.
Euphoria: This surge of dopamine is responsible for the feelings of euphoria and pleasure that accompany opioid use, reinforcing the behavior of taking the drug.
3. Neuroadaptation
Tolerance: Over time, with repeated opioid use, the brain begins to adapt. Its response to opioids weakens, leading to the development of tolerance. This means that larger doses are required to experience the same effects.
Dependence: As the brain adjusts to the regular presence of opioids, it becomes physically dependent. When opioid use is reduced or stopped, withdrawal symptoms emerge, reflecting the brain’s reliance on the drug.
4. Brain Circuitry Changes
Altered Reward System: Chronic opioid use alters the brain’s reward system, making everyday pleasures like food or socializing less satisfying compared to the high induced by opioids.
Prefrontal Cortex Impact: The prefrontal cortex, responsible for decision-making and impulse control, is often impaired in individuals with opioid addiction. This makes it harder to make rational decisions about drug use, leading to continued use despite negative consequences.
5. Emotional and Cognitive Effects
Mood Regulation: Opioids affect brain regions involved in mood regulation and stress response. This can lead to emotional instability, where individuals use opioids as a way to cope with negative feelings.
Cognitive Impact: Long-term opioid use can impair cognitive functions such as memory and executive control, making the addiction and recovery process even more challenging.
Opioid addiction is driven by the interplay between receptor activation, altered reward systems, neuroadaptive changes, and brain circuit disruptions. These chemical changes involve significant cognitive and emotional effects, making recovery highly intricate. Understanding these mechanisms is crucial for both treatment strategies and empathy toward those affected by addiction.
How Medications for Opioid Use Disorder (OUD) Impact Brain Mechanisms
Medications used to treat Opioid Use Disorder (OUD) play a crucial role in altering the brain mechanisms involved in addiction. These treatments aim to restore balance to neurotransmitter systems and reduce the compulsive behaviors associated with opioid use. Here’s a breakdown of how these medications impact the brain and support recovery:
1. Partial Agonists (e.g., Buprenorphine)
Receptor Binding: Buprenorphine is a partial agonist at mu-opioid receptors, which means it activates these receptors but to a lesser degree than full agonists like heroin or morphine.
Reduced Euphoria: By partially stimulating mu-opioid receptors, buprenorphine helps reduce cravings and withdrawal symptoms without producing the intense euphoria associated with full opioids.
Ceiling Effect: Buprenorphine has a ceiling effect, meaning it limits the intensity of its opioid effects, reducing the risk of overdose and lowering the potential for misuse.
2. Full Agonists (e.g., Methadone)
Sustained Agonism: Methadone is a full agonist at mu-opioid receptors, providing a steady level of activation that alleviates withdrawal symptoms and cravings.
Balanced Effects: By maintaining consistent receptor activation, Methadone helps stabilize brain chemistry, reducing the compulsive need to seek and use opioids.
Controlled Dosing: Methadone’s long half-life ensures steady opioid activity, which helps prevent the highs and lows that fuel addiction, improving overall stability.
3. Antagonists (e.g., Naltrexone)
Blocking Receptors: Naltrexone is an opioid antagonist that blocks mu-opioid receptors, preventing opioids from binding and exerting their effects.
Prevention of Reinforcement: By blocking the rewarding effects of opioids, Naltrexone reduces the reinforcement of drug-seeking behavior, helping individuals maintain abstinence.
Reduction in Cravings: Naltrexone can also diminish cravings by removing the euphoric effects associated with opioid use, thus supporting recovery.
4. Combination Medications (e.g., Suboxone)
Mixed Effects: Suboxone combines buprenorphine and naloxone. Buprenorphine manages withdrawal symptoms, while naloxone, an opioid antagonist, is included to deter misuse.
Prevention of Misuse: Naloxone blocks the effects of opioids, reducing the risk of relapse by preventing the medication from being misused for its euphoric effects.
5. Neurochemical Balance
Restoration of Homeostasis: OUD medications help restore balance to neurotransmitter systems that have been disrupted by chronic opioid use. This stabilization improves mood, reduces cravings, and enhances cognitive functioning.
Reduction of Neuroplastic Changes: Long-term opioid use causes neuroplastic changes in the brain’s reward system. Medications can reduce this dysregulation, aiding in the normalization of brain function over time.
6. Behavioral and Cognitive Effects
Enhanced Functioning: Medications for OUD improve cognitive and emotional functioning, helping individuals make better decisions and counteract the impairment caused by opioid use.
Support for Therapy: By reducing withdrawal symptoms and cravings, these medications create a more stable mental state that supports active engagement in behavioral therapies and other recovery-oriented activities.
Medications for Opioid Use Disorder (OUD) modulate opioid receptors, stabilize neurotransmitter systems, and alter brain reward pathways, helping individuals manage cravings and restore balance in the brain. By addressing both the physical and psychological aspects of addiction, these treatments support long-term recovery and reduce the impact of opioid addiction on brain function.
