Addiction as a chronic brain disease provides understanding, supports comprehensive treatment, and reduces stigma. However, it also poses challenges, including an over-reliance on medication and ethical concerns about autonomy and medicalization. To address these issues, communities must implement education, integrated care, support networks, and policy advocacy strategies to ensure effective and equitable addiction management.
Understanding Addiction as a Chronic Brain Disease
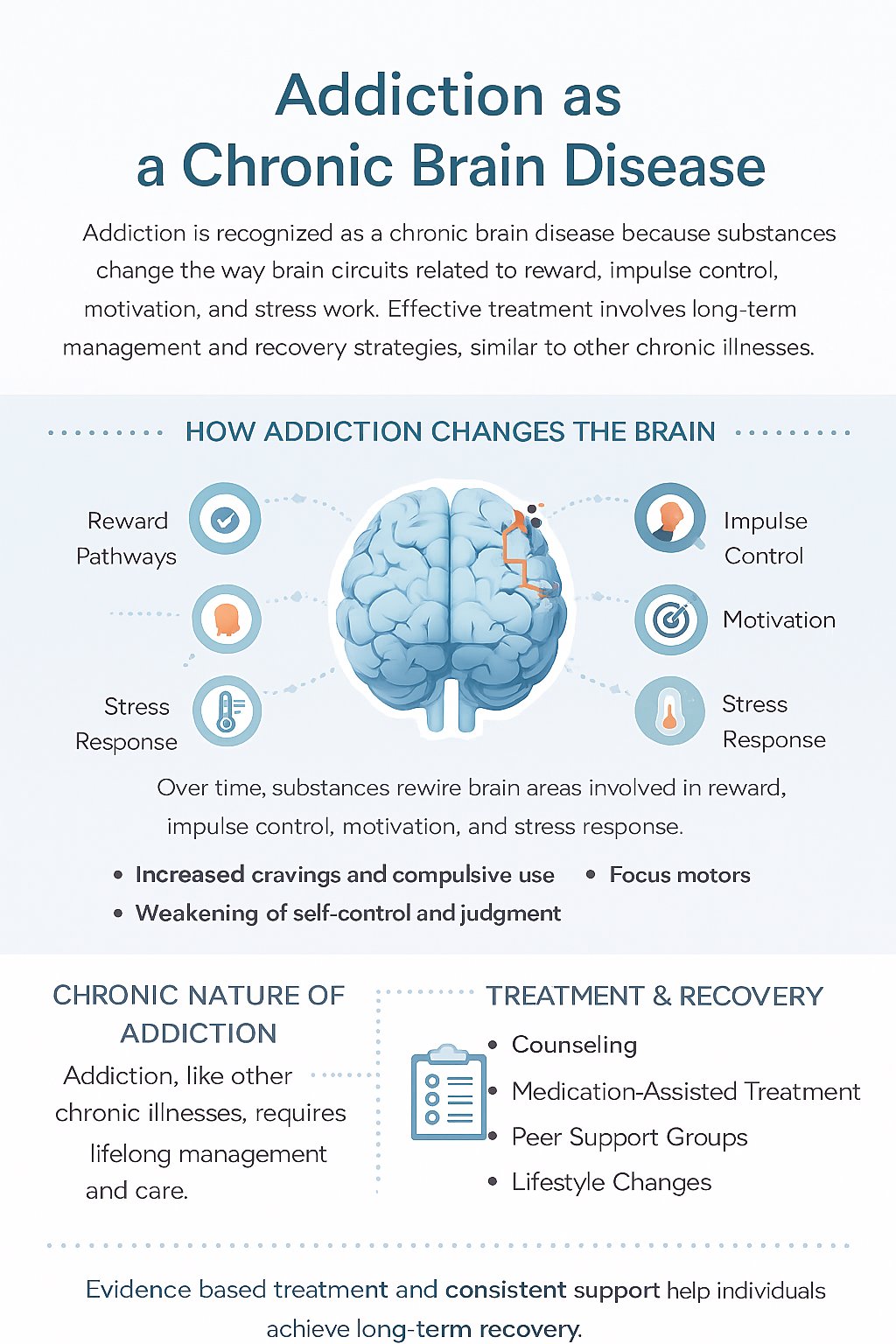
Addiction is now widely identified as a chronic brain disease due to its impact on brain structure and function. Here’s how it is classified as such:
1. Brain Changes
- Neurotransmitter Disruption: Addiction disrupts the brain’s neurotransmitter systems, especially dopamine, affecting reward and pleasure pathways, which drive compulsive behaviors.