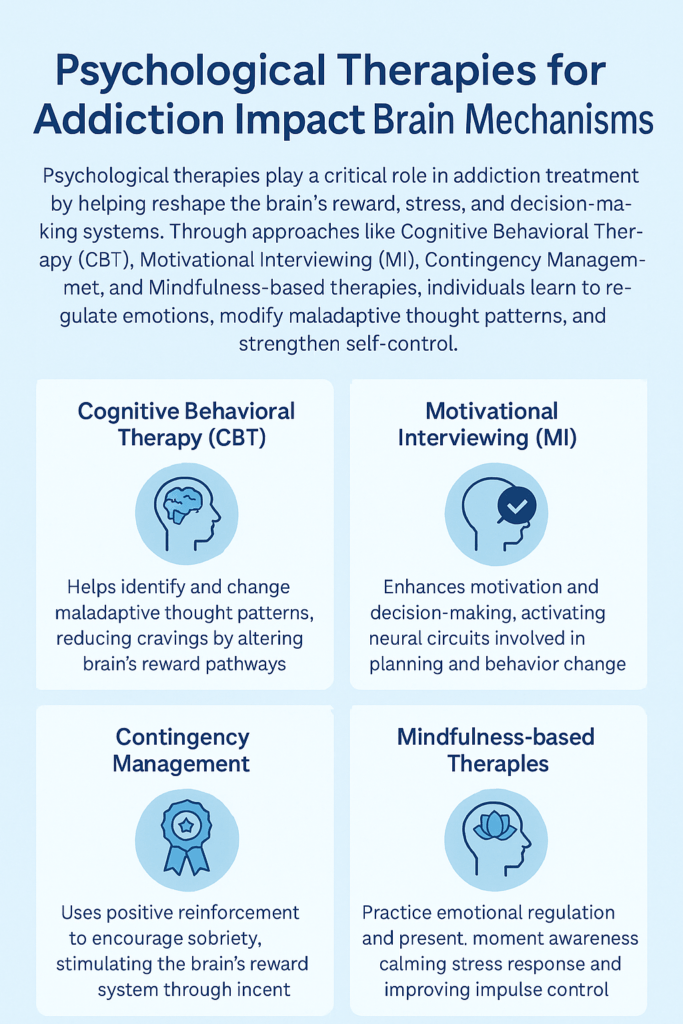
How Psychological Therapies for Addiction Impact Brain Mechanisms
Addiction treatment goes beyond medications—it involves psychological therapies that target the brain mechanisms behind addiction by addressing cognitive, emotional, and behavioral aspects. Here’s an overview of key therapies and how they work:
1. Cognitive Behavioral Therapy (CBT)
Focus: CBT helps individuals recognize and change harmful thought patterns and behaviors associated with addiction.
Mechanism: CBT addresses cognitive distortions and equips individuals with coping strategies to manage triggers and cravings. By changing how people think and react, CBT can reshape brain pathways related to addiction and reward.
2. Motivational Interviewing (MI)
Focus: MI is a client-centered approach designed to enhance motivation for change by resolving ambivalence and strengthening commitment to recovery.
Mechanism: MI enhances intrinsic motivation, influencing brain regions associated with decision-making and reward processing, helping individuals align their actions with recovery goals.
3. Contingency Management (CM)
Focus: CM uses positive reinforcement to encourage abstinence and adherence to treatment goals.
Mechanism: By offering tangible rewards for sobriety and other positive behaviors, CM helps retrain the brain’s reward system, reinforcing abstinence-related behaviors and reconditioning brain circuits involved in reward processing.
4. Mindfulness-Based Relapse Prevention (MBRP)
Focus: MBRP combines mindfulness meditation with relapse prevention techniques to manage cravings and stress.
Mechanism: Mindfulness alters brain activity associated with stress and impulse control, thereby improving emotional regulation. This reduces the risk of relapse by strengthening brain areas that manage emotional responses and decision-making.
5. Dialectical Behavior Therapy (DBT)
Focus: DBT focuses on developing skills in emotional regulation, distress tolerance, and effective interpersonal communication.
Mechanism: By teaching individuals how to manage intense emotions and cravings, DBT targets brain regions involved in emotion regulation and impulse control, making it easier to resist addictive behaviors.
Focus: ACT encourages acceptance of thoughts and feelings while committing to actions aligned with personal values.
Mechanism: ACT helps individuals change their relationship with cravings and negative thoughts. By doing so, it alters brain pathways related to self-control and reduces the influence of addiction-related brain circuits.
7. Family Therapy
Focus: Family therapy addresses relational issues within the family system and improves support for the individual in recovery.
Mechanism: Resolving family conflicts and improving communication can positively influence brain regions involved in the stress response and emotion regulation, creating a more supportive environment for recovery.
8. Group Therapy
Focus: Group therapy provides a setting for individuals to share experiences and learn from others in recovery.
Mechanism: Social support and shared experiences reduce feelings of isolation, reinforcing positive behavioral changes and activating brain regions involved in social connection and emotional regulation.
9. Trauma-Informed Therapy
Focus: Trauma-informed therapy addresses the impact of past trauma on addiction and the recovery process.
Mechanism: By processing trauma and developing healthy coping strategies, trauma-informed therapy helps regulate brain areas related to stress and emotional responses, which are often dysregulated in individuals with a history of trauma.
10. Biofeedback and Neurofeedback
Focus: These therapies use real-time data on physiological functions to help individuals learn to control bodily processes.
Mechanism: These therapies can influence stress-related brain activity by teaching individuals to regulate physiological responses and improve emotional and physical self-regulation.
Psychological therapies for addiction target the underlying cognitive, emotional, and behavioral aspects of the disorder. By retraining the brain’s reward pathways, improving emotional regulation, and enhancing coping strategies, these therapies support recovery and help rewire brain mechanisms disrupted by addiction.
These are the underlying cognitive, emotional, and behavioral factors contributing to addiction, ultimately helping to rewire brain mechanisms associated with addiction and recovery.
The Challenges of Treating Addiction Through Brain-Focused Approaches
Targeting the brain mechanisms behind addiction can be highly beneficial, but it also comes with several challenges. Addressing addiction through brain-focused treatments alone may not be enough for all individuals. Here are some key disadvantages to consider:
1. Complexity of Addiction
Multifaceted Nature: Addiction is driven by a combination of genetic, environmental, psychological, and neurological factors. While brain-targeted treatments address some key aspects, they may not fully resolve all contributing factors. Ignoring psychological and social components may leave underlying issues unaddressed, limiting the effectiveness of treatment.
2. Treatment Resistance
Variable Effectiveness: Not everyone responds to brain-focused treatments the same way. Some individuals may find that these treatments provide limited benefits or fail to address their specific needs and triggers, making treatment outcomes unpredictable.
3. Cost and Accessibility
Expense: Advanced treatments, such as neurofeedback or specific medication-based therapies, can be expensive and may not always be covered by insurance. The high cost creates a financial barrier for many individuals seeking help.
Availability: Access to specialized treatments targeting brain mechanisms is often limited, particularly in underserved or rural areas. This lack of availability can lead to disparities in treatment options and outcomes, making it harder for some to receive the care they need.
4. Potential Side Effects
Adverse Effects: Some brain-focused therapies, particularly medication-based interventions, come with side effects. These may range from mild discomfort to more severe health risks, requiring close monitoring and management by healthcare providers.
Overemphasis on Medication: Relying too heavily on medications or brain-based interventions can sometimes overshadow the importance of holistic care. Behavioral therapies, social support, and lifestyle changes are critical for long-term recovery but may be underutilized when the focus is primarily on brain mechanisms.
5. Stigma and Misunderstanding
Stigma: There can be stigma attached to brain-focused treatments, such as medication-assisted therapy, making some individuals hesitant to seek or adhere to these treatments. Fear of others’ judgment may prevent people from engaging with specific options.
Misunderstanding: Misconceptions about how addiction and brain treatments work can lead to confusion. People may not fully understand the goals and effectiveness of these interventions, potentially reducing their willingness to engage with or trust the treatment process.
6. Long-Term Efficacy
Sustainability: Brain-targeted treatments, while often effective in the short term, may not always offer long-lasting solutions. Long-term recovery typically requires continued support, integration of other therapeutic approaches, and lifestyle changes to maintain sobriety.
7. Ethical Considerations
Informed Consent: Ensuring individuals understand the risks and benefits of brain-focused treatments is essential. Gaining informed consent can be challenging, especially with more advanced interventions that involve complicated procedures or medications.
Privacy Concerns: Some treatments that involve monitoring brain activity or using data from neurological assessments may raise privacy and data security concerns. Protecting sensitive personal information related to an individual’s brain health is essential.
8. Integration with Other Therapies
Holistic Approach: Focusing solely on the brain’s role in addiction may lead to incomplete care. The emotional, behavioral, and social dimensions of addiction are crucial to address for successful recovery. Treatment programs that don’t integrate behavioral therapy or social support may fail to provide comprehensive care.
While targeting the brain mechanisms of addiction can be highly beneficial, it’s essential to recognize the limitations and potential drawbacks. A balanced approach that combines brain-focused treatments with behavioral, emotional, and social therapies offers a more holistic solution, ensuring individuals receive personalized and comprehensive care for their addiction.