- Structural Alterations: Long-term substance use changes brain regions like the prefrontal cortex and limbic system, impairing decision-making, impulse control, and stress response.
2. Chronic Nature
- Long-Term Management: Similar to chronic illnesses like diabetes, addiction requires ongoing treatment and is characterized by cycles of relapse and remission.
- Persistent Behavior: Compulsive drug use persists despite adverse consequences, mirroring symptoms in other chronic diseases.
3. Genetic and Biological Factors
- Genetic Predisposition: Genetics significantly influence addiction risk, with certain genetic variations increasing susceptibility.
- Biological Mechanisms: Addiction affects brain circuitry and stress responses, indicating a biological basis beyond mere willpower.
4. Behavioral Symptoms
- Compulsive Use: Persistent substance use occurs despite knowing the risks, akin to symptoms in other chronic conditions.
- Loss of Control: The inability to regulate drug use reflects how addiction alters brain function.
5. Response to Treatment
- Long-Term Care: Effective management often involves a mix of medication, therapy, and lifestyle changes, emphasizing the chronic nature of the disease.
- Relapse and Remission: The cycle of addiction resembles that of other chronic conditions, requiring symptom management and prevention.
6. Research and Understanding
- Neuroscientific Evidence: Advances in neuroscience have shown how addiction reshapes brain function, supporting the view of it as a brain disease.
- Disease Model: This model aids in understanding the complexity of addiction and informs the development of targeted treatments.
Recognizing addiction as a chronic brain disease shifts the focus from moral judgment to treating it as a medical condition that requires ongoing care, leading to more effective and compassionate recovery approaches.
The Benefits of Treating Addiction as a Chronic Brain Disease
Identifying addiction as a chronic brain disease brings several advantages to treatment, enhancing both effectiveness and compassion. Here are the key benefits:
1. Personalized Treatment Approaches
- Tailored Interventions: Viewing addiction as a brain disease enables treatment plans that target specific neurological and psychological needs.
- Medical Management: This approach supports the use of medications that address brain chemistry, managing symptoms such as withdrawal, cravings, and mental health issues.
2. Increased Access to Evidence-Based Therapies
- Behavioral Therapies: Understanding addiction’s impact on the brain encourages using evidence-based therapies like cognitive-behavioral therapy (CBT) that modify behavior and brain function.
- Integrated Care: Treatment often combines medical, psychological, and social support to address individuals’ complex needs.
3. Enhanced Focus on Long-Term Management
- Chronic Disease Management: Framing addiction as a chronic illness emphasizes ongoing treatment, similar to managing diabetes or hypertension.
- Relapse Prevention: Supports strategies for relapse prevention and continuous care, recognizing that recovery is a lifelong process.
4. Reduction of Stigma
- Medical Perspective: Acknowledging addiction as a brain disease reduces stigma by framing it as a health condition, not a moral failing.
- Compassionate Care: This understanding fosters a more compassionate, empathetic response that supports rather than blames.
5. Improved Patient Engagement
- Understanding the Disease: Patients who see addiction as a brain condition may be more motivated to participate in treatment.
- Motivation and Support: Acknowledging the biological basis increases healthcare providers’ and families’ motivation and support.
6. Advancement of Research and Innovation
- Ongoing Research: Treating addiction as a brain disease fuels research into treatments targeting the neurological mechanisms involved.
- Innovative Therapies: Promotes the development of advanced therapies, such as neuromodulation and personalized medicine.
7. Comprehensive Support Systems
- Integrated Treatment: The chronic disease model encourages addressing both addiction and co-occurring mental health disorders.
- Support Networks: Strengthen support systems such as peer groups, family therapy, and community resources for ongoing recovery.
8. Focus on Prevention
- Early Intervention: Understanding addiction as a chronic condition underscores the importance of early intervention.
- Educational Programs: Support the development of programs to increase awareness and prevent the onset of addiction.
Recognizing addiction as a chronic brain disease shifts treatment to a more effective, compassionate, and individualized approach, promoting better outcomes and long-term recovery.