Ethical Dilemmas in Treating the Brain Mechanisms of Addiction
While targeting the brain mechanisms of addiction can be effective, it introduces several ethical challenges. These dilemmas require careful consideration to balance patient care, autonomy, and broader social concerns. Here are the key ethical issues in treating addiction through brain-focused interventions:
1. Informed Consent
Complexity: Addiction treatments that focus on brain mechanisms can be complex for patients to understand fully. Ensuring that individuals grasp the nature of these treatments, including their risks and benefits, presents a significant ethical challenge.
Capacity: Addiction can impair cognitive function, making it harder for individuals to give informed consent. Healthcare providers must carefully assess whether a patient can make an informed decision about their treatment.
2. Privacy and Confidentiality
Sensitive Data: Brain-focused treatments, such as neurofeedback and brain imaging, generate susceptible neurological data. Ensuring this data remains private and secure is essential, as breaches of confidentiality can have severe consequences for patients, including discrimination or stigma.
3. Coercion and Autonomy
Coercion: In some cases, individuals may feel coerced into brain-based treatments, especially when treatment is mandated or strongly encouraged in legal settings, such as within the criminal justice system. This raises ethical questions about whether consent is genuinely voluntary.
Autonomy: Balancing treatment effectiveness with respect for an individual’s autonomy is crucial. Ensuring patients have the freedom to choose or refuse treatment, even in cases of addiction, is an ongoing ethical challenge.
4. Equity and Access
Disparities: Brain-based treatments can be expensive and inaccessible to many individuals, especially those from underserved communities. This creates disparities in access to these advanced treatments and raises ethical concerns about fairness in healthcare.
Resource Allocation: There are also ethical questions about the allocation of healthcare resources. Should expensive brain-focused treatments be prioritized over more traditional, less costly interventions that could benefit a broader population?
5. Potential for Stigmatization
Labeling: Focusing heavily on the brain mechanisms behind addiction may inadvertently reinforce the stigma that addiction is purely a biological disorder. This can lead to neglecting the psychological, social, and environmental factors that contribute to addiction.
Social Implications: The emphasis on neurological explanations for addiction might influence societal attitudes and policies, potentially leading to approaches that lack empathy and understanding of addiction’s broader complexities.
6. Long-Term Effects and Safety
Unknown Long-Term Effects: Some brain-based treatments, especially newer or more experimental ones, may carry unknown risks and long-term consequences. Ensuring these treatments are safe and effective over time is a critical ethical responsibility.
Risk vs. Benefit: Healthcare providers must weigh the benefits of brain-targeted treatments against their risks. This is particularly important when considering treatments that may affect cognitive functions or behavior.
7. Integration with Other Therapies
Holistic Approach: Addiction is a multifaceted disorder that involves behavioral, emotional, and social factors. Overemphasizing neurological treatments might lead to neglecting these other essential aspects of recovery. A holistic approach integrating brain-based treatments with behavioral therapies is ethically necessary to ensure comprehensive care.
8. Manipulation and Control
Behavioral Control: Brain-based treatments can potentially exert control over individuals’ cognitive functions and behaviors. While this can help reduce addiction, it raises ethical concerns about the extent to which these treatments influence personal freedoms and autonomy.
Focusing on brain mechanisms to treat addiction offers promising avenues for recovery but comes with significant ethical considerations. Ensuring that treatments respect patient autonomy, privacy, and well-being while addressing broader equity, stigma, and safety concerns is crucial for navigating these dilemmas effectively. Balancing brain-focused interventions with holistic care remains a key priority in ethical addiction treatment.
Frequently Asked Questions
Here are some common questions:
How does addiction affect decision-making?
Addiction weakens the prefrontal cortex, the area responsible for judgment, impulse control, and planning. This makes it harder to resist urges, especially during stress or emotional distress.
What is tolerance, and why does it happen?
Tolerance develops when the brain adapts to repeated exposure to a substance by reducing its response. This leads individuals to use higher amounts to achieve the same effect, increasing overdose risk.
How does withdrawal affect the brain?
During withdrawal, dopamine levels drop, and stress hormones rise. This creates symptoms such as anxiety, irritability, insomnia, and physical discomfort, which strongly drive continued use to relieve distress.
Conclusion
The brain mechanism of addiction is a complex interplay of neural circuits and neurotransmitter systems, which both medications and psychological therapies aim to target for effective treatment. While medications work by altering receptor activity and neurotransmitter levels to mitigate cravings and withdrawal, psychological therapies address cognitive and emotional processes to support behavioral change. Despite their potential benefits, these treatments have disadvantages, such as variability in effectiveness, possible side effects, and high costs. Ethical dilemmas must also be carefully managed, including informed consent, privacy, and stigmatization. A comprehensive and ethically sound approach is essential to address these challenges while providing effective and holistic care for addiction.
Video: The Brain Mechanism Keeping You Addicted #opioids #awareness
This Is Why Therapy Works For Addiction #psychology #brain #addiction