Challenges of Treating Addiction as a Chronic Brain Disease
While recognizing addiction as a chronic brain disease provides benefits for treatment, it also presents some challenges and potential disadvantages. Here are some of the key concerns:
1. Potential Overemphasis on Medication
- Medication Reliance: Focusing heavily on pharmacological treatments may neglect the importance of behavioral therapies and psychosocial support.
- Limited Focus: This emphasis could overlook social, emotional, and environmental factors that also contribute to addiction.
2. Medicalization of Addiction
- Reduced Personal Agency: Viewing addiction mainly as a brain disease might diminish the role of personal choice and behavioral change in recovery.
- Disease Stigma: Although medicalization can reduce stigma, it may also suggest that individuals are passive victims, affecting their sense of self-efficacy.
3. Risk of Overdiagnosis and Over-Treatment
- Overdiagnosis: The disease model could lead to categorizing ordinary or everyday substance use issues as chronic conditions.
- Over-Treatment: There is a risk of prescribing excessive treatment for individuals who may benefit from less intensive interventions.
4. Healthcare System Limitations
- Access to Care: Not everyone can access comprehensive addiction treatment equally, limiting the model’s effectiveness.
- Resource Constraints: Healthcare systems may face resource limitations, affecting the availability and quality of addiction care.
5. Challenges in Treatment Adherence
- Complex Regimens: Managing addiction as a chronic disease often involves complicated treatment plans that may be hard to follow.
- Long-Term Commitment: The need for continuous treatment and monitoring can be daunting, affecting individuals’ commitment to ongoing care.
6. Risk of Reduced Focus on Holistic Approaches
- Narrow Focus: Emphasizing the brain disease model may limit attention to the broader psychosocial, cultural, and environmental factors in addiction.
- Integrated Care Challenges: Combining biological, psychological, and social treatment aspects can be difficult.
7. Ethical and Social Implications
- Disease Labeling: Labeling addiction as a brain disease can influence how individuals see themselves and how society perceives them, affecting employment and social relationships.
- Insurance and Funding: Insurance coverage for chronic disease management may be limited, affecting treatment availability and affordability.
8. Resistance to Treatment
- Skepticism: Some individuals and providers may prefer alternative approaches emphasizing behavioral and social aspects over the chronic disease model.
- Barriers to Acceptance: The chronic disease label might be hard for some to accept, affecting their willingness to engage in treatment.
Addressing these challenges is essential to ensure a balanced approach that maximizes the benefits of recognizing addiction as a chronic brain disease while mitigating potential drawbacks.
Ethical Dilemmas in Treating Addiction as a Chronic Brain Disease
Identifying addiction as a chronic brain disease offers new treatment perspectives, but it also introduces several ethical dilemmas that need to be considered. Here are some of the key challenges:
1. Autonomy and Agency
- Reduced Personal Responsibility: Framing addiction as a brain disease might downplay the importance of personal responsibility and self-control, potentially affecting individuals’ motivation to engage actively in recovery.
- Informed Consent: The disease model may undermine informed consent and personal agency, as individuals might feel less in control of their recovery.
2. Stigmatization and Labeling
- Disease Labeling: Labeling addiction as a chronic brain disease can lead to stigma or discrimination, impacting individuals’ social and professional lives and affecting their self-esteem.
- Social Perception: It may perpetuate the idea that individuals are “sick” rather than responsible for their behaviors, influencing how they are treated in various contexts.
3. Over-Medicalization
- Medical Focus: There is a risk of over-medicalizing addiction, potentially resulting in an excessive reliance on medications and neglecting other crucial aspects of treatment, such as psychosocial support and lifestyle changes.
- Risk of Over-Treatment: The disease model may lead to overtreatment or inappropriate medical interventions for those who would benefit more from alternative or less-intensive approaches.
4. Equity and Access to Care
- Healthcare Disparities: Identifying addiction as a chronic disease could exacerbate disparities in access to specialized treatment and long-term care, especially for underserved populations.
- Resource Allocation: Focusing on chronic disease management might lead to unequal resource distribution, with some individuals receiving more comprehensive care while others face significant barriers.
5. Long-Term Commitment and Compliance
- Ethical Responsibility: Long-term treatment and monitoring pose ethical questions about healthcare providers’ responsibility to ensure continued adherence and support.
- Patient Burden: Ongoing treatment regimens may create significant burdens, including financial costs and lifestyle demands, raising ethical concerns about fairness.
6. Consent and Autonomy in Treatment
- Informed Decision-Making: It is crucial to ensure individuals fully understand and consent to long-term treatment, but there may be concerns about whether they grasp the full implications.
- Coercion: Ethical issues can arise if individuals feel pressured to follow a specific treatment plan and question whether they are truly consenting.
7. Impact on Social Dynamics
- Family and Social Relationships: The chronic disease model may affect the management of family and social relationships, creating ethical dilemmas regarding support expectations.
- Support Networks: Challenges may emerge in how support networks are involved and whether they are prepared to manage the demands of long-term care.
8. Balance Between Medical and Psychosocial Approaches
- Holistic Care: If the focus on the brain disease overshadows addressing psychosocial, cultural, and environmental factors, ethical dilemmas can arise.
- Integrated Approach: Balancing medical interventions with holistic care that considers the person as a whole presents ethical challenges.
Addressing these ethical dilemmas requires a balanced and thoughtful approach that considers the complexities of addiction treatment, ensuring that care is compassionate and effective.
Community Strategies for Addressing Addiction as a Chronic Brain Disease
To effectively manage addiction as a chronic brain disease, community resource strategies should prioritize comprehensive support, education, and collaboration. Here are some key strategies to consider:
1. Education and Awareness
- Public Education Campaigns: Launch community-wide initiatives to raise awareness about addiction as a chronic brain disease, aiming to reduce stigma and improve understanding.
- Training for Professionals: Equip healthcare providers, educators, and social workers with training on the chronic nature of addiction to ensure consistent, informed care.
2. Access to Integrated Care
- Coordinated Services: Support models of integrated care that combine medical, psychological, and social services, addressing the diverse needs of individuals with addiction.
- Partnerships with Healthcare Providers: Collaborate with local healthcare services to ensure addiction treatment includes a comprehensive, long-term approach.
3. Support Networks and Peer Support
- Support Groups: Promote support groups and peer recovery networks to provide ongoing encouragement, reflecting the lifelong nature of addiction recovery.
- Family Involvement: Offer resources to help families understand the chronic disease model, enabling them to support their loved ones effectively.
4. Prevention and Early Intervention
- Community Prevention Programs: Implement programs that educate at-risk populations about addiction, emphasizing early intervention and prevention.
- Screening and Early Detection: Encourage routine screening and early identification of addiction in primary care settings.
5. Resource Accessibility
- Affordable Treatment Options: Advocate for programs and policies that make treatment affordable and accessible, regardless of socioeconomic status.
- Funding and Grants: Pursue funding to support community-based addiction programs that align with the chronic disease model.
6. Collaborative Community Efforts
- Cross-Sector Collaboration: Foster partnerships across healthcare, education, law enforcement, and social services to create a unified approach to treatment.
- Community Advisory Boards: Form advisory boards that include individuals with lived experience, healthcare experts, and community leaders to guide addiction initiatives.
7. Long-Term Recovery Support
- Sober Living Environments: Develop sober living environments and long-term residential options that acknowledge the ongoing nature of addiction recovery.
- Job Training and Placement: Provide job training and placement services to help individuals reintegrate into the community and maintain recovery.
8. Policy Advocacy
- Advocate for Policies: Support legislation that treats addiction as a chronic disease, ensuring resources are allocated to long-term treatment approaches.
- Legislative Support: Partner with lawmakers to promote policies that reduce barriers to treatment and improve access.
By implementing these community strategies, we can create a supportive environment that acknowledges addiction as a chronic brain disease, offering the resources and support necessary for effective recovery management.
Conclusion
Recognizing addiction as a chronic brain disease offers valuable insights into its treatment and management, emphasizing the need for long-term care and reducing stigma. While this perspective provides advantages, such as more comprehensive treatment approaches, it also presents disadvantages, including the risk of over-medicalization and ethical concerns about autonomy and equity. Effective community resource strategies, including education, integrated care models, and robust support systems, are crucial in addressing these challenges and ensuring that addiction is managed in a way that balances medical and psychosocial needs.
Video: The Shocking Truth About Addiction and Brain Disease Revealed